Case Report Open Access
Odontogenic Pansinusitis Complicated by Orbital Cellulitis, Epidural Empyema and Intracerebral Abscess of Fronto-basal Region: Case Report
Anna Yu. Poghosyan1*, Ruben V. Fanarjyan2, Voskehat S. Nersisyan1, Grigori A. Harutyunyan3 and Arman N. Zakaryan PhD2
1Department of Maxillofacial and ENT Surgery, University Hospital, Yerevan, Armenia
2Department of Neurosurgery, University Hospital, Yerevan, Armenia
3Department of Diagnostic Radiology, University Hospital, Yerevan, Armenia
- Corresponding Author:
- Dr. Anna Yu. Poghosyan
13 Avag Petrosyan Str., 18 apt
Yerevan, Armenia
Tel: (+374 91) 474 169
E-mail: anna.yu.poghosyan@gmail.com
Received date: July 23, 2014; Accepted date: September 11, 2014; Published date: September 17, 2014
Citation: Poghosyan AY, Fanarjyan RV, Nersisyan VS, Harutyunyan GA, Zakaryan AN (2014) Odontogenic Pansinusitis Complicated by Orbital Cellulitis, Epidural Empyema and Intracerebral Abscess of Fronto-basal Region: Case Report. J Interdiscipl Med Dent Sci 2:149. doi: 10.4172/2376-032X.1000149
Copyright: © 2014 Poghosyan AY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Sinusitis is a relatively common problem, which still can be complicated by intracranial and orbital involment. Intracranial abscesses are uncommon, serious, neurological condition associated with significant morbidity and mortality. A case report of sinusitis, complicated by orbital cellulitis, epidural empyema and intracerebral abscess is presented. The patient was successfully treated by emergency surgical intervention including Coldwell-Luke sinusotomy with perforation of the roof of maxillary sinus, ethmoidotomy, left sided lateral supraorbital craniotomy with perforation of the orbital roof, accompained by parenteral antibiotic administration and tight postoperative observations by CT monitoring.
Keywords
Complicated sinusitis; Orbital cellulitis; Epidural empyema; Intracerebral abscess
Abbreviations
CT : Computerized Tomography; PNS: Paranasal Sinusis; POD: Postoperation Day
Introduction
Sinusitis is a relatively common problem, which still can be complicated by intracranial and orbital involvement. Intracranial abscesses are uncommon, serious, neurological conditions associated with significant morbidity and mortality [1]. These include brain abscess and subdural or epidural empyemas and are classified according to the anatomical location or the etiologic agent [2]. Subdural and epidural empyemas accounting for approximately 20-33% of all intracranial infections [3]. The majority occur in the setting of sinusitis, have a fulminant clinical course, and require prompt diagnosis and emergent neurosurgical intervention [4-6]. Dental infection as a cause of epidural abscess is rare compared to other forms of intracranial suppurations [7]. Morbidity and mortality are minimized by early diagnosis, which is best made using computed tomography scanning, and proper therapy, which consists of surgical drainage and administration of appropriate antimicrobials [8].
