Molecular Mechanism of Diabetic Retinopathy and Its Pharmacotherapy: A Brief Review
Received: 01-Feb-2023 / Manuscript No. ijrdpl-22-84604 / Editor assigned: 03-Feb-2023 / PreQC No. ijrdpl-22-84604 / Reviewed: 17-Feb-2023 / QC No. ijrdpl-22-84604 / Revised: 21-Feb-2023 / Manuscript No. ijrdpl-22-84604 / Accepted Date: 27-Feb-2023 / Published Date: 28-Feb-2023 QI No. / ijrdpl-22-84604
Abstract
Diabetic retinopathy (DR) is associated with vascular dysfunction in retinal vascular system and is the cause of blindness among affected persons. It is one of the life-threatening complications of diabetes mellitus (DM). The STAT proteins, vascular endothelial growth factor (VEGF) and metalloproteinase (MMP) enzymes are responsible for angiogenesis and edema in retinal tissue. The other active marker proteins of angiogenesis associated DR includes epidermal growth factor (EGFR), transforming growth factor (TGF), platelet activating factor (PAF), Hypoxia inducible factor (HIF), integrin, activins and insulin like growth factor. In addition, the neuroinflammation is one of the pathological interventions during DR. Reviewing the factors associated with pathogenesis of retinal damage is important therapeutic marker for research of novel drugs by keeping focus on patient vision. This review points out the novel anti-angiogenic drugs useful for the treatment of DR.
Keywords
Diabetic retinopathy, Angiogenesis, Molecular mechanism, Novel pharmacotherapeutic targets
Introduction
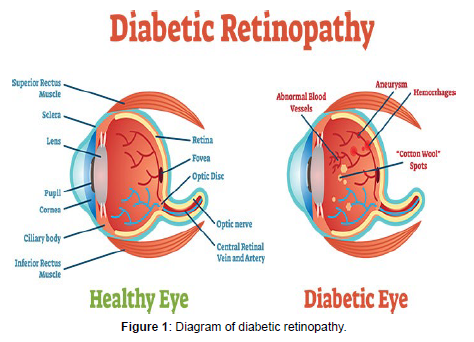
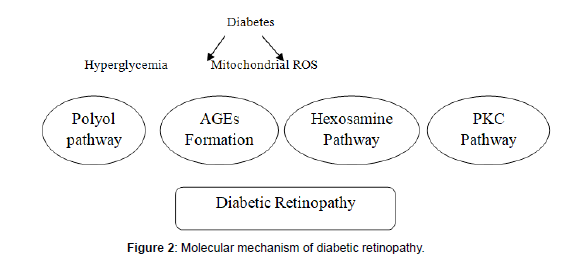
In 1522 B.C., the first recorded mention of diabetes symptoms was made. Diabetes is a globally prevalent disease that affects a variety of body organs [1]. Diabetic retinopathy is defined as damage to the retina's micro vascular system caused by persistent hyperglycemia, which can result in blindness [2]. Diabetic retinopathy is a significant diabetic condition. Early diagnosis of diabetic retinopathy by an automated method is more helpful than manual detection due to advancements in artificial intelligence [3] it is the leading cause of new blindness cases among adults aged 20 to 74. Almost all individuals with type 1 diabetes and more than 60% of people with type 2 diabetes have this condition develop retinopathy throughout the first two decades of their condition. It is indicated by bleeding or the fluid buildup in the retina at a later stage of diabetes [4]. Diabetic retinopathy is greatly increased by high blood pressure, high cholesterol, diabetic kidney disease, genetically enhanced diabetes, or changes in blood sugar levels [5]. In this case, blood is delivered to all layers of the retina via high blood sugar levels might damage tiny blood capillaries, making them vulnerable. When there is a significant amount of glucose or fructose in the blood, the artery begins to crumble due to an insufficient supply of oxygen to the cells [6]. Diabetes mellitus affected around 30 million persons in the United States in 2017, accounting for 9.4% of the population. Diabetic retinopathy accounts for roughly 40%, of the total cost of diabetes treatment in the United States resulting in an annual economic burden of $120 billion. Not only in terms of disease management costs, but also in terms of lost worker productivity [6] the inability of the HbA1c level to predict the diabetic retinopathy's onset and progression is also due to plasma glucose fluctuation [4]. Diabetes Retinopathy raises the risk of nephropathy and is a powerful and self-contained predictor of macro albuminemia development [6-8] Diabetic retinopathy must be detected in order to save the patient's vision at an early stage. Many studies have shown that an early diagnosis can preserve 90 percent of diabetic individuals from developing diabetic retinopathy. An ophthalmologist can manually diagnose diabetic retinopathy or automatically by a computer technology. Various signaling mechanisms, including as leukostasis and platelet