Metastatic Choriocarcinoma of the Kidney in Absence of Existing Primary Uterine Tumour: A Rare Presentation
Received: 07-Dec-2020 / Accepted Date: 21-Dec-2020 / Published Date: 28-Dec-2020 DOI: 10.4172/2476-2024.S1.002
Abstract
Gestational choriocarcinomas are malignant neoplasms generally arising in the uterus in women of child bearing age. These are aggressive tumours with high incidence of metastasis to vascular organs like lung, liver and brain. Renal metastasis is extremely rare with low incidence rate and very few cases reported in literature. Hereby, we report a rare case of metastatic choriocarcinoma to the kidney in a 29 year old female 10 years after resection of a Hydatidiform mole. The histopathological diagnosis was made on a nephrectomy specimen. Pelvic and abdominal scan did not show any abnormal radiological findings. She was started on first line chemotherapy and showed complete response. In conclusion, gestational or primary non-gestational choriocarcinomas should always be considered as a differential diagnosis in young females of reproductive age group presenting with flank abdominal pain, unexplained hematuria and atypical renal tumour histology.
Keywords: Gestational choriocarcinoma; Hyaditidiform mole; Metastasis; Chemotherapy
Introduction
Gestational Trophoblastic Neoplasms (GTNs) are a rare group of gestational trophoblastic diseases (GTD) which arise from abnormal proliferation of trophoblasts. GTNs comprise of invasive mole, choriocarcinomas, placental site trophoblastic tumours and epithelioid trophoblastic tumours [1,2]. Choriocarcinoma is a malignant trophoblastic neoplasm composed of cytotrophoblasts and syncytiotrophoblasts with propensity for invasion into the endometrium, myometrium and nearby blood vessels. It is characterized by a distribution in midline structures and frequent metastases via hematogenous route [1]. The most common sites of involvement being lungs (80%), vagina (30%), liver (10%) and brain (10%) [2,3]. About 50% of choriocarcinomas develop as a complication of antecedent molar pregnancy or subsequent to a history of tubal pregnancy, miscarriage and older maternal age [4,5].
Here, we report a case of metastatic choriocarcinoma in unilateral kidney and lung arising 10 years after evacuation of complete hydatidiform mole.
Case Report
A 29 year old female presented with complaints of abdominal pain since one year, exacerbated since 15 days. No other significant medical or surgical history was noted. On evaluation, patient was found to have a right renal mass. Positron Emission Tomography and Computed Tomography (PET-CT ) showed 6.5 × 5.9 cm metabolically active soft tissue lesion in the mid pole region of right kidney abutting the duodenum and liver. Renal vein and inferior vena cava was normal. Left lung lower lobe showed a metabolically active necrotic soft tissue mass lesion measuring 4.9 × 3.3 cm. A clinical diagnosis of advanced renal cell carcinoma was made. Transbronchial biopsy of the lung lesion was inadequate with presence of extensive haemorrhage fibrin and scanty viable tissue suggesting poorly differentiated carcinoma, which was not amenable to ancillary tests. Further, patient underwent segmentectomy of lung lesion with right radical nephrectomy. Intraoperatively, kidney showed bleeding into the retroperitoneum with 1 litre hematoma within gerota’s fascia.
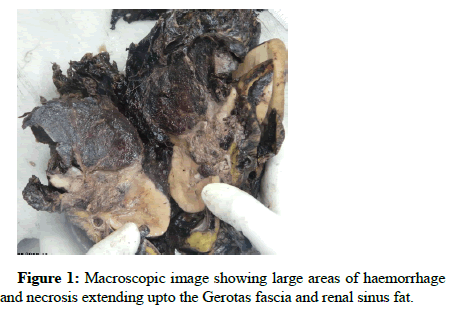
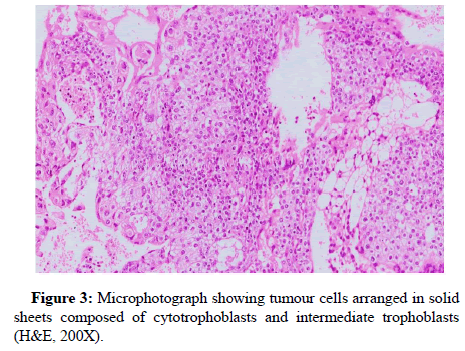
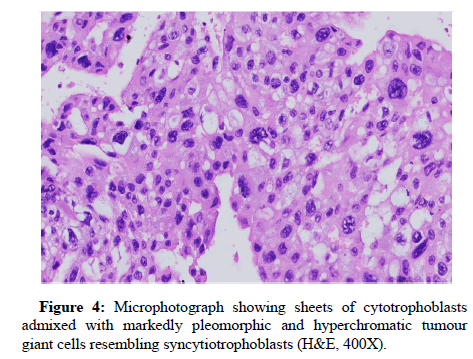
On gross examination, right kidney showed a large grey brown to black tumour with extensive areas of haemorrhage and necrosis extending into the perinephric fat and Gerota’s fascia (Figure 1). Renal sinus fat invasion was seen. Microscopic examination of both lung and renal lesion showed large areas of central haemorrhage and fibrinous exudate surrounded by a diffusely infiltrative neoplasm (Figures 2a and 2b). The neoplastic cells were seen forming syncytium and sheets, composed of large polygonal cells with moderate eosinophilic to clear cytoplasm resembling cytotrophoblasts. These cells were rimmed by multinucleate cells resembling syncytiotrophoblasts (Figures 3 and 4). Extensive areas of perinephric haemorrhage and necrosis was noted. Multiple lymphovascular emboli were present.