Case Report
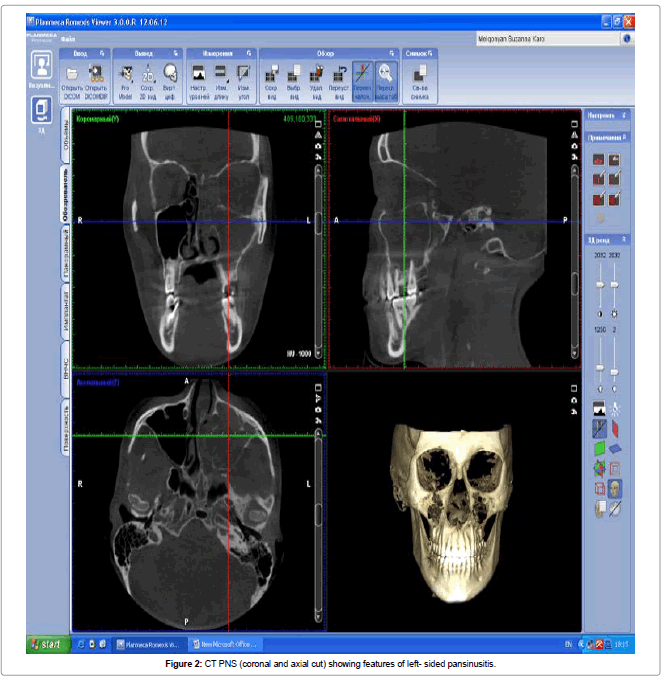
A 22-year-old female was referred to the department of ENT and Maxillofacial Surgery of “Heratsy’№1 University Hospital on December 2013 with severe edema of the left eyelid, inability to open the left eye, headache and high grade fever within the last three days. She gave a history of recurrent episodes of headaches with left-sided foul smelling anterior nasal discharge of yellowish color for 2 years duration following the left upper second molar endodontic treatment. 3 months prior to admission she had a toothache from the same tooth. On clinical examination there was a left- sided exoftalm with severe upper eyelid edema, conjuctival congestion and chemosis (Figure 1). Movements of left eyeball were restricted in all directions, but visual acuity was within normal limits. Diffuse swelling of left fronto-temporal and buccal region was present and left frontal, ethmoid and maxillar sinuses were tender on palpation. There were no signs of meningeal irritation or any neurological deficits. Initial blood analyses showed no pathological changes. CT scan of PNS showed left-sided pansinusitis (Figure 2).
Emergent the Caldwell -Luc sinusotomy with ethmoidotomy was performed. There were significant number of polyps and very foul smelling pus in maxillary and ethmoidal sinuses. After cleaning of sinuses a small perforation approximately 6-7 mm in diameter was performed in upper wall of the maxillary sinus in projection of retrobulbar area for evacuation of the pus. The causative tooth was extracted. Active irrigation with antiseptics (Betadine, Dioxidine) was performed and wide drainage tube was placed in maxillary sinus without suturing. Empirical antibacterial treatment was initiated with Ceftriaxone and Metronidazol.
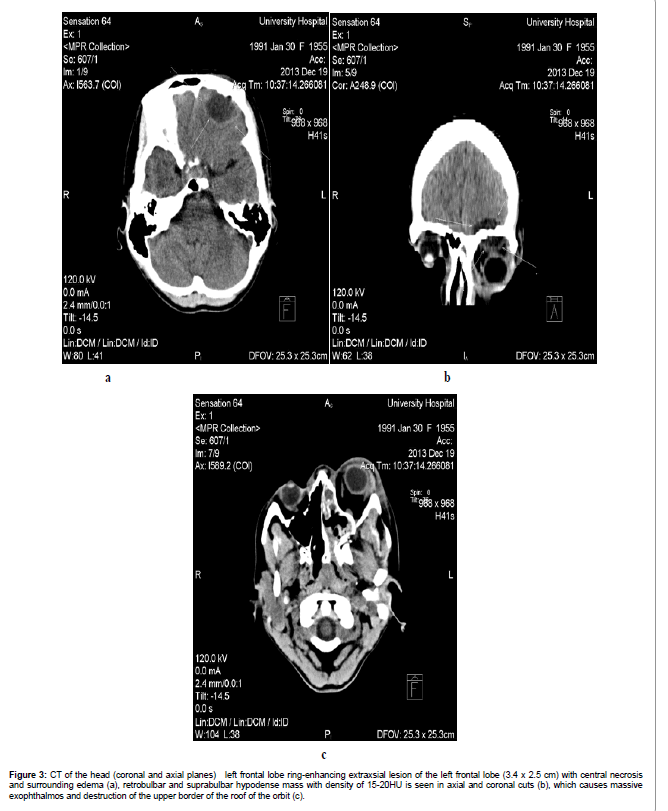
In second POD a follow-up CT scan was performed (Figure 3ac). A ring enhancing extra-axial mass of the left frontal lobe with the dimensions of 3.4 x 2.5 cm with central necrosis and surrounding edema was observed on axial cut (Figure 3a). Retrobulbar and suprabulbar hypodense lesion with density of 15-20HU was seen on axial and coronal planes, which was causing significant massive exophthalmos and destruction of the upper border of orbital roof (Figure 3b and c). Destruction of the orbital roof was also noted (Figure 3b).
