Mesenteric Vein Thrombosis after Laparoscopic Right Colectomy - A Case Report and Literature Review
Received: 10-Nov-2017 / Accepted Date: 25-Nov-2017 / Published Date: 30-Nov-2017 DOI: 10.4172/2573-542X.1000115
Abstract
Introduction: Mesenteric vein thrombosis (MVT) is a rare but serious condition. Prompt diagnosis and early treatment are essential to avoid high mortality from this condition. Very few cases of this complication after laparoscopic colon resection have been reported in the literature.
Presentation of case: We report superior mesenteric vein thrombosis in a 69-year old male after uneventful laparoscopic right colectomy for colon cancer. Incidental diagnosis of MVT was made on staging CT scan of abdomen one month after surgery. He was promptly treated with anticoagulation which avoided adverse outcomes. The patient was asymptomatic throughout the course of the disease.
Discussion: There is significant lack of its awareness about this disease in medical fraternity due to very low incidence. Additionally, signs and symptoms are often confusing especially in patients who have had recent surgery. Pain abdomen, nausea, and diarrhea are most common symptoms. High degree of clinical suspicion by treating physician is the key to early diagnosis. Undiagnosed patients have high mortality due to consequent mesenteric ischemia and sepsis. CT angiography is the most important diagnostic test and prompt systemic anticoagulation is the treatment of choice.
Conclusion: Awareness of this condition and a high index of suspicion are two most important attributes in fighting with this deadly and rare complication after laparoscopic colon resection.
Keywords: Mesenteric vein; Thrombosis; laparoscopy; Diagnosis
Introduction
Superior mesenteric vein thrombosis (MVT) is a potentially fatal condition without timely treatment. Often there is a delay in the diagnosis due to low clinical suspicion and nonspecific symptoms. The consequences of delay in diagnosis are mesenteric ischemia and potential death. MVT is being increasingly diagnosed due to the frequent use of imaging and advancements in technology. We are reporting a case of mesenteric vein thrombosis in a 69-year-old male one month after laparoscopic right colectomy and presenting a pertinent review of the literature.
Presentation of Case
This work has been reported in line with SCARE criteria. A 69-years old male with past medical history of hypertension, type 2 diabetes, stroke, hypercholesterolemia, and morbid obesity (Body Mass Index 38) presented in a community hospital with symptomatic anemia, hemoglobin 8.9 g/dl. He was diagnosed with advanced carcinoma of cecum during diagnostic colonoscopy. The patient had no history of hypercoagulable state. Apart from anemia, preoperative hemogram was and CEA (2.4 ng/ml) were normal.
CT scan of abdomen and pelvis as part of metastatic workup confirmed large circumferential mass in the cecum with few regional mesocolic lymph nodes. He underwent laparoscopic right hemicolectomy. The procedure took five and half hours due to large body habitus and intra-abdominal adhesions. Standard 14 mm of Hg pressure of pneumoperitoneum was used during the procedure. He was placed on intermittent pneumatic compression stockings intraoperatively. No pre or intraoperative heparin was given. Procedure and the immediate postoperative course were uneventful. The patient received both chemical and mechanical DVT prophylaxis following surgery. Subcutaneous heparin (5000 IU every 8 hours) was initiated 12 hours after surgery. The patient was discharged home on 5th postoperative day.
