Research Article Open Access
Microvascular Reconstruction in the Revascularised Diabetic Foot: A Perforosome Approach
Thalaivirithan Margabandu Balakrishnan1* and Paramasivam Ilayakumar2
1Department of plastic faciomaxillary and reconstructive surgery, Madras Medical College, Rajiv Gandhi Government General Hospital, Chennai, India
2Department of vascular surgery, Madras Medical College, Rajiv Gandhi Government General Hospital, Chennai, India
- *Corresponding Author:
- Balakrishnan TM
old no 15, New no 10, Thiruvalluvar Street
Rangarajapuram, Kodambakkam
Chennai -24, Pin: 600024, India
Tel: 9841194221
E-mail: thalaiviri.b@gmail.com
Received Date: September 12, 2016; Accepted Date: September 21, 2016 ; Published Date: September 28, 2016
Citation: Balakrishnan TM, Ilayakumar P (2016) Microvascular Reconstruction in the Revascularised Diabetic Foot: A Perforosome Approach. Clin Res Foot Ankle 4:206. doi:10.4172/2329-910X.1000206
Copyright: © 2016 Balakrishnan TM, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Clinical Research on Foot & Ankle
Abstract
Background and Introduction: Now there is increasing occurrence of diabetic foot with ongoing epidemic of diabetes mellitus throughout the world. Considerably there is also increase in the critically ischemic diabetic foot which requires timely recognition, timely revascularization and last but not the least timely reconstruction. In this article author describes his perforosomal approach for the microvascular reconstruction in the revascularised diabetic foot. This thoughtful applied anatomical approach is pursued right from the recognition of critical ischemia. It begins with assessment of perforosomes involved by ischemia and subsequently perforosomal directed distal revascularization (PDDR) and then perforosome directed reconstruction. Plastic surgeon coordinates with interventional radiologists or vascular surgeon to pursue direct distal revascularization of all involved perforosomes. Finally this culminated in the perforosomal approach for the reconstruction, which results in shoeable and stable foot or foot residuum in all cases. Altered vasohemodynamics peculiar to the revascularised diabetic foot called “Regional vascular insufficiency” (RVI) also discussed in this article. Aim: Aim of the study is to discern how effective is the microvascular reconstruction (MVR) in healing the recipient site in neuroischemic diabetic foot affected by RVI. Also how effective is PDDR in bringing the healing potential in the ischemia-affected perforosomes of foot. To analyze the complications related to PDDR and MVR. Materials and Method: This is prospective cohort study with level II evidence conducted with 50 (age 44 to 68and M: F ratio 40:10) critically ischemic diabetic foot patients (ABI <or= 0.7) with no healing potential. All had undergone PDDR followed by microvascular reconstruction during March 2011 to March 2016. All patients were followed for on average period of 18 months post reconstruction. The outcomes were analyzed in terms of, averagelatency period (between the revascularization and reconstruction contributed by regional vascular insufficiency) as a measure of effectiveness of PDDR, and then factors like ambulation capabilities attained, length of hospital stay and rate of recurrence of ulcers as the measure of effectiveness of microvascular reconstruction (MVR). All patients also underwent many adjuvant procedures (internal offloading) as an integral part of MVR. Complications related to PDDR and MVR are also analyzed. Results: Fifty patients admitted with critically ischemic diabetic foot were included this study based on the selection criteria. Descriptive and life table statistical analysis is used in this study. All of them undergone PDDR (46 had angioplasty; 2 had angioplasty and bypass-hybrid procedure; 2 had bypass alone down to foot). No patients in angioplasty group had any procedural complication except in one case in the hybrid group and one in angioplasty group had transient renal parameters rise. One in distal bypass group had bypass wound infection treated surgically and recovered. One perforator/propeller suffered partial epidermolysis treated conservatively. The average Latency period in the bypass group is 28 days, hybrid procedure group is 28.5 days and angioplasty group is 18.5 days. Results are stratified in to 4 groups. In group one (above hip perforosome – thoraco dorsal artery muscle perforosome (TDAP), thirty one patients had MVR with latissimus dorsi thoracodorsal artery muscle perforosome with split thickness skin graft. In this group there is 2 cases of arterial insuffiency successfully revised on 1st POD. There was no other complication in this group. In Group two (above hip perforosome-radial forearm arm flap), six patients had MVR with radial forearm flap. No complications occurred in this group. In-group three (below hip disease free perforosome reconstruction), four patients had MVR with vastus lateralis perforator flap as the angiogram revealed healthy profunda femoris vessels in these cases. One case in this group required revision for venous insuffiency with vein graft on the 1st POD and flap salvaged successfully. Other three patients of this group had MVR with free Gracilis flap and one patient received contralateral medial plantar artery perforosome. Dorsum defect (1 case) and great toe stump raw area (4 cases) are treated by arcuate artery perforator flap and first dorsal artery perforator flap respectively in the fourth group (Perforator/propeller flaps group). All MVR flaps survived in this group except one case there was superficial epidermolysis. In the post PDDR phase 36 cases had calcaneal raw area (perforosomes supplied by calcaneal branch of peroneal and posterior tibial vessels are involved) and all are treated by latissimus dorsi thoracodorsal vessel muscle perforosome with skin graft. It took 2.5 months on average to assume bipedal walking in this group. Forefoot raw area was present in the post PDDR phase in 11 cases. It took 2 months on average for these patients to assume bipedal walking. One case of modified pirograffs amputation stump raw area had undergone after PDDR, MVR with vastus lateralis perforator flap. This patient assumed bipedal walking with prosthesis on 70th postoperative day. All perforator flaps resumed bipedal walking on average 26 days from the time of MVR. Only one case of Lattisimus dorsi required thinning performed at 60th postoperative day and this patient started bipedal ambulation on 4th month following MVR. There was no periprocedural mortality in this study. Flap survival rate is 100% in our study. Overall recurrence ulceration rate is 6%.
Discussion: When compared to available other similar related studies author had better results in terms of duration of hospital stay and period after MVR before assuming bipedal ambulation and less latency periods because of PDDR and subsequently with perforosomal approach of MVR. Ulcer recurrence rate is also comparable to other related studies.
Conclusion: This perforosomal approach makes a definitive difference in salvaging the critically ischemic diabetic foot.
Keywords
Perforosome approach; Microvascular reconstruction; Salvaging diabetic foot; Critically ischemic diabetic foot; Regional vascular insufficiency; Perforosome directed distal revascularization; Perforosome directed reconstruction
Introduction
India was declared as “world capital for diabetes mellitus” with 69.1 million diabetic patients (source International Diabetic Federation 2015 data). Despite efforts by various health departments all over the world the epidemic of this non-communicable disease is sadly going unabated.
Around 422 million people are affected by diabetes mellitus in the world (source NCD Risk factor collaboration 2016).
Therefore the complications related to this systemic disease also going on escalating. Diabetic foot is one such important complication. 59% of our diabetic population during their life develops at least onefoot complication (MMC on going study).