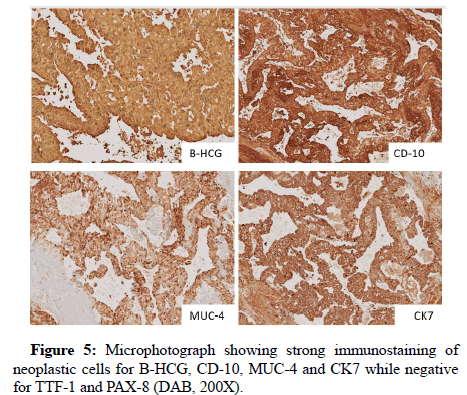
Immunohistochemistry showed strong immunoexpression for Ck, Ck7, Beta-HCG, MUC-4 and CD10 (Figure 5) while negative for PAX-8 and TTF-1. Post-op Beta-HCG level was markedly elevated with a value of 12585 mIU/ml. In view of the above findings, patient’s gynaecological medical records were re-evaluated. She had a past history of dilatation and curettage for H mole in 2010. However, radiological findings did not reveal lesion in any other pelvic or abdominal organs.
A final diagnosis of metastatic choriocarcinoma involving right kidney and left lung upper lobe without a detectable primary foci was made. The patient was started on EMA-CO chemotherapy regime. She tolerated the treatment well and showed normalization of Beta-HCG levels. No metastatic lesions were noted at 6 months follow-up.
Discussion
Choriocarcinomas are highly malignant epithelial neoplasms which are classified as gestational and non-gestational [6]. Gestational choriocarcinoma are more common and includes cases of primary uterine origin with or without metastasis. It is the most aggressive and most common gestational trophoblastic disease contributing to 1 in 2500 pregnancies in Asia and Africa [4,5]. Half of the gestational choriocarcinomas have a prior incidence of molar pregnancy while it can also occur in association with normal pregnancy (25%) or spontaneous abortion (25%) [5,6]. According to literature, median interval between a preceding molar pregnancy and development of choriocarcinomas has been reported around 36.5 months [5] while Hui P reported an average of 13 months [7]. Due to high vascularity of trophoblastic tumours, the most common symptom of GCs is irregular uterine bleeding. However in patients with extrauterine spread extrauterine haemorrhage may be the first presenting symptom [7].
Non gestational choriocarcinomas are extremely rare and very few cases have been reported in literature [4]. These tumours are almost always seen as component of mixed germ cell tumours or mixed tumour of the endometrium in post-menopausal women [7]. Thus, extensive search for non choriocarcinomatous component should always be made before making a diagnosis of primary extrauterine non gestational choriocarcinoma [4,6,7]. Compared to gestational choriocarcinomas, these tumours are often chemotherapy resistant and associated with worse prognosis [6,8].
With the advent of successful chemotherapy regime, very few cases of metastatic choriocarcinoma have been reported. Incidence of metastatic choriocarcinomas after evacuation of complete mole is reported to be about 4%-5% by Thomakos et al. [6] Lung metastasis has been reported in more than 90% of patients with gestational choriocarcinomas [6].
Renal metastasis is extremely rare. Incidence of renal metastasis has been reported to be around 12%, while 48% cases have been found in autopsy [9,10]. However, in our case metastasis to the kidney without detectable primary can be related to the ‘burned out’ hypothesis. It is a phenomenon described as metastasis to extrauterine sites from a spontaneously regressed primary lesion in the uterus [5].
On histology, choriocarcinomas are diffusely infiltrating neoplasms with a destructive growth pattern invading the deep endomyometrium [7]. A classical biphasic pattern has been observed with alternating arrangement of cytotrophoblasts and syncytiotrophoblasts separated by intermediate trophoblasts. Large areas of central haemorrhage with necrosis are seen.