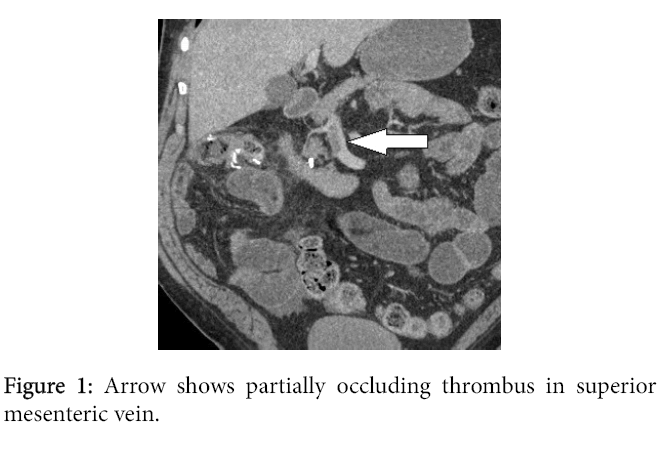
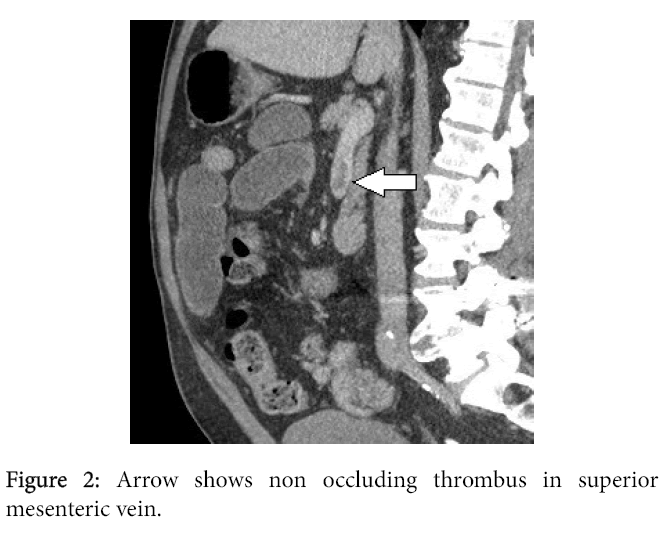
Final histopathology showed invasive adenocarcinoma with mucinous features and 2 out of 24 lymph nodes were positive for metastasis, (pT3 N1b M0). Margins were negative. CT scan of abdomen and pelvis was performed as per oncologist a month after the procedure for staging of the disease. Incidentally, non-occlusive superior mesenteric vein thrombosis was found. The thrombus was clearly seen originating from right colic vein stump and extending into SMV (Superior Mesenteric Vein) for four centimeters with partial occlusion of the lumen (Figure 1 and Figure 2). The portal vein was patent. The patient was completely asymptomatic at that time. He was started on therapeutic enoxaparin and continued on warfarin for 6 months. The patient remained asymptomatic through the entire course.
Review of Literature and Discussion
The incidence of MVT is lower than mesenteric artery thrombosis (MAT).1 MVT accounts for approximately 5-15% of mesenteric ischemic events. It was first recognized as a cause of mesenteric ischemia by Warren [1]. There is a wide range of predisposing factors for this condition. Based on etiology MVT is classified as primary or secondary [2]. When an obvious cause is found, the disease is labeled as primary.3 Currently primary MVT accounts for one-third of cases.4 More cases are falling into the category of secondary MVT as our ability to diagnose causes of MVT improve. Based on chronicity, MVT is also classified as acute, subacute and chronic. Approximately threefourth cases have known etiology [1,3,4]. Factors postulated in Virchow's triad predispose this condition namely venous stasis, hypercoagulability and endothelial injury. Hypercoagulation states are the most common among these [3-5].
Predisposing factors could be systemic or local. Systemic factors include hereditary thrombophilic conditions such as antithrombin III deficiency, protein C and S deficiencies, factor V Leiden deficiency, and various acquired conditions such as sepsis, pregnancy, oral contraceptive use, malignant neoplasm, and myeloproliferative disorders.6 Local factors include direct trauma to portomesenteric vessels, inflammatory process in the vicinity, intra-abdominal malignancies, factors slowing down the mesenteric blood flow such as cirrhosis and direct pressure on veins by ascites and pneumoperitoneum [6].
Portomesenteric venous thrombosis after laparoscopic surgery is an infrequently observed yet a potentially life threatening condition. It is well defined in the literature. Apart from above-mentioned factors, additional locoregional factors may play a role in patients who undergo laparoscopic surgery [6]. The elevated intraabdominal pressure generated by the pneumoperitoneum results in a reduction of portal venous flow. This effect is significantly stronger during carbon dioxide insufflation as compared to inert gases. However, data on the direct effect of capnoperitoneum on coagulation are inconclusive [7-9].
Intra-abdominal blood flow to hollow and solid organs is reduced by 10% to 80% but rapidly normalizes after desufflation of the abdominal cavity. Capnoperitoneum and extreme body positions (35- degree tilt) reduce portal vein blood flow significantly (>30%) [10]. Short desufflation periods does not improve mean portal vein flow [11].