The morbidity and mortality produced by the diabetic foot ulcers are significant and comparable to that of breast cancer as shown by the studies in United States [1]. Also it has been felt by all the surgeons working in the podiatry that there was paradigm shift from previously common neuropathic diabetic foot ulcers to neuroischemic diabetic foot ulcers, which now constitutes little over 50% [2]. So it is imperative that timely recognition of critically ischemic diabetic foot is necessary. Once recognized timely revascularization followed by reconstruction should culminate in the shoeable and stable foot or foot residuum.
Author in this article discusses briefly the newer concepts like perforosome, regional vascular insufficiency (RVI), perforosome directed distal revascularization (PDDR) and then finally the study details are presented. It is hoped that this article will help contemporary alert surgeon to embark on this challenging task of salvaging the critically ischemic diabetic foot.
Perforosome Concept
Ever since Isao Koshima [3] introduced the perforator concept, there is burgeoning interest in this interesting applied anatomical field. Author defines the perforosome as “a vaso neuro osteo histo surgical unit supplied by the single perforator vessels arising from the source vessel”.
It is further distilled extension knowledge of understanding of the angiosomal concept introduced by Ian Taylor [4]. Angiosome is vasoneuro-histosurgical unit supplied by the single source vessel.
Many perforosomes fit in to each other like a jig saw puzzle pieces to form the angiosomes. In turn many angiosomes form the part of the human body.
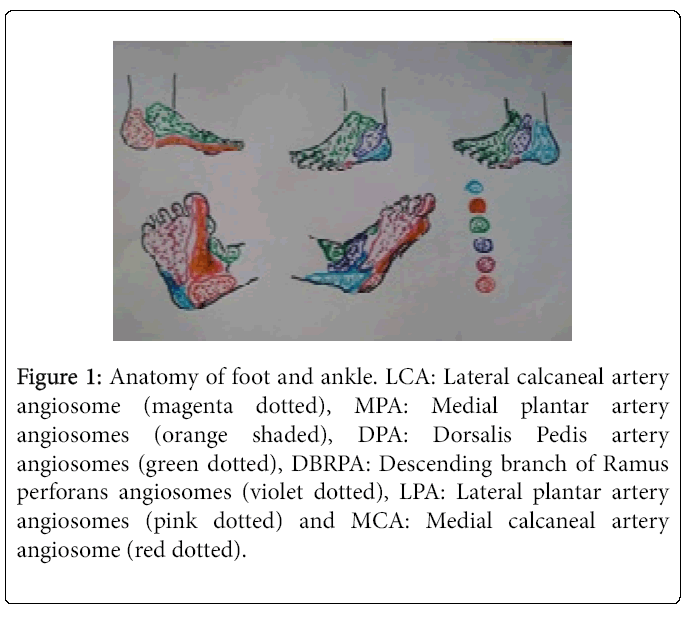
Author look at the anatomy of foot and ankle as the interdigitation six different angiosomes and each supplied by one source vessel as shown in the (Figure 1).
Figure 1: Anatomy of foot and ankle. LCA: Lateral calcaneal artery angiosome (magenta dotted), MPA: Medial plantar artery angiosomes (orange shaded), DPA: Dorsalis Pedis artery angiosomes (green dotted), DBRPA: Descending branch of Ramus perforans angiosomes (violet dotted), LPA: Lateral plantar artery angiosomes (pink dotted) and MCA: Medial calcaneal artery angiosome (red dotted).
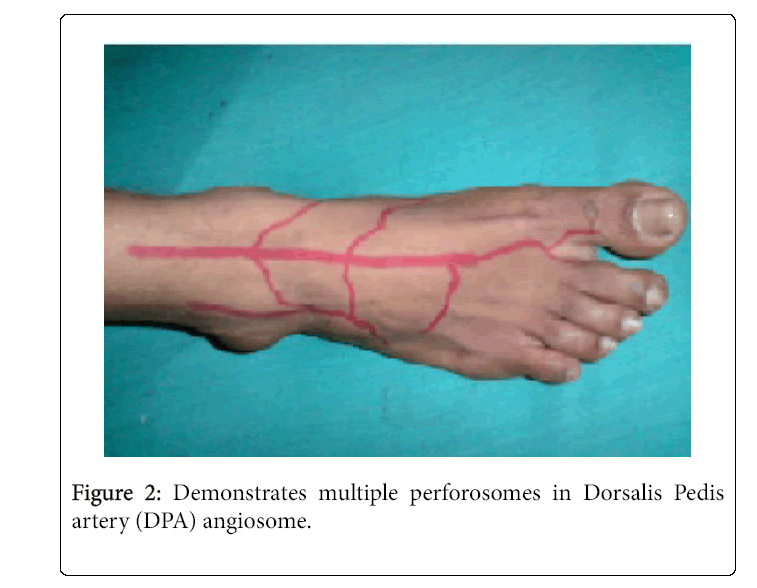
In Figure 2 Dorsalis Pedis artery has got many perforosomes arising from the Dorsalis Pedis artery like medial tarsal artery perforosomes, lateral tarsal artery perforosomes, medial malleolar and lateral malleolar perforosomes, first dorsal artery perforosomes arcuate artery perforosomes and proper dorsal artery perforosomes.
Perforosome Directed Distal Direct Revascularisation (PDDR)
After the advent of thin balloons and guide wires and combination of anterograde and retrograde puncture techniques by the interventional radiologists the perforosome directed distal direct revascularization has become a reality after 2009; also the vascular surgeons realized the importance of direct revascularization of the perforosome involved by the ischemic ulcer or gangrene.
The study done by Neville et al. [5] brought the importance of angiosome directed distal direct revascularization.
This kind of intervention has shown to decrease the major limb amputation by four fold and increase the healing rate by 50%. Author’s intervention is a corollary extension of this same concept.
Here the angiosome concept is further refined by the perforosomal concept as the diabetic peripheral arterial disease although can involve any infra inguinal vessels but peculiarly involves the cluster of perforosomes distally in foot and ankle where ischemic ulcers or gangrene occurs.
Patients with ABI less than or equal to 0.7 and wound showing no granulation which is the emblem of wound healing potential-these two are the main selection criteria apart from others used by the authors for taking the patient for PDDR.
Patients with highly calcified infra genual vessels with physical fitness for anesthesia are taken for bypass or hybrid procedure with earnest efforts to revascularise distally and directly the involved perforosomes.
Others are subjected to angioplasty alone again with PDDR approach. It is beyond the scope of this article to discuss the specific indications for the open surgery and minimally invasive angioplasty procedure.
Author as the orchestrating member of the multispecialty integrated approach this PDDR was done in all 50 patients with critically ischemic diabetic foot and subsequently taken up for the microvascular reconstruction.
Regional Vascular Insuffiency (RVI)
This is a pathophysiological state in the post revascularization scenario where there is failure of wound healing due to perfusion deficiency attributed by diabetic functional micro angiopathy in the presence of good macro vascular blood flow.