activation, have been discovered to be implicated in the pathophysiology of DR. ICAM-1, vascular endothelial growth factor (VEGF), NF-kB, inducible nitric oxide synthase (iNOS), COX, oxidative stress. [2]. A number of researches have looked into the link between different dietary components and diabetic retinopathy. Micronutrients, macronutrients, food groups and drinks, as well as dietary patterns, are all included. Diabetic macular edema can appear at any stage of diabetic retinopathy's evolution. A breach of the bloodretinal barrier causes it which as a result of enhanced vascular (Figure 1, 2) permeability and of hard exudates in the macula. Micro aneurysms appear early in the progression of diabetic retinopathy and are frequently the first clinically noticeable symptoms. Inflammatory cells are known to be attracted to these 'balloon-like' protrusions of the capillary wall causing additional endothelial lining damage. The international clinical diabetic retinopathy scale is one of the most widely used clinical scales, including a 5-point scale diabetic retinopathy (mild, moderate, severe, and proliferative). The collection of fluid (edema) in the macula, a portion of the retina, is referred to as DME. The macula is a part of the retina necessary for reading, identifying faces, and driving because it provides excellent, straight-ahead vision. In diabetic retinopathy, DME is the most common cause of vision loss patients. DME affects Patients with diabetic retinopathy account for almost half of all diabetic retinopathy patients. DME can strike at any time during a person's life. Diabetic retinopathy, albeit as the condition worsens, it becomes more likely. People with any kind of diabetes can develop diabetic retinopathy (type 1, type 2 or gestational). The longer a person has diabetes, the higher the risk. Diabetic retinopathy affects 40 to 45 percent of diabetics in the United States, yet only approximately half of them are aware of it. Diabetic retinopathy can develop or deteriorate quickly in women who acquire or have diabetes during pregnancy. For clear eyesight, a healthy, clean cornea is required. When if your cornea is damaged due to disease or an accident, it can be. Swell, scar, or become badly deformed; distorting your vision. Certain disorders can obstruct your cornea's clarity; putting corneal failure is a possibility for you. These are some of them:
• Scarring can result from infections such ocular herpes or fungal keratitis.
• Scarring caused by trichiasis, which happens when eyelashes grow inwards, toward the eye, and rub on the cornea
• Fuchs' dystrophy, for example, is a hereditary disorder.
• Keratoconus, which is a type of advanced keratoconus.
• Corneal thinning and uneven corneal morphology (such as with keratoconus).
• LASIK surgical problems are uncommon.
• Corneal chemical burns or damage caused by an eye accident.
• Corneal edema (excessive swelling).
• Rejection of grafts after a corneal transplantation before.
• Corneal failure as a result of problems from cataract surgery.
Corneal eye disease, which I affect about 10 million individuals worldwide and is the fourth leading cause of blindness (after cataracts, glaucoma, and age-related macular degeneration). More than 47,000 corneal transplants will be performed in the United States in 2013, according to the Eye Bank Association of America. Since 1961, corneal transplants have helped over one million people regain their vision.
• Diabetic retinopathy is a condition that the blood vessels in the retina, which lines the back of the eye and is light-sensitive, are damaged. It is the leading cause of vision impairment and blindness in people of working age, as well as the leading cause of vision loss in diabetics.
• Diabetes macular edema. DME is a diabetic retinopathy condition that produces swelling in the macula, a portion of the retina. Diabetic eye illness, in any form, has the potential to cause significant vision loss and blindness.
