Oral Carcinoma, HPV Infection, Arsenic Exposure-their Correlation in West Bengal, India
Received: 22-Sep-2016 / Accepted Date: 05-Oct-2016 / Published Date: 12-Oct-2016 DOI: 10.4172/2161-119X.1000266
Abstract
Objective: The aim is to find out any possible correlation between HPV infection and oral carcinoma along with this metal toxicity. Methods: Ethical clearance for this study was obtained from the Ethics Committee of Vivekananda Institute of Medical Sciences, Ramakrishna Mission Seva Pratishthan. Patients attending our hospital were screened for the presence of oral premalignant and malignant lesions. The subjects were administered a standard questionnaire. The buccal swab and hair samples (107 cases and 50 controls) were collected after obtaining informed consent from all the corresponding subjects, and were analysed for detection of HPV 16 DNA and arsenic level analysis, respectively. Results: 22.5% of malignant samples showed the presence of HPV 16 DNA. 80% of cases showed their arsenic count above the safe limit (0.8 μg/g). Conclusion: A considerable percentage of malignant samples showed the presence of HPV16 DNA, indicating that there may be a correlation between HPV infection and oral malignancy in this population. A higher percentage of cases showing an elevated arsenic count states a possible link between arsenic toxicity and the development of this disease. However, a higher population size and statistical analysis are required for a proper conclusion.
Abbreviations
HPV: Human Papilloma Virus; OSCC: Oral Squamous Cell Carcinoma; OM: Oral Malignant; OPM: Oral Premalignant; PBS: Phosphate Buffer Saline; SD: Standard Deviation; As: Arsenic
Introduction
Otosclerosis is a primitive osteodystrophy of endochondral layer of the otic capsule. It is responsible for conductive hearing loss and sometimes mixed hearing loss. Clinical incidence varies from 0.1 to 2% worldwide. In Tunisia, its prevalence ranges from 0. 4% to 0.8% [1]. Its therapeutic management is most often the fate of the surgery which aim is usually to correct conductive component of deafness. It is therefore necessary for functional surgery patient prognosis. A significant hearing improvement is achieved in most surgical patients. However, a small proportion of patients may have persistent or recurrent deafness and sometimes signs of labyrinthisation. Imaging then finds its indications. The CT scan is realized in first intention, completed with MRI if radio-clinical discrepancy or labyrinthisation signs [2]. The purpose of this study is to review the role of postoperative imaging and to illustrate the main causes of surgical failures and post-operative complications of otosclerosis.
Materials And Methods
This was a retrospective study on patients diagnosed with otosclerosis that received surgery (stapedectomy or stapedotomy) attended at the otology department of La Rabta Hospital between 1995 and 2015. A post-operative clinical assessment was made of all the patients at two months, six months and every one year after surgery. Persistent or recurrent hearing loss, tinnitus or vertigo was noticed. Postoperative audiometry was performed at 3, 6, 9, 12, 18 and 24 months and then annually. Air conduction (AC), bone conduction (BC), post-operative air bone gap (ABG) and net decibel (dB) gain of each ear was detected. Tonal audiometry of AC and BC was undertaken at frequencies of 500, 1.000 and 2.000 Hz. Hearing improvement was defined as air-bone gap closure to 10 dB or less and/or AC improvement of 20 dB or more. CT scan was performed when surgical failure or labyrinthine complication were suggested. The temporal bone CT Scan was performed using a 64 channels multidetector scanner General Electric GE. The exploration was conducted in the standard axial plan with helicoidal technique and volumetric acquisition (120 kv, 200 mA, rotation time of 0.5 s, thickness of the section of 0.5 mm, matrix 512 × 512). The head of the patient was located in a neutral position and the time of study was of 4 to 6 s. The data analysis was performed in an Advantage® work station. The temporal bones were visualized in three basic plans (axial, sagital and coronal), reconstructed in isometric way (with the same resolution as the original acquisition) every 0.6 mm. In addition, there were performed 2D reconstructions multiplanar and oblique curves, and Maximum Intensity Projections (MIP), according to the structure of clinical interest or as the findings: Ossicular chain, round and oval windows, the cochlea, vestibular aqueduct, semi-circular canals and facial nerve canal.