In the current case, several factors may have played a role. Apart from clinical risk factors such as intraabdominal malignancy, morbid obesity, and surgical intervention, and capnoperitoneum may have played a role. Furthermore, we observed that SMV clot was clearly seen originating from the stump of the right colic vein which was not flush ligated. Long blind stump (3 cm) of larger vein (such as right colic) may have been the initiation point of the venous clot which propagated further in favorable circumstances such as low flow state. This could be similar to observation in ligated saphenous vein stumps. Therefore flush ligation of larger veins seems appropriate [12].
The diagnosis of MVT is difficult due to its lower incidence and poorly defined symptomatology. Most patients who undergo colectomy are at risk of MVT due to the primary pathology of the colon such inflammatory conditions (IBD and diverticulitis) and malignancies of the colon [13]. These clinical conditions predispose patients undergoing colectomy to MVT. Additionally, pneumoperitoneum during laparoscopic colectomy creates higher intra-abdominal pressure and venous stasis.
Nature and severity of symptoms depend on the severity of the disease.3 Minor non-occlusive thrombosis of the mesenteric or portal vein may go undiagnosed. On another hand, symptomatic patients have central abdominal pain. Other symptoms include nausea, vomiting, and diarrhoea [4]. Massive portomesenteric thrombosis may cause transmural ischemia of small bowel leading to severe abdominal pain and peritonitis [14]. This is a life threatening condition, early diagnosis is of paramount importance [3]. High clinical suspicion is the key to the diagnosis. The investigation should be directed based on clinical suspicion. Routine blood work often does not provide a clue. Leucocytosis is often present and is nonspecific. Patients presenting with bowel ischemia may have raised serum lactate [3,4].
Cross sectional imaging is the most important test to diagnose this condition, it also guides the management. CTA (CT angiography) and MRA (Magnetic Resonance Angiography) are highly accurate vascular imaging modalities with high sensitivity and specificity for evaluation of the mesenteric vasculature [15]. These imaging modalities have virtually replaced reference standard DSA (Digital Subtraction Angiography).15 Isolated MVT with no portal vein thrombosis is more difficult to diagnose on CT with only 67% sensitivity. Mesenteric angiography or DSA is considered gold standard test but is invasive, resource intensive and often unnecessary [3]. CTA, and MRA may also reveal evidence of bowel ischemia however difficult unless pneumatosis or frank perforation of bowel has already occurred [4].
Once the diagnosis is confirmed, systemic anticoagulation should be started.4 It has shown to improve survival and reduce the risk of recurrence [4]. Supportive measures include nasogastric suction, fluid resuscitation, and bowel rest [3,16]. Further treatment is based on the extent of thrombosis and associated bowel ischemia [16]. Transmural ischemia of small bowel needs immediate surgical resection of involved segment. If the extensive length of bowel is involved with patches of ischemia, resection of clearly ischemic bowel and observation of doubtful area with a second look within 24-48 hours is appropriate. This is the desirable approach in order to preserve as much length of the small bowel as possible to avoid short bowel syndrome [16]. Intraoperative thrombectomy has been defined in literature for acute severe MVT with imminent bowel ischemia [17]. On another hand, the role of thrombolysis is controversial. The trans catheter thrombolysis via the percutaneous trans hepatic or trans jugular intrahepatic route, or indirectly via superior mesenteric artery access are among other treatment modalities suggested, albeit with higher risk of bleeding. The mortality rate among patients with acute mesenteric venous thrombosis ranges from 20 to 50%. [14,16,18].
Through literature search, we could only find only two cases of MVT after laparoscopic colectomy. Two larger series reported MVT after colectomy for IBD. In the current case, we encountered nonocclusive superior MVT [18,19]. It was diagnosed incidentally and had no clinical suspicion of mesenteric ischemia. Outpatient treatment with systemic anticoagulation was deemed appropriate. More cases of SMVT are diagnosed due to improvement and availability of diagnostic tests such as CTA. Therefore, awareness of this entity and its treatment options is essential in clinical practice.
Conclusion
Mesenteric vein thrombosis is a potentially lethal disease. It is rare after laparoscopic colectomy. Therefore clinician’s awareness of this condition is crucial in early diagnosis and timely management. CT angiography is the diagnostic test of choice. It may also provide information about bowel ischemia. Prompt treatment with systemic anticoagulation is the cornerstone of treatment. Surgical intervention usually is limited to resection of ischemic bowel. Other invasive modalities including catheter directed thrombolysis and embolectomy are useful in rare cases. MVT should be considered as one of the differential diagnoses in patients with recent laparoscopic colectomy who have postoperative abdominal symptoms.