Chronically elevated blood sugar causes diabetic retinopathy in the retina, which causes damage to the retina's tiny blood vessels. The retina detects light and converts it into messages that the optic nerve sends to the brain. Diabetic retinopathy is a kind of retinopathy caused by diabetes can induce fluid leakage or hemorrhage (bleeding) in the retina, causing vision distortion. New abnormal blood vessels proliferate (increase in number) on the retina's surface in the most severe form. Surface, causing scarring and retinal cell loss.
Diabetic retinopathy can be divided into four stages:
A. Mild non-proliferative retinopathy- Micro aneurysms, or small regions of balloon-like bulging in the retina, are present at this stage of the disease tiny blood vessels, form. Fluid may flow into the retina from these tiny aneurysms. There is at least one micro aneurysm in or near the retina. Other lesions may or may not be present. Half of all diabetics in the world suffer from the simple form of diabetic retinopathy.
B. Moderate Non proliferative retinopathy- The retina's blood vessels may expand and distort as the disease advances. It's also possible that they'll lose their ability to move blood. Both disorders induce distinct alterations in the retina's appearance and may play a role in DME.
C. Severe Non proliferative retinopathy- Many more blood vessels are clogged, cutting off blood circulation to parts of the retina. These tissues secrete growth factors, which signal the retina to start producing new blood vessels.
D. Proliferative Diabetic retinopathy - At this advanced stage, growth factors produced by the retina promote the development of new blood vessels that grow along the inside surface of the retina and into the vitreous gel, which fills the eye. The young blood vessels are more prone to leaking and bleeding because they are weak. Scar tissue can contract, causing retinal detachment (the separation of the retina from the underlying tissue) similar to how wallpaper peels away from a wall. Retinal detachment can result in vision loss that is permanent. Wallpaper rips away from a wall in a similar way. Retinal detachment can result in permanent visual loss. It entails the creation of new blood vessels, which are caused by retinal ischemia and spread out either from the disc or from other parts of the retina. Diabetic retinopathy is a form of retinopathy in which the blood vessels in the eye get damaged.
E. Pathophysiology- Damage to the retina's small blood vessels and neurons causes diabetic retinopathy. The earliest changes that contribute to diabetic retinopathy include narrowing of the retinal arteries, which results in lower retinal blood flow; malfunctioning of the inner retina's neurons, which is followed by variations in the function of the outer retina, which leads in modest vision impairments. The blood-retinal barrier is broken, allowing blood components to flow into the retina neuropile, which protects the retina from a variety of contaminants in the blood (including poisons and immune cells). The basement membrane of retinal blood vessels thickens over time, capillaries degrade, and cells, particularly pericytes and vascular smooth muscle cells, are lost. Ischemia and tiny aneurysms, which appear as balloon-like structures projecting from capillary walls and attracting inflammatory cells, as well as advanced dysfunction and degeneration of the retina's neurons and glial cells, result as a result of this. The syndrome usually emerges 10–15 years after diabetes mellitus is established. Blood glucose is considered to trigger pericyte mortality by activating protein kinase C and mitogen-activated protein kinase (MAPK), which inhibits signaling through platelet-derived growth factor receptors, which supports cellular survival, proliferation, and growth via a sequence of intermediates. The withdrawal of this signal causes the cells in this experimental model to die via programmed cell death. Small blood vessels, such as those in the eye, are at risk due to poor blood sugar (blood glucose) management. An excessive amount of glucose damages the retina's tiny blood vessels. During the early stages of non-proliferative diabetic retinopathy, most people do not notice any changes in their vision (NPDR). Early abnormalities in the eye that are reversible and do not impair central vision are referred to as background retinopathy. According to a genetic study, diabetic retinopathy has a familial link to glucose levels, low-density lipoprotein cholesterol, and systolic blood pressure, implying that glycemic control and cardio metabolic factors may play a role in the progression of diabetic retinopathy.
F. Diagnosis-OCT (optical coherence tomography) imaging is ideal for diagnosing DME because of its high axial resolution and large retinal scan coverage. DME-related alterations in the photoreceptor, external restricting film, Bruch's layer, and retinal pigment epithelium layer were discovered using spinal domain optical coherence tomography (SD-OCT). The conventional approach in the screening for diabetic retinopathy is ophthalmoscopy with or without pupil dilation; Detection of micro aneurysms in the posterior pole is the first clinical sign, symptom, and fluorescein angiography is also employed for the detection.