So it is lingering perfusion failure despite reestablished adequate blood flow. No structural abnormalities made out in the microcirculation of diabetic foot so far. But the peculiar regional abnormality that is made out in the neuroischemic diabetic foot is failure of the capillaries to dilate and to undergo compensatory hyperplasia in the face of normal oxygen gradient from depth of wound to surface.
In addition to this there is hemorrheological abnormalities of leukocytes and serum proteins. Red blood cells are also stiff in diabetic due to non-enzymatic glycation of spectrin a trans membrane protein.
As a result of this stiff RBCs do not stack one over the other at the arteriolar end of capillaries which normally happens during entry of red blood cells in to the four micrometer diameter arteriolar end of microcirculation. Super imposition of this systemic factors (hemorrheological abnormality) on the regional factor (functional microangiopathy) is the cause for failure of proliferation of fibro capillary network-“the organ of repair”.
So there is continued wound healing failure due to transient perfusion failure despite successful PDDR found in all cases for varying period.
So there is no granulation appear for variable period despite the PDDR, which renders palpable vessels in the vicinity. But this improves with balanced debridements and with special active dressing after PDDR.
When the granulation-the emblem of wound healing potential begins to appear in the wound patient is taken up immediately for definitive reconstruction.
This RVI is the main reason for the latency period between the revascularization and definitive reconstruction. Surgeon at the same time restrict his debridement only to obviously infected tissues as all neuropathic ischemic tissues do not manifest classical signs of inflammation and at the same time un restrained excision will lead to loss of all potentially salvageable tissues.
Reinforced with tissue saving approach author directs whole team for the ultimate aim of obtaining the shoe able and stable foot or residuum of foot with no recidivism.
All ischemic tissues are more prone for exposure desiccation and devitalization sequence. So reconstructive surgeon must balance this factor against the maturation of regional vascular insufficiency following revascularization and seize the early opportunity of reconstruction with technique that brings in well-vascularized tissues to recipient site.
These regional vascular insufficiency areas are also incapable of mounting inflammatory or immune response to surgical trauma and therefore diabetic wounds are staggered in smoldering inflammatory phase of wound healing with inherent delay.
Microvascular tissue transfer and especially the perforosomes replacement (with its supra normal blood supply) [6] for perforosomes in neuroischemic diabetic foot in authors experience solve well all these problems.
Study Period
March 2011 to March 2016.
Materials and Method
This is prospective cohort study with level II evidence conducted with 50 (age 44 to 68 and M: F ratio 40:10) critically ischemic diabetic foot patients (ABI <or= 0.7) with no healing potential.
Inclusion Criteria
Diabetic patients with ischemic ulcers with no healing potential or patients with gangrene limited to toes or clustered perforosomes and also with ABI less than or equal to 0.7 are selected for this study.
All patients with post angiogram pathology discerned with need for immediate revascularization are only included in the study.
Exclusion Criteria
Patients with elevated renal parameters on the dialysis and heart failure due to coronary insufficiency were excluded from the studies. Positive cases with retroviral diseases and those afflicted by other communicable viral diseases are excluded from the study.
Those cases with large gangrene at presentation with unsalvageable foot and other end of spectrum with asymptomatic critically neuroischemic diabetic foot are all excluded from the study.
Those with severe co morbid illnesses, and poor functional status are not fit for any revascularization and reconstruction are not included.
Treatment Schedule
All 50 patients had undergone all 4 steps of treatment
Step no 1
Those with stable wound are taken up for color Doppler imaging followed by CT angiogram to discern the arterial altered anatomy.
Those with invasive infection and wet gangrene (unstable wound) are taken for immediate debridement on emergency basis and wound is stabilized with intravenous antibiotics and simultaneously they are investigated for arterial anatomy.
Step no 2
All had undergone immediately any one of the following PDDR procedure by the revascularization team based on the location severity of stenosis and blocks A. Distal perforosome directed bypass.
B. Combination of bypass for in flow vessel disease and perforosome directed distal angioplasty –hybrid procedure.
C. Perforosome directed distal angioplasty alone.
Step no 3
RVI found in all cases are treated for variable period with balanced debridement and active special dressing including topical negative pressure dressings.
Step no 4
After healing potential heralds in the wound early definitive perforosome directed reconstruction done in all cases.
As an integral part of reconstruction adjuvant procedures like tendon transfers, tenotomies, tendon lengthening, contracture releases, capsulotomies, arthrodesis, arthroresis, osteotomies and ostectomies are done.
These internal offloading procedures address neuropathy induced faulty biomechanics, faulty muscle recruitments, muscle imbalances, tendoachilles contracture, Charcot’s degeneration of joints, which all predispose to deformities and hyperpression points and precipitate, perpetuate ulcers.
All perforosome directed (perforosome replacement for perforosome) MVR are carried by the single surgeon.
Other General Measures
Diabetologists maintained good glycemic control during the treatment. Regional offloading during revascularization, and subsequently with debridements and reconstructions are usually with well-padded customized posterior slabs fitted with rocker outsole.
They are then weaned on the local offloading with silicone gel socks and type 1-foot wear with molded insoles. Antibiogram directed antibiotics are followed.
Author in this study selected 50 patients critically ischemic diabetic foot with grade IIID to grade IVD lesions in foot (university of Texas grading) [7]. All are treated by PDDR.
After controlling the infection in appropriate cases with antibiotics and average of 3.5 numbers of sittings of debridement before they are taken up for PDDR. After PDDR almost all patients showed signs of regional vascular insufficiency, which is accountable for latency period between revascularization and reconstruction.
Perforosome Directed Reconstruction
For sake of lucid presentation details of reconstruction is divided in to 4 groups.
Group 1: Microvascular reconstruction with above hip perforosome (TDAP – thoracodorsal artery perforator based latissimus dorsi muscle flap with split thickness skin graft) (total 31 cases)
Used for plantar and peri calcaneal defects (29), entire sole defect (2). The LD muscle perforosome is harvested in exact volume dictated by the defect volume and thus donor site morbidity also less.
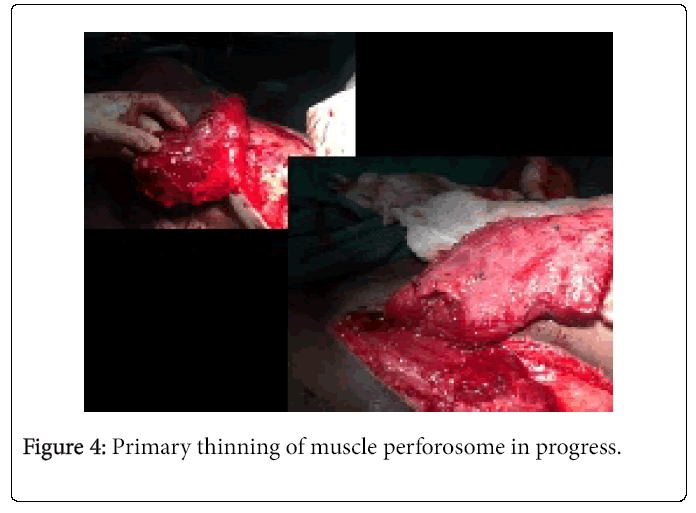
Harvested muscle flap is primarily thinned on its posterior surface as required.
