Non Hodgkin Lymphoma in Supraglottis: Case Report
Received: 21-Dec-2016 / Accepted Date: 18-Jan-2017 / Published Date: 25-Jan-2017 DOI: 10.4172/2161-119X.1000285
Abstract
Introduction: Lymphoma represents less than 1% of malignant laryngeal tumors. and the main site in larynx is in supraglottis. The symptoms are very interspecific and the diagnosis is a challenge. Case: A 23 years old man, healthy, referring dysphonia and globus for 2 months. CT and nasofibrolaryngoscopy showed a supraglottic mass without any specific features. Patient was underwent to biopsy which diagnosed non- Hodgkin's large cell B lymphoma. Conclusion: The diagnosis of non-Hodgkin lymphoma laryngeal is a challenge to the otolaryngologist, since, usually, patients present with nonspecific complaints or systemic signs suggestive of this condition and the diagnosis is done only by biopsy
Keywords: Lymphoma; Non-Hodgkin; Head and neck neoplasms; Supraglottic tumors
253863Introduction
Primary hematologic larynx malignancies are rare. Lymphoma represents less than 1% of malignant laryngeal tumors with the B-cell phenotype as the predominant. Fewer than 100 cases of primary laryngeal lymphoma have been reported in the global literature [1–3].
Initially, the patient may present dysphagia, dysphonia, dyspnea, and cervical lymphadenopathy. Systemic symptoms (fever, weight loss and sweating) and lymph nodes are not necessarily included. Indirect laryngoscopy usually reveals a polypoid submucosal supraglottic mass, nonulcerated, with no specific diagnostic features. The diagnosis rests on the histological examination of a biopsy specimen [1,4].
We report a case of primary laryngeal non-Hodgkin's large cell B lymphoma from supraglottis.