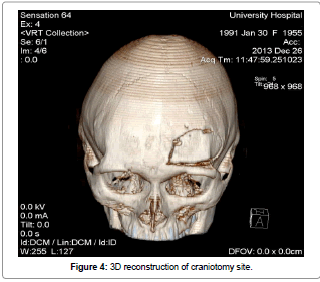
At the same day the left sided lateral supraorbital craniotomy was performed by neurosurgeons to reach the left orbital roof, frontal sinus and frontobasal region of the brain. The patient was positioned supine. The head was turned 30º to the right with minimal flexion, and was fixed with a three- pins Mayfield head frame. A curvilinear incision was made behind the hairline. The skin was opened in one layer fashion (skingalea- pericranium-muscle) and was retracted with 3 spring hooks. The bone flap was measured 4-5 cm x 3 cm. The epidural empyema was washed, and the supraorbital abscess was removed through a bur hole placed on the roof of the left orbit. The left frontal sinus was opened widely, cleaned with curettes, and closed with bone wax to prevent a possible liquorrhea. The dura of the left frontobasal region was opened, and the brain abscess was removed and drained (Figure 4).
Figure 3:CT of the head (coronal and axial planes) left frontal lobe ring-enhancing extraxsial lesion of the left frontal lobe (3.4 x 2.5 cm) with central necrosis and surrounding edema (a), retrobulbar and suprabulbar hypodense mass with density of 15-20HU is seen in axial and coronal cuts (b), which causes massive exophthalmos and destruction of the upper border of the roof of the orbit (c).
Cultures of the fluid collected from maxillary sinus and epidural empyema fluid revealed the growth of Streptococcus spp. The medication was changed to intra-venous Moxitec 400 mg q.d., Metronidazole 500 mg t.i.d., Fraxiparin 0.3 q.d subcutaneously and enhanced detoxication therapy (0.9% NaCl, 4% KCL, Iono- tech etc.).
Irrigation of maxillary sinus t.i.d. was performed through the drainage tube of placed inside maxillary sinus. 3% Hydrogen peroxide, Dioxidine, 0.12 % Chlorhexidine gluconate were used for irrigation purposes. Moxicin eye drops was used 5 times per day and Solcoseril eye gel 3 t.i.d.. This regimen was maintained for 1 week. Beginning from the second week Moxitec and Metronidazole were discontinued and Sulfperazone was prescribed b.i.d. with Mannitol q.d. intravenously for 3 weeks. Periodicaly blood analysis were performed with monitoring of the sodium and potassium. Gradual clinical and radiological improvement was observed. On 15-th POD oro-maxillary communication was closed by suturing.
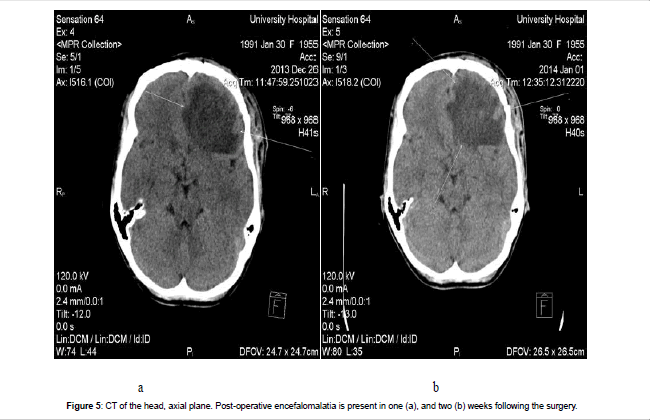
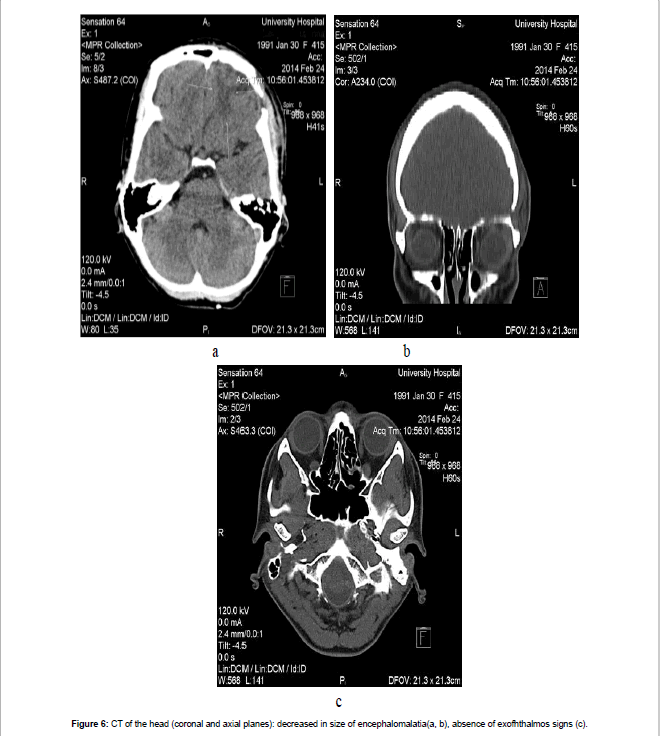
Lesion dynamics and postoperative brain edema, which was strongly pronounced within first two postoperative weeks due to encephalitis were monitored weekly using CT (Figure 5a and b). Follow up examinations revealed a gradual reduction of edema`s size until its resolution in 8 weeks following the admission (Figure 6a-c).