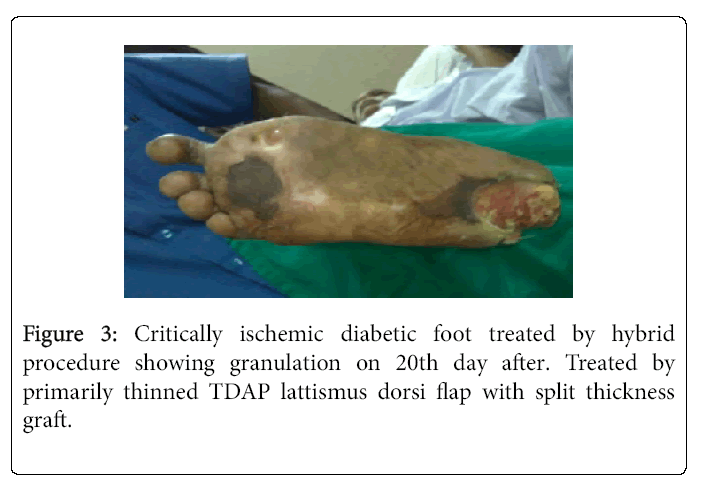
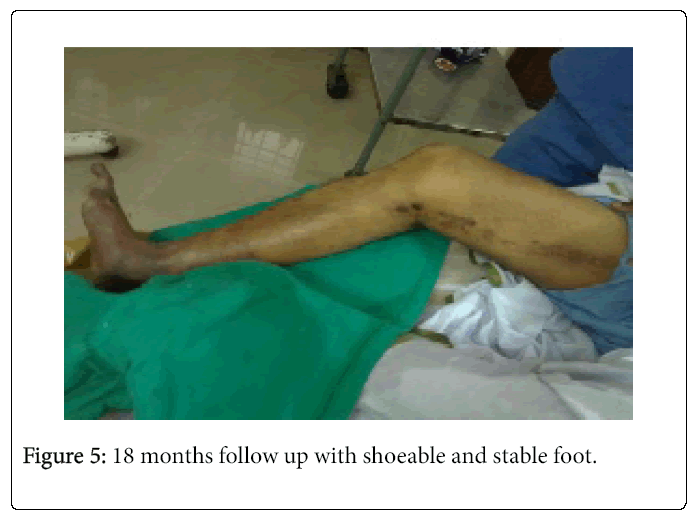
Adjuvant procedures (internal offloading) performed in this group tibialis anterior transfer (12), ostectomies (31), tendoachilles lengthening (4). Average follow up 13 months. Recurrence rate of breakdown and ulceration (6%). It took 2.5 months on average to assume bipedal walking in this group. Mortality (periprocedural) nil. Flap success rate 100% (Table 1) (Figures 3-5).
| Type of PDDR | Complications related to PDDR | Average Duration of RVI | Average duration of hospital during PDDR and for treatment of RVI | Average duration of hospital stay during reconstruction | Complications related to reconstruction |
|---|---|---|---|---|---|
| Hybrid (1), distal bypass (2) and distal angioplasty (28) | Transient raise in renal parameters (1) | 18.5 days | 21 days | 23 days | Salvaged vein thrombosis (2 cases). No loss |
Table 1: Flap success rate Group 1.
Group 2: Microvascular reconstruction with above hip perforosome (radial forearm flap) (Total 6 cases)
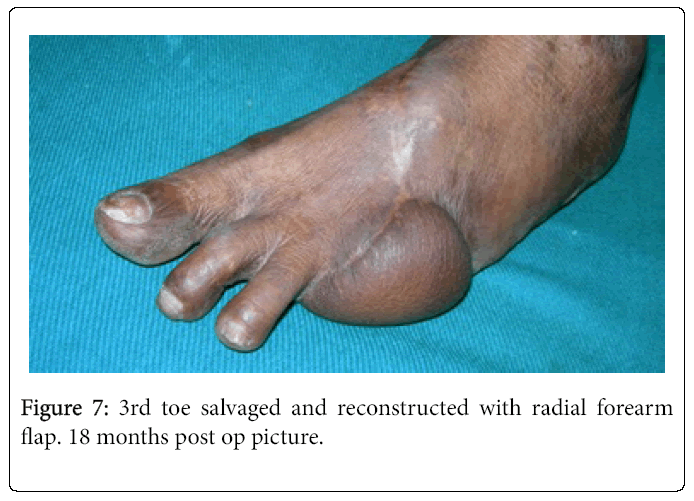
Reconstructed for forefoot defects (6 cases). To suit the volume and thickness primary thinning done only in 2 cases. Adjuvant procedures (internal offloading); tendo Achilles lengthening (5 cases), ostectomies (6 cases). Average follow up in this group is 18 months.
Recurrence rate break down and reulceration in this group is (0%). It took 2 months on average to assume bipedal walking in this group.
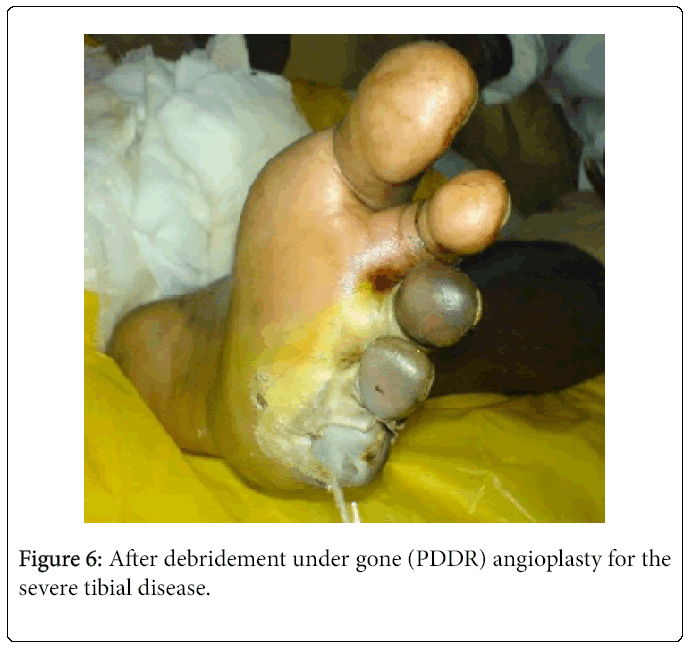
Mortality (periprocedural) nil. Flap success rate 100% (Table 2) (Figures 6 and 7).
| Type of PDDR | Complications related to PDDR | Average Duration of RVI | Average duration of hospital during PDDR and for treatment of RVI | Average duration of hospital stay during reconstruction | Complications related to reconstruction |
|---|---|---|---|---|---|
| Distal angioplasty (6) | Nil | 12 days | 14 days | 28days | Infection one case recovered with antibiotics and drainage |
Table 2: Flap Success rate Group 2.