Case Report
A 23 years old man consulting for globus sensation and hoarseness associated to vocal fatigue, dysphagia for solids and dyspnea exacerbated after great effort. The condition was started two months earlier. He had no history of fever, night sweats, or weight loss. There is no history of comorbidities and medication use, smoking and alcoholism.
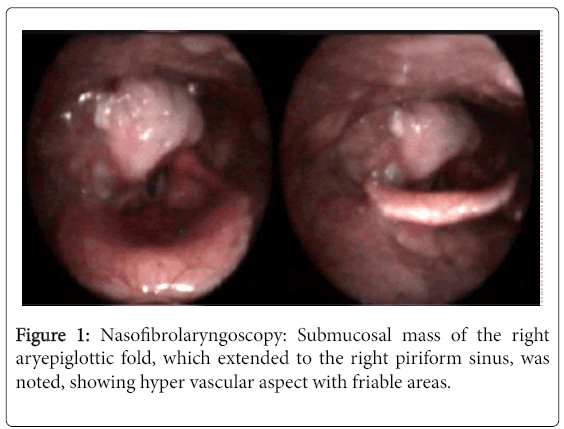
In the neck palpation, there was a cervical lymph node in right level IIa about 3 cm size, it was moveable, soft and painless. The Waldeyer ring was clinically normal. The flexible nasofibrolaryngoscopy (Figure 1), a submucosal mass of the right aryepiglottic.
Laboratory tests did not show changes in peripheral blood and the serology for Cytomegalovirus, Epstein Barr virus, rubella, syphilis, HIV and toxoplasmosis were all negative.
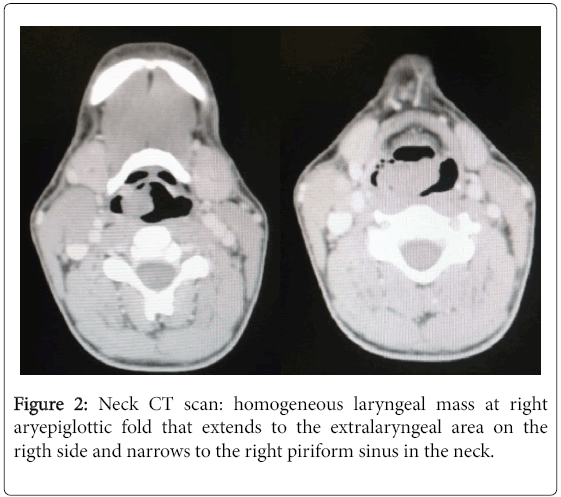
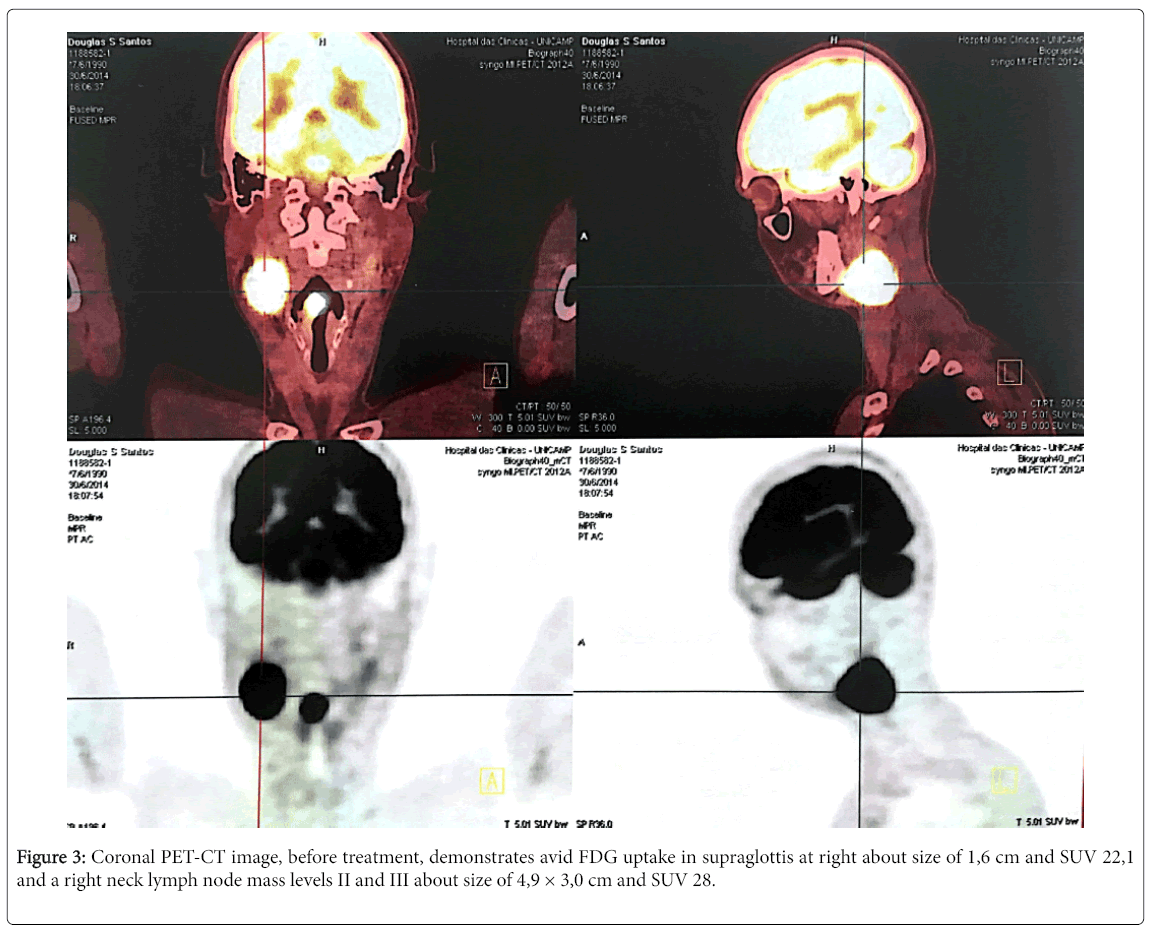
Computed tomography imaging (Figure 2) had any specific characteristic that could distinguish from any larynx mass. Also, noted a cervical lymph node right level II measuring 3.9 × 3.0 × 2.2 cm. A PET-CT was performed showing only this supraglottic mass and neck lymph node at right as we can see in Figure 3.
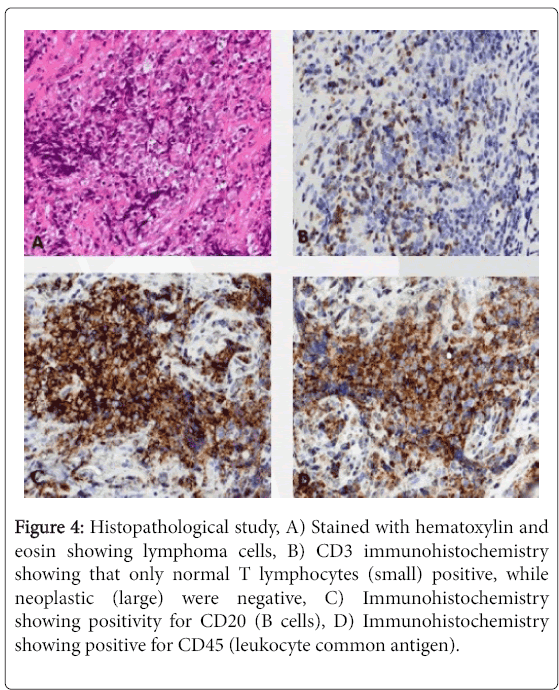
Under general anesthesia, the patient underwent direct microlaryngoscopy for endoscopic biopsy. Fragmented tissue biopsies measuring 0.5 × 0.5 cm in diameter were received. Histologically, the tumor resulted in non-Hodgkin`s large B cell lymphoma with high proliferative index (Figure 4). Immunohistochemistry it was positive for CD45, CD20, CD10, BCL6, Ki67 and negative for AE1AE3, CD3 and Bcl2 (Table 1).