• Visual acuity testing is the first step. This eye chart exam assesses a person's vision at different distances.
• Tonometry. The pressure inside the eye is measured with this test.
• Pupil dilation is a condition in which the pupil dilates. The pupil dilates (widens) when drops are placed on the eye's surface, enabling a doctor to examine the retina and optic nerve
The doctor can evaluate the retina for the following things during a full dilated eye exam:
• Blood vessel changes
• Leaky blood vessels or warning signs of leaky blood vessels, such as fatty deposit
• Macula edema (swelling of the macula)
• Lens alterations
• Nerve tissue damage
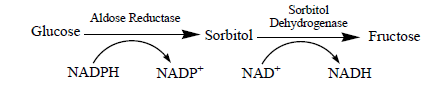
Increased Polyol Pathway Flux
The detrimental effects of hyperglycemia-induced increases in polyol pathway flow could be explained by a number of postulated mechanisms. It's a two-step metabolic pathway in which glucose is converted to sorbitol, which is then converted to fructose by sorbitol dehydrogenase. The sorbitol (polyol) pathway, an alternative route of glucose metabolism, is made up of these two enzymes. Sorbitol has a difficult time diffusing across cell membranes and builds up, resulting in oxidative stress. Excess sorbitol accumulation has been discovered in a variety of tissues, including diabetic animals' retinas and non-diabetic eye donors' retinas subjected to high glucose at levels comparable to non-diabetic rats' retinas incubated under the same conditions Using NAD+ as a cofactor, the enzyme sorbitol dehydrogenase (SDH) transforms sorbitol to fructose. When sorbitol is converted to fructose, NAD+ is changed to NADH, which is the substrate for NADH oxidase, which produces reactive oxygen species, causing oxidative stress (ROS). These are essential co-factors in the body's redox system. Reduced levels of these co-factors led in lower levels of glutathione (a scavenger of free radicals) and higher levels of oxidative stress. It is the most common cause of retinal damage.
A. Accumulation of AGEs- The accumulation of advanced glycation end products in retina is caused by chronic hyperglycemia. The AGE-specific receptor is their primary signaling receptor (commonly abbreviated as RAGE) -AGEs are responsible for stimulate inflammatory signaling pathways by releasing reactive oxygen species. The best chemically documented AGEs in humans are carboxymethyl lysine (CML), carboxyethyl lysine (CEL), and pentosidine, which act as markers for AGE formation and accumulation in hyperglycemia. CML and other AGEs have been identified in diabetes patients' retinal blood vessels and found to correlate with the severity of retinopathy, showing that AGEs play a pathophysiological role in diabetes. Phosphatidylinositol 3 recruitment can be triggered by AGE receptor binding, which involves tyrosine phosphorylation of Janus kinase (JAK)/signal transducers and activators of transcription (STAT) and tyrosine phosphorylation of Janus kinase (JAK)/signal transducers and activators of transcription (STAT). From kinase to Ras activation of protein kinase C to oxidative stress via NFkB and AP, AGEs interact with cells in a variety of ways a single transcription.
B. Hexosamine pathway- Increased glucose flow insulin resistance and diabetic vascular disease have been linked to the Hexosamine pathway. Problems and the activation of growth factor synthesis in vitro and in vivo investigations. The bulk of glucose is metabolized through glycolysis, which uses glucose-6 phosphate to do so being the first step, followed by fructose-6 phosphate, and pathway. However, Some fructose-6-phosphate is diverted into a signaling pathway, where it is transformed to glucosamine-6-phosphate, which is then turned to UDP (uridine diphosphate) N-acetyl glucosamine by an enzyme called GFAT (glutamine: fructose-6 phosphate amido transferase) The Hexosamine biosynthetic route may promote retinal neuro degeneration by decreasing the neuroprotective action of insulin or by inducing apoptosis, which could be caused by changes in finally the rest of the glycolytic protein glycosylation. Benfotiamine, a lipid soluble thiamine, may be clinically helpful in reducing the start and progression of diabetes pathogenesis resulting from hyperglycemiainduced vascular damage because of its capacity to block the Hexosamine pathway, as well as AGE production and PKC pathways Glycolipids, proteoglycans, and glycoprotein are formed when N-acetyl glucosamine-1 is converted to UDP-N-acetyl glucosamine.