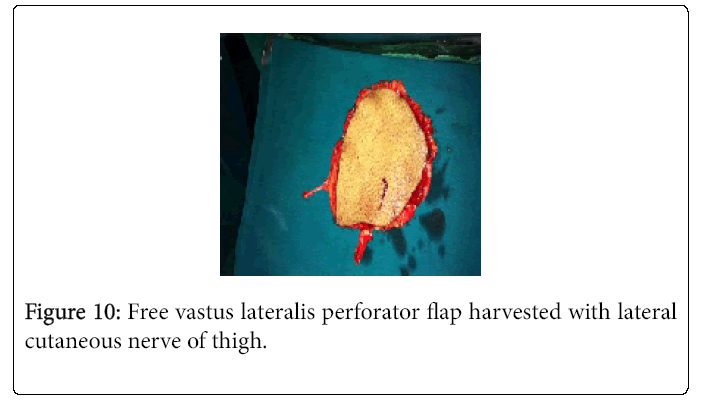
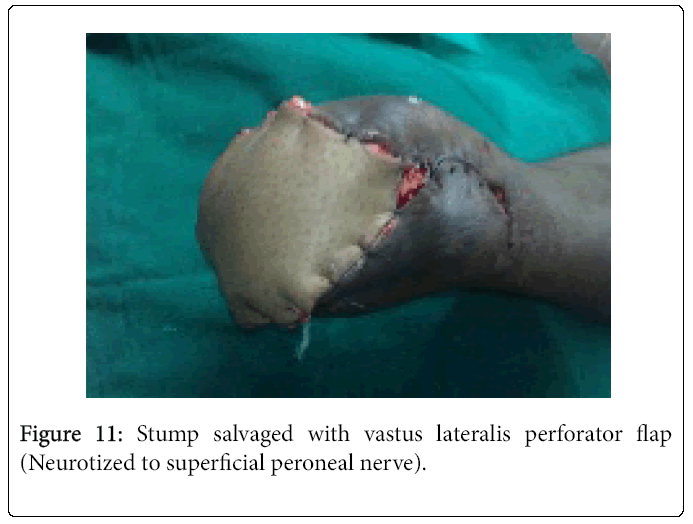
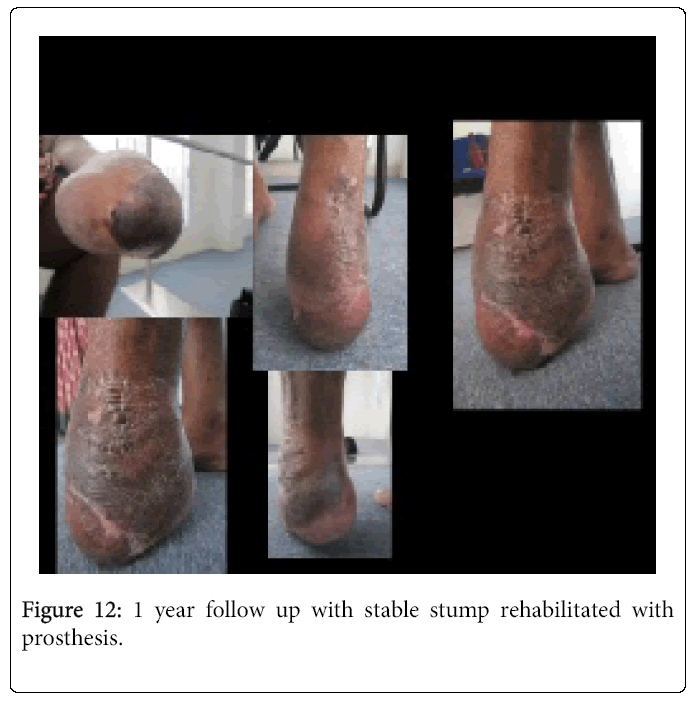
Group 3: Microvascular reconstruction with disease free distant below hip perforosomes –total 8 cases in this group- Vastus lateralis perforator flaps (4 cases) and free Gracilis muscle flap (3) with split thickness graft (as profunda vessel is found free of involvement). Free medial plantar artery perforator flap (1 case-where the contralateral foot has preserved arch and disease free)
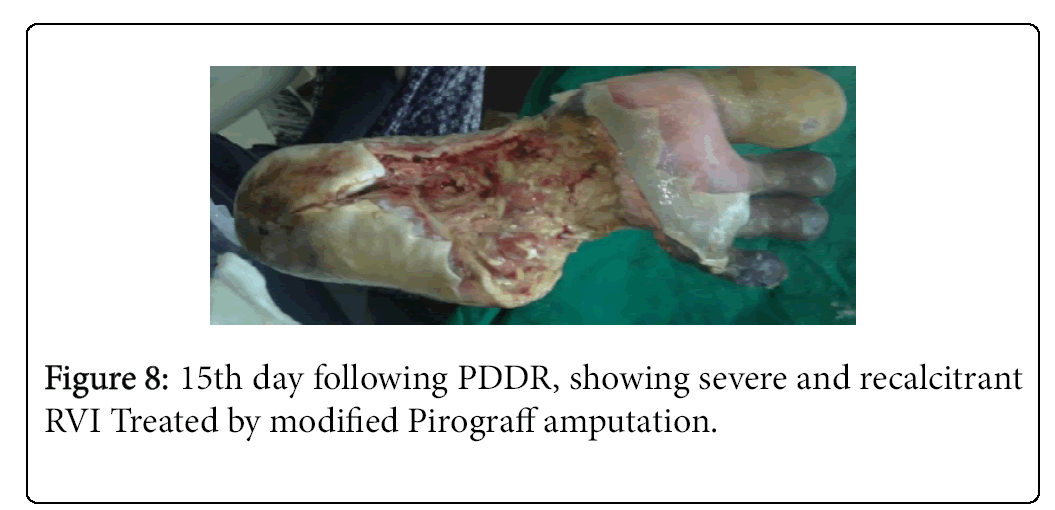
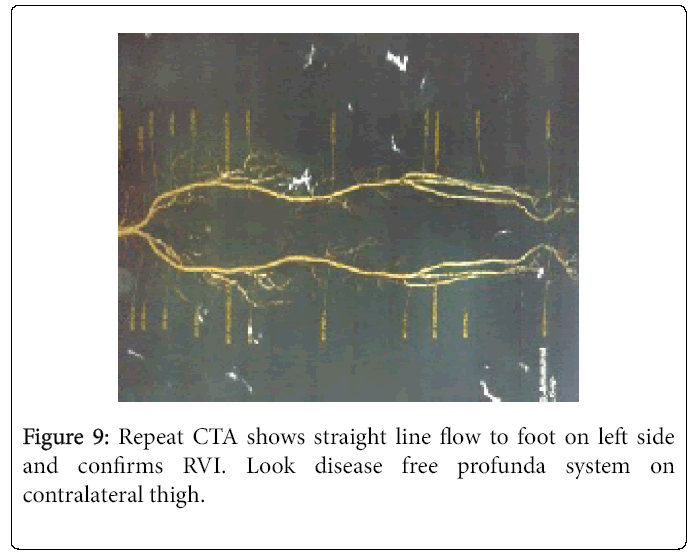
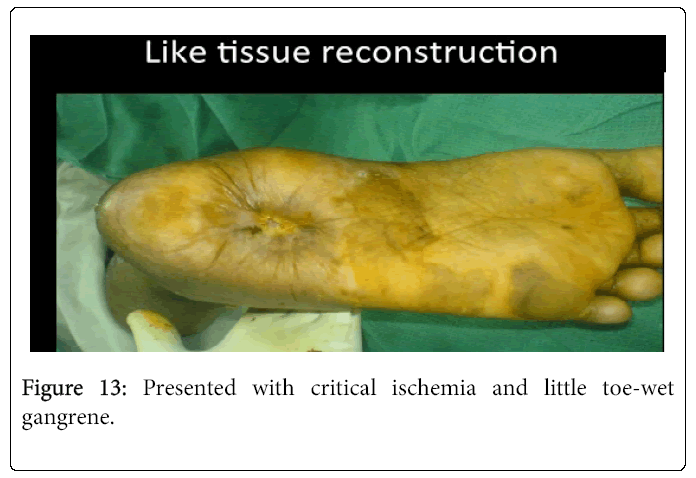
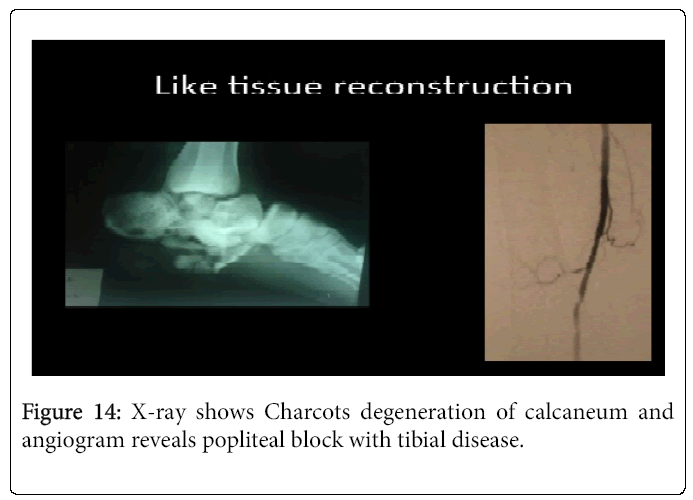
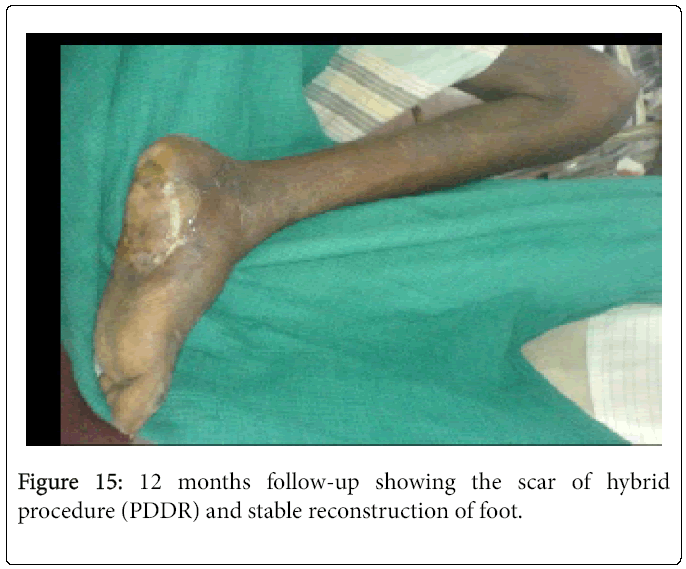
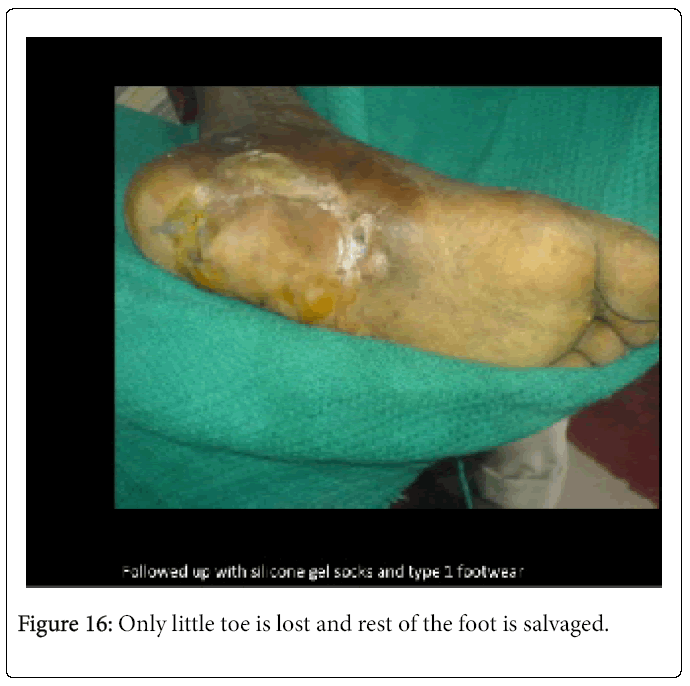
Reconstructed defects: failed pirograffs amputation stump (1). Plantar calcaneal defects (7). Primary thinning of perforator flap to suit the defect in such a way that prosthetic rehabilitation of stump carried easily. Gracilis is trimmed to defect dimension maintaining the NV hilum on its anterior border of muscle. Adjuvant procedures (internal offloading); ostectomies (8); tendon transfers (8). Average follow up in this group is 18 months. Recurrence and transfer lesions in this group is 1 case (treated by excising plantar calcaneal spur osteotomy on raising the flap). It took 3.5 months on average to assume bipedal walking in this group. Mortality (periprocedural) nil. Flap success rate 100% (Table 3) (Figures 8-16).
| Type of PDDR | Complications related to PDDR | Average Duration of RVI | Average duration of hospital during PDDR and for treatment of RVI | Average duration of hospital stay during reconstruction | Complications related to reconstruction |
|---|---|---|---|---|---|
| Distal angioplasty (7) Hybrid procedure (1) |
Nil | 20 days | 28 days | 23 days | Salvaged vein thrombosis (1 case). No loss |
Table 3: Flap Success rate Group 3.