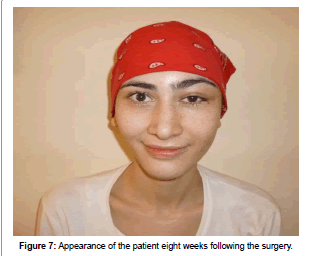
At the end of 8 weeks the patient was discharged. External examination was showing a slight asymmetry because of the left upper eyelid residual edema (Figure 7). The patient has no complains, neurological deficits or visual problems.
Discussion
Sinusitis is a relatively common problem encountered by an otorhinolarygologist. Despite the advent of newer antibiotics, diagnostic procedures and recent advances in management, it still precipitates with life-threatening intracranial complications [4,9]. The suppurative complications of sinusitis can be divided into intracranial and orbital. Orbital complications include preseptal cellulitis, orbital cellulitis with/ without abscess formation and cavernous sinus thrombosis [10]. They present with periorbital oedema, chemosis, visual loss, restricted eye movement, and proptosis. The latter three findings help to differentiate orbital infections from preseptal cellulitis, which is confined to structures anterior to the orbit [11]. Orbital complications of sinusitis and intracranial infection coexist in up to 45% of cases. Therefore, patients exhibiting orbital signs should undergo cranial imaging [12]. Intracranial complications of paranasal sinusitis constitute true surgical and medical emergencies [13]. Morbidity and mortality are minimized by early diagnosis, which is best made with computed tomography scanning, and proper therapy, which consists of surgical drainage and administration of appropriate antimicrobials [8]. The intracranial complications of paranasal sinusitis include subdural empyema, epidural abscess, intracerebral (intraparenchymal) abscess, meningitis, cavernous sinus thrombosis and thrombosis of other venous sinuses. It is not uncommon for a patient to exhibit more than one focus of infection—intracranial or orbital, or both [14,15]. Most cases of sinusitis are uncomplicated and occur in the outpatient setting. Overall, sinus disease is the presumed underlying cause of about 10% of intracranial suppuration [12,14,15].
Subdural empyema, however, is much more strongly associated with underlying sinusitis and is also the most common sinusitisassociated intracranial infection [13].
Epidural empyemas tends to remain localized within the extradural space. It can be recognized on noncontrast CT scans as a lens-shaped lesion of low density adjacent to the inner plane of the skull. The skull may show evidence of prior trauma or surgery, focal osteomyelitis, or permeation by infection. Contrast-enhanced CT shows enhancement of the inner dural layer of the collection. Mass effect with effacement of sulci, ventricular compression, and ventricular displacement may be present [16].
Most symptoms are a result of the size and location of the spaceoccupying lesion or lesions.
The triad of fever, headache (often severe with lateralization towards the side of the abscess), and focal neurological deficit occurs in less than half of patients. It is important to note that fever is absent in over 50% of patients with brain abscess at the time of the initial presentation [17,18].