C. Pkc pathway- Increased permeability of the endothelium is a sign of endothelial dysfunction vascular permeability and excessive neovascularization, diabetic macular edema and proliferative diabetic retinopathy are two complications of diabetes. Protein Kinase (PKCs) is a class of roughly 13 isoforms found in a variety of mammalian organs (MM OF DR 1) PKCδ and PKCβ are two PKC isozymes that have been linked to diabetes etiology. PKCδ influences beta islet cell function and insulin resistance in diabetes, and it is PKCβ that plays a key role in diabetic micro vascular problems. The traditional isoforms' activity (PKC-α, -β1/2, and PKCδ) DAG has been connected to vascular dysfunctions and the etiology of diabetes mellitus Phosphatidylserine (PS), The traditional PKC is activated by calcium, DAG, and phorbol esters such as phorbol 12-myristate 13-acetate. (cPKC) isoforms (PKC -α, -β1, -β2, and –γ) (PMA), PS, DAG, or PMA activate novel PKCs (nPKC; PKC- δ, -ε, -θ and -η) while calcium does not. Calcium, DAG, or PMA do not activate atypical PKCs (aPKC; PKC- ζ and -ι/λ) (PKC PATHWAY). LY333531, a protein kinase c inhibitor, is now being tested in a phase 3 clinical trial for severe pre-proliferative diabetic retinopathy and diabetic macular edema.
D. Poly (ADP-ribose) Polymerase (PARP) - It is a nuclear enzyme that resides in an inactive state until the cell is bombarded with DNA-damaging impulses, at which point it becomes active DNA breaks are thought to be required stimuli for PARP activation. Various environmental factors, such as oxidative and nitrosative stress, can cause DNA breakage. PARP catalysis the repair of DNA strand breaks when it comes across them PARP breaks down its substrate, the NAD+ molecule, into nicotinic acid and ADP-ribose, delaying glycolysis and mitochondrial action. Both the alteration of by decreasing mitochondrial superoxide or ROS generation with either MnSOD or UCP-1, the inhibition of glyceraldehydes 3-phosphate dehydrogenase (GAPDH) by ADP-ribose and the lowering of its activity by hyperglycemia were avoided. PARP is well known to play a role in gene transcription regulation as well. PARP interacts with and is controlled by nuclear factor-B (NF-B) , p53 , and AP-1 are all transcription factors. PARP inhibitors or knocking down the PARP gene in cells or mice might reduce NF-B activation and transcription of NF-B-dependent genes such inducible nitric oxide synthase or intracellular adhesion molecule (ICAM)-1. And poly (ADP-ribosylations).
Treatment
A. Glycemic control- A number of big clinical trials (DCCT, UKPDS, and ACCORD) have shown that insulin injections can delay the onset and severity of DR. The Diabetes Control and Complications Trial (DCCT) and the United Kingdom Prospective Diabetes Study (UKPDS) both found that maintaining optimum metabolic control can help prevent the onset and progression of diabetes. The DCCT and UKPDS findings revealed that, while intensive therapy does not entirely prevent retinopathy, it does reduce the chance of developing and progressing diabetic retinopathy. The prevalence of retinopathy in type 1 diabetic participants was 12% when glycated hemoglobin (HbA1c) was 10% in the 14-year progression of retinopathy study (WESDR), and an increased risk of PDR was linked to more severe baseline retinopathy and higher HbA1c levels.
B. Anti-VEGF drugs-Anti-VEGF medications are injected into the vitreous gel to prevent a protein known as vascular endothelial growth factor (VEGF) from stimulating aberrant blood vessels to develop and leak fluid. By inhibiting VEGF, aberrant blood vessel formation can be reversed, and fluid in the retina can be reduced. Anti-VEGF medications include Avastin (bevacizumab), Lucentis (ranibizumab), and Eylea (ranibizumab) (aflibercept). The US Food and Drug Administration (FDA) have approved Lucentis and Eylea for the treatment of DME. The FDA approved Avastin to treat cancer, but it's also used to treat eye problems like DME.