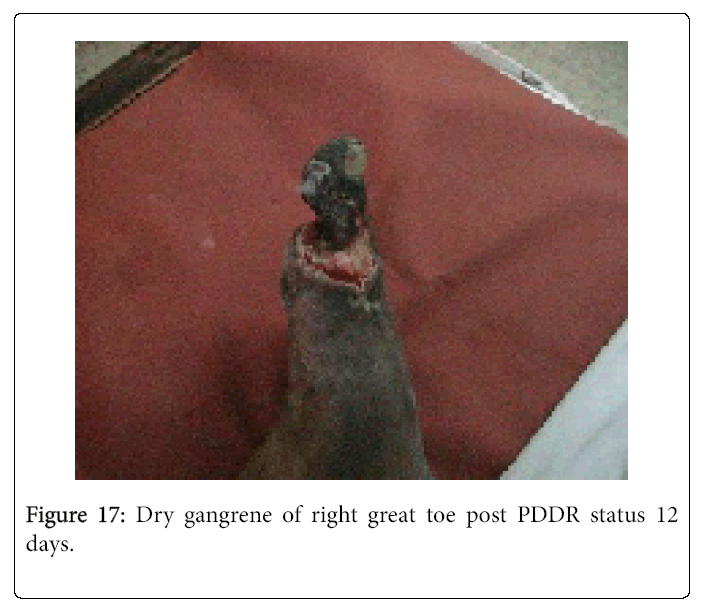
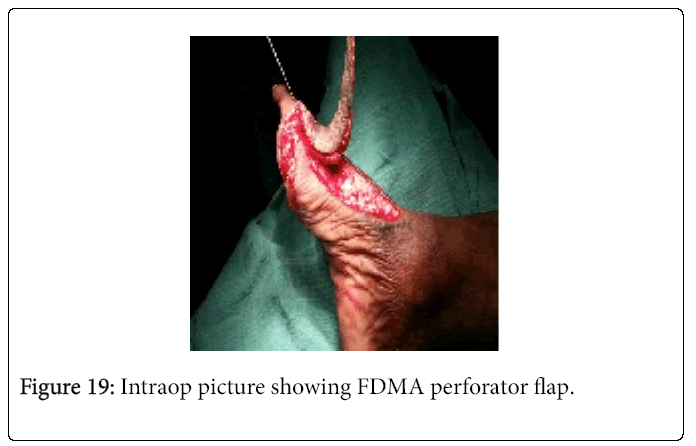
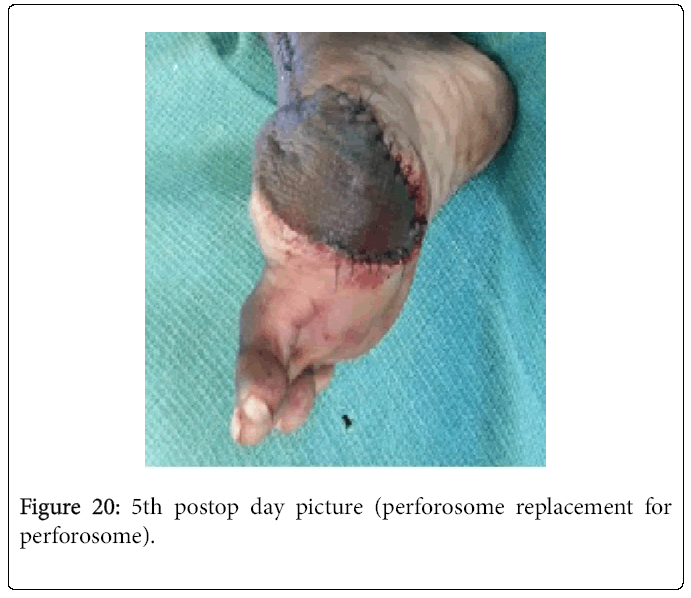
Group 4: Microvascular reconstruction with regional below hip perforosome (arcuate artery perforator flaps1 case, First dorsal metatarsal artery based perforator 5 cases)(total 6 cases). These are microvascular flaps with no microvascular anastomosis
Used for dorsum foot (1 case) and great toe amputation stump defects (5). In the post PDDR status these raw area are 6cm2 on average. So the regional perforators checked by post revascularization CTA and hand held Doppler and found satisfactory. Therefore these perforator/propeller flaps are done. Adjuvant procedures (internal offloading) performed in this group tibialis anterior transfer (5), ostectomies (6), tendoachilles lengthening (4). Average follow up 13 months. Recurrence of ulceration and transfer lesion nil. It took 26 days on average to assume bipedal walking in this group. Mortality (periprocedural) nil. Flap success rate 100% (Table 4) (Figures 17 – 20).
| Type of PDDR | Complications related to PDDR | Average Duration of RVI | Average duration of hospital during PDDR and for treatment of RVI | Average duration of hospital stay during reconstruction | Complications related to reconstruction |
|---|---|---|---|---|---|
| Distal angioplasty in all cases | Transient raise in renal parameters (1) | 12days | 22days | 23 days | Partial loss salvaged by secondary dressing .No complete loss |
Table 4: Flap success rate Group 4.
Mortality (periprocedural) nil. Flap success rate 100% (Table 3) (Figures 8-16).
Surgical Strategies for Microvascular Transfer
Normal perforosomes from above hip and free from functional micro angiopathy is transferred to the defect is the best solution for Regional vascular insufficiency.
Working with radiologists and Angiogram Disease Free Below Hip Perforosomes can be chosen.
In perforosome approach with impetus on one stage reconstruction, either free flap with recruited tailored perforosomes or regional perforator /propeller flap with supernormal blood supply is harvested. With PDDR and subsequent balanced debridements and special active dressings the RVI is treated. Thus the microvascular flaps with robust blood supply complements the PDDR and completely reestablish the healing potential in neuroischemic diabetic foot.
To prevent dissection of vessel wall, which is common; No dilatation of atherosclerotic vessels. Recipient vessel must be cut back to get disease free soft vessel or may have to choose another vessel. If only recipient vessel is diseased come “out-in” on the donor vessel and preferably in out at the diseased recipient vessel. If both vessels are diseased use double arm sutures and in out fashion on both sides. Vessel wall dissection is common and therefore use of LIGA CLIPs during transfer and this in authors experience eschew the vessel wall dissection.
To prevent cut throughing of vessel, thin or fine suture material in the order of 10/0 should be used. Micropoint round bodied needles are preferred over micropoint spatulated needles.
To prevent thrombosis Post op routine LMW heparin in addition to LOMODEX and Trental infusion is our routine. Epidural top ups help in preventing vasospasm and its sequelae –the thrombosis is routinely used by the author. This also provided extended postoperative pain relief.
Discussion
Now the global consensus in the management of diabetic foot is to salvage foot with all modalities possible and aim for shoeable and stable foot or residuum of foot. The second important aim one should incorporate all adjuvant treatments as an integral part of reconstruction to prevent transfer lesions and recidivism. There are several factors like Monckebergs sclerosis of infra genual vessels, edema, neuropathy and infection pose hurdles in the recognition of the critically ischemic diabetic foot [8]. Sclerosed vessels in the infragenual region masquerade the ischemia by false high ABI. Edema, neuropathy blunts the inflammatory response in ischemic foot and gives false appearance of no florid infection. Bacterial infection pose more metabolic demand locally and aggravate ischemia in diabetic foot in the face of fixed and restrained blood flow resulting in more devitalization and in turn results in more devitalized tissues which are perfect pabulum for the bacterial proliferation and thus reverberating ischemia-infection down hill cycle sets in the diabetic foot. Unless timely debridement and mechanical control of infection is achieved this cycle ultimately going to result in the amputation. Therefore the first step in the critically ischemic diabetic foot is control of invasive infection and then early revascularization. There are several studies to this date [9] reports that limb salvage rate is around 60% following revascularization. But in this study we have salvaged foot or foot residuum in all cases.