References
- Clair DG, Beach JM (2016) Mesenteric ischemia. N Engl J Med 37410: 959-968.
- Warren S, Eberhard TP (1935) Mesenteric venous thrombosis. Surg Gynecol Obstet 61:102-121
- Kumar S, Sarr MG, Kamath PS (2001) Mesenteric venous thrombosis. N Engl J Med 345: 1683-1688.
- Hmoud B, Singal AK, Kamath PS (2014) Mesenteric venous thrombosis. J Clin Exp Hepatol 4: 257-263.
- Byrnes JR, Wolberg AS (2017) New findings on venous thrombogenesis. Hämostaseologie 37: 25-35.
- James AW, Rabl C, Westphalen AC, Fogarty PF, Posselt AM, et al. (2009) Portomesenteric venous thrombosis after laparoscopic surgery: A systematic literature review. Arch Surg 144: 520-526.
- Schmandra TC, Kim ZG, Gutt CN (2001) Effect of insufflation gas and intraabdominal pressure on portal venous flow during pneumoperitoneum in the rat. Surg Endosc 15: 405-408.
- Lindberg F, Rasmussen I, Siegbahn A, Bergqvist D (2000) Coagulation activation after laparoscopic cholecystectomy in spite of thromboembolism prophylaxis. Surg Endosc 14: 858-861.
- Larsen JF, Ejstrud P, Svendsen F, Redke F, Pedersen V, et al. (2001) Randomized study of coagulation and fibrinolysis during and after gasless and conventional laparoscopic cholecystectomy. Br J Surg 88: 1001-1005.
- arsen JF, Ejstrud P, Svendsen F, Redke F, Pedersen V, et al. (2001) Randomized study of coagulation and fibrinolysis during and after gasless and conventional laparoscopic cholecystectomy. Br J Surg 88: 1001-1005.
- Schafer M, Krahenbuhl L (2001) Effect of laparoscopy on intra-abdominal blood flow. Surgery 129: 385-389.
- Schmedt CG, Heupel O, Riemer V, Gutt CN, Büchler MW (2003) Insufflation profile and body position influence portal venous blood flow during pneumoperitoneum. Surg Endosc 17: 1951-1957.
- Rikimaru H (2016) Thrombosis of the saphenous vein stump after varicose vein surgery. Ann Vasc Dis 9: 188-192.
- Zhang J, Duan ZQ, Song QB, Luo YW, Xin SJ, et al. (2004) Acute mesenteric venous thrombosis: a better outcome achieved through improved imaging techniques and a changed policy of clinical management. Eur J Vasc Endovasc Surg 28: 329-334.
- Rhee RY, Gloviczki P, Mendonca CT, Petterson TM, Serry RD, et al. (1994) Mesenteric venous thrombosis: still a lethal disease in the 1990s. J Vasc Surg 20: 688-697.
- Van Dijk LJ, Van Petersen AS, Moelker A (2017) Vascular imaging of the mesenteric vasculature. Best Pract Res Clin Gastroenterol 31: 3-14.
- Inahara T (1971) Acute superior mesenteric venous thrombosis: Treatment by thrombectomy. Ann Surg 174: 956-961.
- Bala M, Kashuk J, Moore EE, Kluger Y, Biffl W, et al. (2017) Acute mesenteric ischemia: Guidelines of the World Society of Emergency Surgery. World J Emerg Surg 12: 38.
- Poultsides GA, Lewis WC, Robert F, Walters DL, Cherry DA, et al. (2005) Portal vein thrombosis after laparoscopic colectomy: thrombolytic therapy via the superior mesenteric vein. Am Surg 71: 856-860.
Citation: Ramesh K, Namrata C (2017) Mesenteric Vein Thrombosis after Laparoscopic Right Colectomy-A Case Report and Literature Review. Cancer Surg (Los Angeles, Calif.) 3: 115. DOI: 10.4172/2573-542X.1000115
Copyright: © 2017 Ramesh K, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7403
- [From(publication date): 0-2017 - Sep 23, 2025]
- Breakdown by view type
- HTML page views: 6342
- PDF downloads: 1061