Ranibizumab has received the most extensive testing in clinical trials, including the Diabetic Retinopathy Clinical Research Network (DRCR.net), RISE (clinicaltrials.gov ID: NCT00473330), RIDE (clinicaltrials.gov ID: NCT00473382), RESOLVE (clinicaltrials.gov ID: NCT00284050), RESTORE (clinicaltrials.gov ID: NCT00687804). Intravitreal ranibizumab injections given monthly for DME improve the proportion of eyes with a 2 or 3 step improvement in diabetic retinopathy severity, decrease the proportion of eyes with a 2 or 3 step worsening in diabetic retinopathy severity, and decrease the proportion of eyes progressing to proliferative diabetic retinopathy. In a clinical trial, the NEI-sponsored Diabetic Retinopathy Clinical Research Network compared Avastin, Lucentis, and Eylea. All three medicines were shown to be safe and effective in treating most persons with DME in the research. Patients with 20/40 vision or better at the start of the experiment saw identical improvements in vision regardless of which of the three medicines they were given. Patients with 20/50 vision or poorer at the start of the trial, on the other hand, saw higher improvements in vision with Eylea. Because the cost of Avastin, Lucentis, and Eylea, as well as how often they must be administered, patients should speak with an eye care expert about these concerns. Optical coherence tomography image of a diabetic retinopathy and DME patient's retina (OCT). Before (top) and after (bottom) anti-VEGF treatment, the two pictures were taken (Bottom). The fovea, a part of the macula where vision is generally sharpest, is the dip in the retina. Before therapy, note the enlargement of the macula and elevation of the fovea.
C. Focal/grid macular laser surgery- A few to hundreds of small laser burns are performed to leaking blood vessels in areas of edema around the centre of the macula during focal/grid macular laser surgery. DME laser burns reduce edema in the retina by slowing fluid leaking. Although the surgery is normally completed in a single session, some people may require multiple treatments. Focal/grid laser is used before anti-VEGF injections, on the same day or a few days after an anti-VEGF injection, and occasionally just when DME does not improve after six months of anti-VEGF therapy.
D. Corticosteroids- The development of diabetic retinopathy is complicated by inflammation. Increased blood flow, increased vascular permeability, tissue edema, leukostasis, microglial activation, macrophages and neutrophil infiltration, complement activation, and increased cytokines (VEGF, tumour necrosis factor ,α-interleukin) have all been reported in both animal models and human diabetic retinopathy. Eye issues such as cataract formation, increased intraocular pressure, and glaucoma have been linked to systemic corticosteroids. These side effects are also seen with intra-ocular formulations, and they could be a limiting factor for these operations. DME can be treated with corticosteroids, which are injected or implanted into the eye. They can be used alone or in conjunction with other medicines or laser surgery. The Ozurdex (dexamethasone) implant is meant to be used for a short period of time, whereas the Iluvien (fluocinolone acetonide) implant is meant to be used for a longer period of time. Both are biodegradable and reduce DME by releasing a steady number of corticosteroids. The use of corticosteroids in the eyes raises the risk of cataracts and glaucoma. DME patients who use corticosteroids should be monitored for increased pressure in the eye and glaucoma
E. PKC inhibitors - In animal models of DR, ruboxistaurin, a PKC-beta-specific inhibitor, has been demonstrated to reduce diabetic BRB breakdown and retinal neuropathy.