Brain abscess is one of the most serious diseases of the central nervous system. This condition is more common among men--twice to three times, and morbidity rate is highest in fourth decade of the life. The development of the brain abscess can resulted from the spread of infection from local sites or blood -borne from distal sites. In 10-15% of cases multiple abscesses develop. Headache is the most common symptom. The radiologic tests: computed tomography or magnetic resonance are tests of choice in diagnosis and monitoring of treatment [19].
Routine laboratory studies are not helpful for the diagnosis of brain abscess. Up to 40% of patients have a normal peripheral white blood cell count. Acute-phase reactants are moderately helpful but nonspecific [20].
Decision about therapeutic methods depends on number, size and localization of lesions and patient's condition. In conservative treatment empirical antibiotic therapy and supportive treatment are used. Currently two methods of surgical treatment are used: CTguided stereotactic aspiration and evacuation of the brain abscess by craniotomy [19,21-23].
Once an abscess has formed, surgical excision or drainage combined with prolonged antibacterial therapy (usually 4-8 weeks) remains the treatment of choice. Some neurosurgeons advocate complete evacuation of the abscess, while others advocate repeated aspirations as indicated [22]. Small abscesses and lesions in the stage of cerebritis respond well to medical therapy alone [24]. However, emergency surgical drainage of the epidural abscess or subdural empyema and any underlying sinusitis should be done [9]. Weekly or biweekly CT scans to monitor the size of the abscess are, however, mandatory following aspiration, and repeated aspirations may be required [25] Craniotomy is also recommended for multiloculated abscesses and larger lesions with significant mass effect that are superficial and located in noneloquent regions of the brain [21,26]. The goals of surgical intervation are decompression of brain and complete evacuation of pus. Vision impairment, as well as worsening of periorbital erythema or edema, proptosis and restriction of eye movement and lack of response to an initial trial of appropriate antibiotics is absolute indications for surgical drainage. The route of surgical drainage is determinate by localization of the orbital abscess. Endoscopic orbital decompression or external approach can be employed. In addition, definitive management of infected sinuses should be done preferably at the same time [11,27].
When the predisposing condition is a contiguous focus of infection, such as paranasal sinusitis, otitis media, or dental abscess infection, it is usually polymicrobial (>50%-60% of cases), particularly if culture specimens from the brain abscess are cultured optimally on anaerobic media. Aerobic streptococci, staphylococci, gram-negative organisms, and anaerobic organisms, including anaerobic and microaerophilic streptococci have been reported as the causative agents [28].
Initial empiric antimicrobial therapy should be based on the expected etiologic agents according to the likely predisposing conditions, the primary infection source, and the presumed pathogenesis of abscess formation. When abscess specimens are available, staining of the material can help guide in selection of medical therapy. Whenever proper cultures are taken and organisms are isolated and their susceptibility is determined, the initial empiric therapy can be adjusted to specifically treat the isolated bacteria [26].
Third generation cephalosporins and metronidazole offers broad coverage and good brain-blood barrier and abscess penetration [9]. If adjacent osteomyelitis is present, prolonged intravenous therapy for a minimum duration of 6 to 8 weeks should be considered [13].
If not recognized early, both epidural empyema and brain abscess can be fatal. A delay in surgical drainage and decompression can be associated with high morbidity and mortality.
Conclusion
Paranasal sinusitis can on rare occasions lead to serious, potentially life-threatening orbital and intracranial complications. Early diagnosis with aggressive medical and surgical management can lead to improved outcome. We present a case of odontogenic pansinusitis, complicated with orbital cellulitis, epidural empyema and brain abscess, which was successfully treated by emergency surgical intervention including sinusotomy and craniotomy accompanied by parenteral antibiotic administration and careful postoperative CT monitoring.
References
- Shotelersuk V, Goyal M., Rauchenstein JN., Konez O (2001) Subdural empyema secondary to odontogenic masticator space abscess: Detection by indium-111-labeled white cell scan. Journal of Clinical Imaging 25: 18-22.
- Nathoo N, Nadvi SS, van Dellen JR., Gouws E(1999) Intracranial subdural empyemas in the era of computed tomography. A review of 699 cases.Neurosurgery 44: 529-535
- Danziger A., Price H., Schechter MM (1980) An analysis of 113 intracranial infections. Neuroradiology 19: 31-34.