Choriocarcinomas are characterised by raised serum Beta-HCG values. The levels of serum Beta-HCG correlate with tumour mass and higher levels indicate tumour progression [6]. GTNs have been reported to have a high cure rate with methotrexate based chemotherapy regime even in metastasised choriocarcinomas [5]. The commonly used regimes include EMA-CO (Etoposide, Methotrexate, Actinomycin D, Cyclophosphamide, and Vincristine), MEA (methotrexate-etoposide-actinomycin D) or EP/EMA. EMA-CO chemotherapy regimen has shown complete response rates of 71%-78% and long term survival rates of 85%-94% [3,11-14].
Conclusion
Metastatic choriocarcinoma of the kidney is a rare entity and should be considered as a differential diagnoses in young females with history of GTDs presenting with flank abdominal pain or refractory hematuria. Serum Beta-HCG levels are required to confirm the diagnosis. Choriocarcinomas are highly curable neoplasms with a very high response rate of over 90% to chemotherapy. Hence, an early and preoperative diagnosis of choriocarcinoma is necessary to avoid the high risk of morbidity and mortality associated with surgery and to avoid complications such as hyperemesis gravidarum, massive haemorrhage, infiltration into other organs and perforation of viscera.
Source of Funding
None
Conflict of Interest
None
References
- Yen CC, Tsai HW, Yen CJ (2019) Postmolar metastatic choriocarcinoma mimicking primary lung cancer. J Cancer Res Pract 6: 41.
- Ahamed NA, Sait K, Anfnan N, Farwan K, Nizamuddin SH, et al. (2015) Gestational choriocarcinoma presenting with lacrimal gland metastasis: A first reported case. Obstet Gynecol Cases Rev 2015.
- Thomakos N, Rodolakis A, Belitsos P, Zagouri F, Chatzinikolaou I, et al. (2010) Gestational trophoblastic neoplasia with retroperitoneal metastases: A fatal complication. World J Surg Oncol 8: 1-6.
- Salako AA, Olajide AO, Takure AO, Sabageh D, Arowolo OA (2011) Metastatic choriocarcinoma presenting as advanced renal cell carcinoma: A case report. Trop J Obstet Gynaecol 28: 70-73.
- Iijima Y, Akiyama H, Nakajima Y, Kinoshita H, Mikami I, et al. (2016) Solitary lung metastasis from gestational choriocarcinoma resected six years after hydatidiform mole: A case report. Int J Surg Case Rep 28: 231-233.
- Yamamoto E (2009) Solid tumor section. Atlas Genet Cytogenet Oncol Haematol 13: 683-685.
- Hui P (2019) Gestational trophoblastic tumors: A timely review of diagnostic pathology. Arch Pathol Lab Med 143: 65-74.
- Mack RB, Katz SM, Amenta PS (1992) Choriocarcinoma of the kidney. J Am Osteopath Assoc 92: 799-802.
- Ikeda I, Miura T, Kondo I, Kimura A (1996) Metastatic choriocarcinoma of the kidney discovered by refractory hematuria. Acta Urol Jpn 42: 447-449.
- Kutcher R, Lu TH, Gordon DH, Becker JA (1977) Renal choriocarcinoma metastasis: A vascular lesion. Am J Roentgenol 128: 1046-1048.
- Kyriakou F, Vaslamatzis MM, Bastani S, Lianou MA, Vourlakou C, et al. (2011) Primary choriocarcinoma of the renal pelvis presenting as intracerebral hemorrhage: A case report and review of the literature. J Med Case Rep 5: 1-4.
- Li HM, Hou WC, Lai YJ, Kao CC, Chao TK, et al. (2016) Gestational choriocarcinoma with renal and pulmonary metastases lacking a primary uterine origin. Taiwan J Obstet Gynecol 55: 881-885.
- Devasia A, Nath V, Abraham B, Gopalkrishnan G, Nair S (1994) Hematuria, renal mass and amenorrhea: Indicators of a rare diagnosis. J Urol 151: 409-410.
- Katke RD (2015) Atypical presentation of uterine choriocarcinoma: A case report with review of literature. Clin Cancer Investig J 4: 713.
Citation: Pahwa S, Anila S, Meenakshi K, Gurudutt G, Sunil P (2020) Metastatic Choriocarcinoma of the Kidney in Absence of Existing Primary Uterine Tumour: A Rare Presentation. Diagn Pathol Open S1: 002. DOI: 10.4172/2476-2024.S1.002
Copyright: © 2020 Pahwa S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 2786
- [From(publication date): 0-2020 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 1932
- PDF downloads: 854