F. Non-steroidal inflammatory drugs- Although there hasn't been much research done on non-steroidal anti-inflammatory medicines (NSAIDs) for DME, the evidence so far suggests that they have a minor role in its treatment [7].NSAIDs are a class of antiinflammatory drugs that work by blocking cyclooxygenase (COX) enzyme-mediated eicosanoid synthesis. Examples include aspirin and salicylate. NSAIDs work by inhibiting COX enzymes. COX- 1 and COX-2 are the two isoforms of COX enzymes that have been studied the most. COX-1 is a homeostatic enzyme that is expressed constitutively in a variety of cell types. COX-2, on the other hand, is primarily activated at sites of inflammation. PGE2 and PGF2 are two of the most common pro-inflammatory prostaglandins (PGE). COX-2 has NF-B binding sites in its promoter region, and COX-2 expression is controlled by NF-B activity during inflammation. Because iNOS is also an NF-B-driven protein, iNOS and COX-2 are frequently produced together in inflammation. COX2 expression and activity are positively regulated by iNOS products, particularly RNOS. COX-2 expression and its derivatives, notably PGE2, are dramatically enhanced in diabetic retinas and retinal cells treated with high glucose. COX-2 inhibition, but not COX-1 inhibition, lowers PGE2 generation in diabetic rat retinas, indicating that COX-2 plays the primary role of COX-2 in DR. COX-2 inhibition also blocks Immunotherapy. COX-2 is an inducible enzyme that is elevated in response to pain, fever, and inflammation, although it is also expressed in some systems under normal circumstances. In retinal pigment epithelium (RPE) cells, COX-2 is the most prevalent isoform, and it is up-regulated in the presence of pro inflammatory cytokines. COX-2 is involved in angiogenesis and has been linked to choroidal neovascularization (CNV) and proliferative diabetic retinopathy (PDR).
G. Vitrectomy- The removal of the lens at the same time as the vitrectomy was linked to a high rate of anterior segment neovascularization, which led to a preference for leaving the lens alone. The vitreous gel in the middle of the eye is surgically removed in a vitrectomy. The operation is performed under local or general anesthesia to treat significant bleeding into the vitreous. Ports (temporary watertight holes) are inserted into the eye to allow the surgeon to introduce and remove equipment such as a small light or a vitrector (a small vacuum). To maintain eye pressure during surgery and to replace the lost vitreous, a transparent salt solution is gently pushed into the eye through one of the ports. The same instruments used during vitrectomy also may be used to remove scar tissue or to repair a detached retina. Vitrectomy can be done as an outpatient or inpatient procedure, with the latter usually requiring only one overnight stay in the hospital. The eye may be covered with a patch for days to weeks after treatment and may be red and uncomfortable. Drops can be used to minimize inflammation and infection risk in the eye. If both eyes need vitrectomy, the second eye is normally treated after the first has healed.
H. Traditional corneal transplant surgery- A round buttonshaped, full-thickness slice of tissue is taken from the damaged or injured cornea during traditional corneal tr
Ansplant surgery, also known as penetrating keratoplasty (PK), using either a surgical cutting device called a trephine or a fem to second laser. A matched "button" is then positioned and sutured into place from the donor tissue. Sutures (stitches) are usually left in place for a year or longer after surgery.
References
- Firestein GS (2003) Evolving concepts of rheumatoid arthritis. Nature 423:356-361.
- McInnes IB, Schett G (2011) The pathogenesis of rheumatoid arthritis. New England Journal of Medicine 365:2205-2219.
- McInnes IB, Schett G (2017) Pathogenetic insights from the treatment of rheumatoid arthritis. The Lancet 389:2328-2337.
- Streubel A, Siepmann J, Bodmeier R (2003) Multiple unit Gastroretentive drug delivery: a new preparation method for low density microparticles. J Microencapsul 20: 329-47.
- Goole J, Vanderbist F, Aruighi K (2007) Development and evaluation of new multiple-unit levodopa sustained-release floating dosage forms. Int J Pharm 334: 35-41.
- Shrma S, Pawar A (2006) Low density multiparticulate system for pulsatile release of meloxicam. Int J Pharm 313: 150-58.
- Klausner EA, Lavy E, Friedman M, Hoffman A (2003) Expandable gastro retentive dosage forms. J Control Release 90: 143-62.
- Deshpande AA, Shah N, Rhodes CT, Malik W (1997) Development of a novel controlled-release system for gastric retention. Pharm Res 14: 815-19.
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Indexed at, Google Scholar, Crossref
Citation: Shivashankar M (2023) Molecular Mechanism of Diabetic Retinopathyand Its Pharmacotherapy: A Brief Review. Int J Res Dev Pharm L Sci, 9: 149.
Copyright: © 2023 Shivashankar M. This is an open-access article distributedunder the terms of the Creative Commons Attribution License, which permitsunrestricted use, distribution, and reproduction in any medium, provided theoriginal author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 2225
- [From(publication date): 0-2023 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 1836
- PDF downloads: 389