Figure 4: Histopathological study, A) Stained with hematoxylin and eosin showing lymphoma cells, B) CD3 immunohistochemistry showing that only normal T lymphocytes (small) positive, while neoplastic (large) were negative, C) Immunohistochemistry showing positivity for CD20 (B cells), D) Immunohistochemistry showing positive for CD45 (leukocyte common antigen).
| S. No. | Immunostaining | |
|---|---|---|
| 1 | AE1AE3 | Negative for neoplastic cells, positive internal control. |
| 2 | CD45 | Positive for neoplastic cells. |
| 3 | CD3 | Negative for neoplastic cells, positive internal control. |
| 4 | CD20 | Positive for neoplastic cells. |
| 5 | CD10 | Strongly diffuse positive. |
| 6 | Bcl2 | Negative for neoplastic cells, positive internal control. |
| 7 | Bcl6 | Weakly diffuse positive. |
| 8 | Ki67 | Strongly diffuse positive. (80% of neoplastic cells) |
Table 1: Details of the immunostaining and hybridization: Immunohistochemistry.
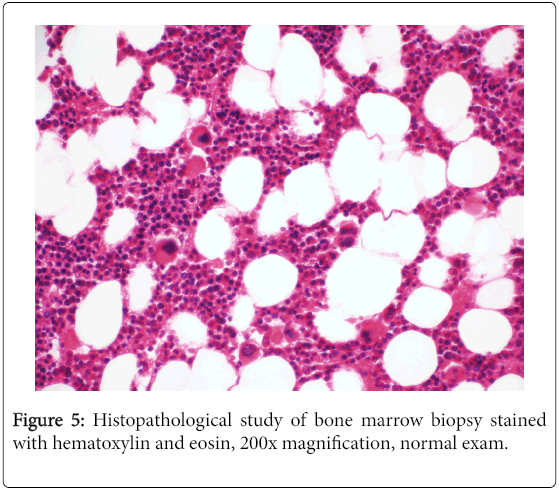
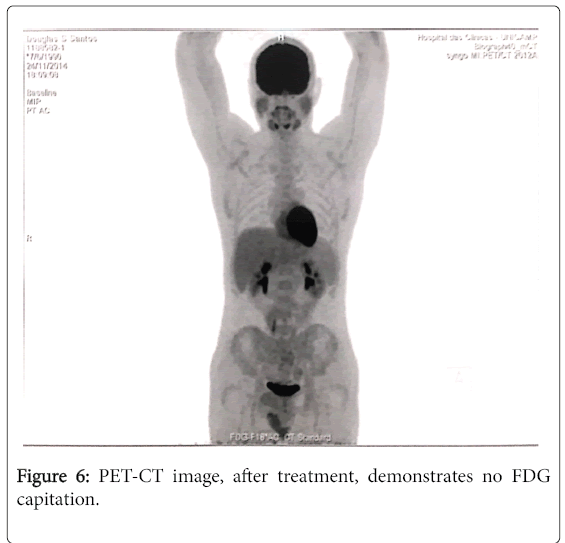
The patient was referred to the hematology service for specific treatment. After a negative bone marrow biopsy (Figure 5), he was given three cycles of R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) and after sessions of chemotherapy with no complications he was considered free from disease. In control examination, there were no signals of the lesion and no complains. A PET-CT (Figure 6) was performed six months after treatment and there were no more lesions.
Discussion
Non-Hodgkin's lymphoma (NHL) is the second most common hematologic tumor in the larynx, after plasmacytoma [5]. The diagnosis is a challenge, since patients present with unspecific symptoms such as dysphonia, dysphagia and odynophagia and, initially, lymphadenopathy and other systemic symptoms such as fever, night sweats and weight loss are not present [1,4].
Male are more affected than female and the age at onset range from 4 to 81 years, with the mean age of occurrence to be the seventh decade [6,7]. Initial symptoms include hoarseness, dysphagia, globus sensation, stridor, or systemic signs, such as weight loss and fever. Laryngeal lymphomas tend to remain localized for a long period without progress of symptoms. Chemotherapy and radiation therapy are the most common therapeutic strategies advocated worldwide for laryngeal lymphoma treatment.
Supraglottis is the main larynx site of primary NHL Lymphomas because it contains follicular lymphoid tissue [1,8]. Diffuse large B-cell and mucosa associated lymphoid tissue (MALT)-type marginal zone B-cell lymphomas are the most commonly found primary laryngeal hematopoietic neoplasms [1,3]. Other types of lymphomas, such as Tor natural killer (NK)-cell lymphomas, have rarely been reported. [1,9-13].