- Dolan RW, Chowdhury K (1995) Diagnosis and treatment of intracranial complications of paranasal sinus infection. J Oral Maxillofac Surg 53:1080-1087.
- Gallagher RM, Gross CW, Phillips CD (1998) Suppurative intracranial complications of sinusitis. Laryngoscope 108:1635-1642.
- Kaufman D.M., Litman N., Miller M.H (1983)Sinusitis: induced subdural empyema. J Neurology 33:123-132.
- Kanu OO, Ukponmwan E, Bankole O, Olatosi JO, Arigbabu SO (2011) Intracranial epidural abscess of odontogenic origin.J NeurosurgPediatr 7:311-315.
- Sellick JA Jr (1989) Epidural abscess and subdural empyema.J Am Osteopath Assoc89: 806-810.
- Vaydyanathan V. Shetty K (2011) Intracranial and orbital complications of sinusitis: a case series and review of literature. Clinical rhinology; An International Journal4: 87-92.
- Goldberg AN, Oroszlan G., Anderson TD (2001) Complications of frontal sinusitis and their management. OtolaryngolClin North Am 34: 211-225.
- Osborn M.K., Steinberg J.P (2007) Subdural empyema and other suppurative complications of paranasal sinusitis. Lancet Infect Dis 7: 62-67.
- Jones N.S., Walker JL., Bassi S., Jones T., Punt J (2002) The intracranial complications of rhinosinusitis: can they be prevented? Laryngoscope 112:59-63.
- Clayman GL, Adams GL, Paugh DR, Koopmann CF. Jr (1991) Intracranial complications of paranasalsinusistis: a combined institutional review. Laryngoscope 101: 234-239.
- Giannoni CM., Stewart MG., Alford E (1997) Intracranial complications of sinusitis. Laringoscope 107:863-867.
- Singh B, Van Dellen J., Ramjettan S., Maharaj TJ (1995) Singenic intracranial complications. J LaringolOtol 109: 945-950.
- Pereira JL, Carvalho GT, Borgo MC (2010) Epidural empyema relating to dorsal myiasis. Rev Soc Bras Med Trop 43: 345.
- Mathisen GE, Johnson JP (1997) Brain abscess. Clin Infect Dis 25:763-779.
- Ronald AR (1980) Rarer Infectious Diseases. CanFamPhisician26:395-397
- Kalinowska-Nowak A, Garlicki A, Bociaga-Jasik M (2009) Brain abscess--modern diagnostics and therapeutic treatment. PrzeglEpidemiol 63: 89-95.
- Osenbach RK, Loftus CM (1992) Diagnosis and management of brain abscess. NeurosurgClin N Am 3:403-420.
- Bernardini GL (2004) Diagnosis and management of brain abscess and subdural empyema. CurrNeurolNeurosci Rep 4: 448–456.
- Kocherry XG, Hegde T, Sastry KV, Mohanty A (2008) Efficacy of stereotactic aspiration in deep-seated and eloquent-region intracranial pyogenic abscesses. Neurosurg Focus 24: E13.
- Mampalam TJ, Rosenblum ML (1988) Trends in the management of bacterial brain abscesses: a review of 102 cases over 17 years. Neurosurgery 23:451–458.
- Townsend GC, Scheld W (1998) Infections of the central nervous system. AdvInt Med 43:403–440.
- Sharma BS, Gupta SK, Khosla VK (2000) Current concepts in the management of pyogenic brain abscess. Neurol India 48:105–111.
- Mamelak AN, Mampalam TJ, Obana WG, Rosenblum ML (1995) Improved management of multiple brain abscesses: a combined surgical and medical approach. Neurosurgery 36:76–86.
- Vairaktaris E, Moschos MM, Vassiliou S, Baltatzis S, Kalimeras E, et al. (2009) Orbital cellulitis, orbital subperiosteal and antroorbital abscess. Report of three cases and review of literature. J CraniomaxillofacSurg 37:132-136.
- Brennan MR (1995) Subdural empyema.AmFam Physician 51: 157-162.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 18284
- [From(publication date):
December-2014 - Aug 24, 2025] - Breakdown by view type
- HTML page views : 13527
- PDF downloads : 4757