In all cases during the latency period, the time gap between the revascularization and definitive reconstruction is optimally utilized for (A) balanced debridements to save all potentially salvageable tissues. (B) To make wound clean, and free from bio burden. (C) To render the wound that is showing healing potential from all quarters (as sign of recovery from RVI) and so that a well vascularized distant tissue (microvascular flap) is coapted to wound surface with good healing potential, and this avoids any delayed necrosis at wound edges. (D) Patient general condition is optimized.
There exists a morbid connexion between the group of patients whose critically neuroischemic diabetic foot is unsalvageable undergo amputation, also are prone for pre terminal coronary events with high mortality as shown by the [5,7] EURODIALE study. Therefore the logical conclusion is saving the foot or residuum of foot indirectly saves the life of these patients. “Saving limb and foot is therefore saving life.” One can also reasonably come in to this conclusion after analyzing the sequel of major limb amputation. For example a below knee amputation increases the walking metabolic equivalents by 110% which impose severe demand [10] on the myocardium which is already receiving limited perfusion from the coronary atherosclerosis may easily precipitate the pre terminal event. Thus the timely revascularization and microvascular reconstruction, which rapidly replenishes the healing potential at recipient site, goes long way in saving the limb and in turn saving the life. This hypothesis is proved by our results of this study, which showed no mortality in the study group. To this date there is no other studies found in literature with same perforosome approach. So the results of this study are compared to only related studies where MVR is done after revascularization [9,11-13]. In Goldberg et al. study follow up period averaged 43 months with 96% successful MVR. Our study the follow up averaged only 18 months but we had 100% successful MVR. Their recurrence rate was 11%. Ours is only 6%. This could be possibly accounted by perforosome approach right from the recognition of critical ischemia in diabetic foot. Also noted in this study are no attempt has been made for direct revascularization of ischemia areas [14]. In FW Logerfo et al. study [12] again the MVR procedures lowers the major limb amputation rate during their study period. We also established in our study by our perforosome approach when practiced in timely manner we can salvage shoeable and stable foot or residuum of foot with nil major amputation in the study population in average 18 months follow up period. In Karp et al. [15] studies 19 patients with MVR for 65 months. During this period they have done only one amputation for flap breakdown. Again this study did not include only critically ischemic diabetic foot. So this anatomical approach fetch 100% salvage rate of useful foot in the critically ischemic diabetic foot study population. With significant Impact (p<0.01) the PDDR brings in the healing potential on average 21 days when compared to our own institutional records between 2001 to 2006 in comparable patient population. Overall amputation in the institute for diabetic foot is reduced by 40% in the study period.
Conclusion
Contemporary alert surgeon must be fully aware of beneficial effects of PDDR and perforosomal anatomical approach in MVR which effectively heals and salvage the critically ischemic diabetic foot. PDDR rapidly replenishes the perfusion and brings rapidly the healing potential and serves well to save all potentially salvageable tissues in ischemic diabetic foot. Microvascular transfer of perforosomes with supra normal blood supply helps in achieving the early saving of critically ischemic diabetic foot after revascularization.
Conflict of Interest
None declared.
References
- Hicks CW, Selvarajah S, Mathioudakis N, Sherman RE, Hines KF, et al. (2016) Burden of infected diabetic foot ulcers on hospital admission and costs. Ann Vasc Surg 33: 149-158.
- Apelqvist J, Elgzyri T, Larsson J, Löndahl M, Nyberg P, et al.(2011) Factors related to outcome of neuroischemic/ischemic foot ulcer in diabetic patients. J Vasc Surg 53:1582-1588.
- Blondeel PN, Van Landuyt KH, Monstrey SJ, Hamdi M, Matton GE, etal. (2003) The ��?Gent� consensus on perforator flap terminology; preliminary definitions. Plast Reconstr Surg 112:1378-1383.
- Boradmann M (2013) The angiosome concept in clinical practice: implications for patient-specific recanalization procedures. J Cardiovasc surg (Torino) 54:567-571.
- Beckert S, Witte M, Wicke C, Königsrainer A, Coerper S (2006) A new wound-based severity score for diabetic foot ulcers.Diabetes Care 29:988-992.
- Rubino C, Coscia V, Cavazzuti AM, Canu V,et al. (2006)Hemodynamic enhancement in perforator flaps: the inversion phenomenon and its clinical significance. A study of relation of blood velocity and flow between pedicle and perforator vessels in perforator flaps. J Plast Reconstr Aesthet Surg59:636-643.
- Prompers L, Schaper N, Apelqvist J, Edmonds M, Jude E, et al. (2008)Prediction of outcome in individuals with diabetic foot ulcers: focus on the differences between individuals with and without peripheral arterial disease. The EURODIALE Study.Diabetologia 51:747-755.
- Mills JL, Conte MS, Armstrong DG, Pomposelli F, Schanzer A, et al. (2014) The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: Risk stratification based on Wound, Ischemia and foot Infection (WIfI). J Vasc Surg 59:220-234.
- Hinchliffe RJ, Andros G, Apelqvist J, Bakker K, Friederichs S, et al. (2012)Effectiveness of Revascularization of the ulcerated foot in patients with diabetes and peripheral arterial disease: a systematic review. Diabetes Metab Res Rev 28:179-217.
- Jetté M, Sidney K, Blümchen G (1990) Metabolic equivalents (METS) in exercise testing, exercise prescription and evaluation of functional capacity. Clin Cardiology 13:555-565.
- Rainer C, Schwabegger AH, Meirer R, Perkmann R, Ninkovic M, et al. (2003) Microsurgical management of diabetic foot. J Reconstr Microsurg19:543-553.
- LoGerfo FW, Gibbons GW, Pomposelli FB, Campbell DR, Miller A, etal. (1992) Trends in the care of diabetic foot. Expanded role of arterial reconstruction.Arch Surg127:617-620.
- Neville RF, Attinger CE, Bulan EJ, Ducic I, Thomassen M, et al. (2009)Revascularization of a specific angiosome for limb salvage: does the target artery matter?.Ann Vase Surg23:367-373.
- Goldberg JA, Adkins P, Tsai TM (1993) Microvascular reconstruction of foot: weight bearing pattern, gait analysis and long-term follow-up.Plast Reconstr Surg 92:904-911.
- Karp NS, Kasabian AK, Siebert JW, Eidelman Y, Colen S, et al. (1994)Microvascular free flap salvage of diabetic foot: 5-year experience. Plast Reconstr Surg94:834-840.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13035
- [From(publication date):
September-2016 - Aug 20, 2025] - Breakdown by view type
- HTML page views : 12056
- PDF downloads : 979