Computed tomography (CT) imaging show that lymphoma usually are tumors with homogeneous enhancement after intravenous contrast injection [3]. A large nonnecrotic supraglottic lesion with a submucosal component that demonstrates homogeneous enhancement is more characteristic of lymphoma than of squamous cell carcinoma. Laryngeal lymphoma is commonly seen to extend into the hypopharynx, but it can also be isolated to the supraglottis. Cervical lymphadenopathy, a common finding in supraglottic squamous cell carcinoma, is seen in a smaller percentage of patients with laryngeal lymphoma [2].
In recent years, the advent of new technologies that allow the subtyping and the understanding of molecular mechanisms, such as PCR and gene sequencing has allowed the identification of molecular signaling pathways and drug targets. Thus, added to the usual treatment of NHL, consisting of radiotherapy and/or chemotherapy, new therapies such as monoclonal antibodies like rituximab [5].
Conclusion
The diagnosis of NHL laryngeal is a challenge to the otolaryngologist, since, usually, patients present with nonspecific complaints and no systemic signs suggestive of this condition. Computed tomography can demonstrate nonspecific homogenous enhancement and nasofibrolaryngoscopy has no specific features. Direct biopsy makes the diagnosis.
It is an important consideration in the differential diagnosis of laryngeal tumors, as lymphoma is treated with chemoradiation instead of surgery.
References
- Markou K, Goudakos J, Constantinidis J, Kostopoulos I, Vital V, et al. (2010) Primary laryngeal lymphoma: Report of 3 cases and review of the literature. Head Neck 32: 541-549.
- Siddiqui NA, Branstetter BF 4th, Hamilton BE, Ginsberg LE, Glastonbury CM, et al. (2010) Imaging characteristics of primary laryngeal lymphoma. AJNR Am J Neuroradiol 31: 1261-1265.
- Horny HP, Kaiserling E (1995) Involvement of the larynx by hemopoietic neoplasms. An investigation of autopsy cases and review of the literature. Pathol Res Pract 191: 130–138.
- King AD, Yuen EH, Lei KI, Ahuja AT, Van Hasselt A (2004) Non-Hodgkin lymphoma of the larynx: CT and MR imaging findings. AJNR Am J Neuroradiol 25: 12-15.
- Dunleavy K, Wilson WH (2014) Appropriate management of molecular subtypes of diffuse large B-cell lymphoma. Oncology (Williston Park) 28: 326-334.
- Ansell SM, Habermann TM, Hoyer JD, Strickler JG, Chen MG, et al. (1997) Primary laryngeal lymphoma. Laryngoscope 107: 1502-1506.
- Kato S, Sakura M, Takooda S, Sakurai M, Izumo T (1997) Primary non-Hodgkin's lymphoma of the larynx. J Laryngol Otol 111: 571-574.
- Andratschke M, Stelter K, Ihrler S, Hagedorn H (2005) Subglottic tracheal stenosis as primary manifestation of a marginal zone B-cell lymphoma of the larynx. In Vivo 19: 547–550.
- Marianowski R, Wassef M, Amanou L, Herman P, Tran-Ba-Huy P (1998) Primary T-cell non-Hodgkin lymphoma of the larynx with subsequent cutaneous involvement. Arch Otolaryngol Head Neck Surg 124: 1037–1040.
- Chan JK, Sin VC, Wong KF, Ng CS, Tsang WY, et al. Nonnasal lymphoma expressing the natural killer cell marker CD56: A clinicopathologic study of 49 cases of an uncommon aggressive neoplasm. Blood 89: 4501–4513.
- Hadjileontis CG, Kostopoulos IS, Kaloutsi VD, Nikolaou AC, Kotoula VA, et al. (2003) An extremely rare case of synchronous occurrence in the larynx of intravascular lymphoma and in situ squamous cell carcinoma. Leuk Lymphoma 44: 1053-1057.
- Mok JS, Pak MW, Chan KF, Chow J, Hasselt CA (2001) Unusual T- and T/NK-cell non-Hodgkin's lymphoma of the larynx: A diagnostic challenge for clinicians and pathologists. Head Neck 23: 625-628.
- Pak MW, Woo JK, Van hasselt CA (1999) T-cell non-Hodgkin's lymphoma of the larynx and hypopharynx. Otolaryngol Head Neck Surg 121: 335-336.
Citation: Junior NT, Zago TM, Pauna HF, Crespo AN (2017) Non Hodgkin Lymphoma in Supraglottis: Case Report. Otolaryngol (Sunnyvale) 7:285. DOI: 10.4172/2161-119X.1000285
Copyright: © 2017 Junior NT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7277
- [From(publication date): 0-2017 - Aug 17, 2025]
- Breakdown by view type
- HTML page views: 6305
- PDF downloads: 972