MRI was performed using a GE 1.5 Tesla or Siemens 3Telsa system. The following scan parameters were used for the T2-weighted TSE sequence (FOV 130 × 130 × 24 mm, 0.6 mm isotropic voxels, TR/TE/TSE factor 2400 ms/200 ms/73 and 80 sections, resulting in an acquisition time of approximately 6 min) 3D Volumetric CISS in axial plan with coronal and sagittal reformation and MIP reconstruction. Oblique sagital reformatted images in perpendicular plan to 7th and 8th nerve in internal auditive conducts were performed.
Imaging records were retrospectively evaluated by a senior radiologist, and radiology resident. Statistical analyses were performed with software package: Statistical Package for the Social Sciences. Clinical and audiological data were correlated to CT and MRI findings. These correlations were analyzed with linear and binary logistic regression model (Pearson test): p-value<0.05 was considered to indicate a statistically significant difference.
Results
A total of 326 patients diagnosed with otosclerosis that received surgery were initially identified from the department of otology clinical records. Thirty five of 326 (10.7%) had developed post-operatively clinical symptoms suggested surgical failure or labyrinthine complication. Fourteen patients were operated bilateraly a total of 49 ears; 7 (20 %) were males and 28 (80%) were females (sex ratio=0.25). Their ages were between 24 years and 80 years; the mean age was 49.7 years. Patients were underwent stapedotomy with vein graft interposition and reconstruction with either a Teflon piston in 14 cases (29%), a bucket handle prosthesis in 23 cases (47%), or a total prosthesis in 12 cases (24% ).
Surgical Failure
Surgical failures were noticed in 28 ears (57%). They were an early procedural failure (<6 months) in four cases and a failure occurred during follow-up in 24 cases over a period ranging from 6 months to 26 years with a mean of 7.8 years.
Clinical data
In this group of patients, the hearing loss was the most the commonest presenting symptoms described in 25 cases (89% of failure). In three cases, it was persistent deafness in early postoperative (less than three months). In the remaining 22 cases (79%), there was a recurrence of deafness after a temporary improvement postoperative period, which was of variable duration ranging between 1 and 26 years. Tinnitus was found in 21 cases (75%), always associated with one or more other clinical features. Vertigo was found in three cases (11%). In one case, it appeared in immediate postoperative period.
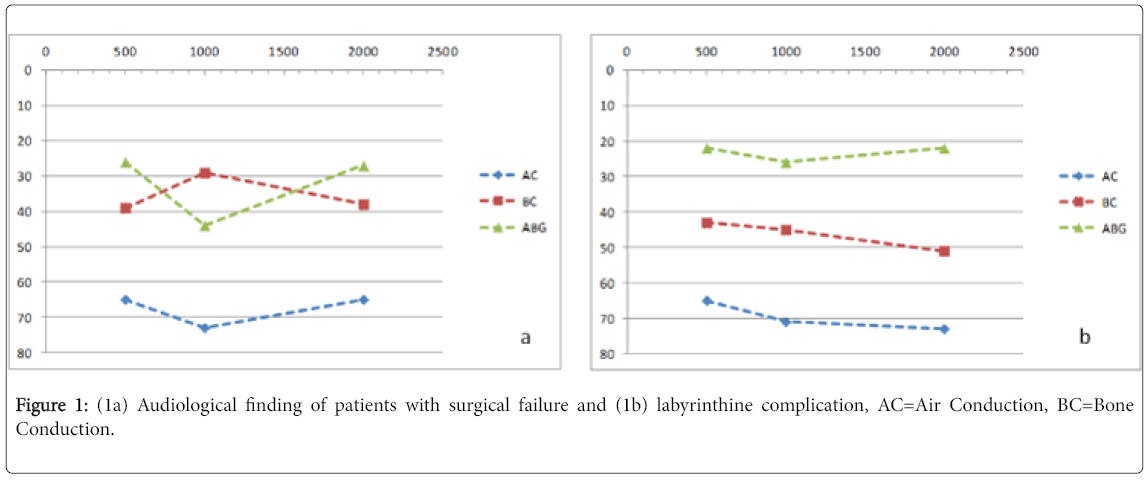
Audiological finding (Figure 1a)
In 4 cases (14%), hearing loss was developed in early postoperative. They were about, in all cases, conductive type. The ABG was about 41.1 dB. In late post-operative, we noticed 21 cases of mixed hearing loss, 2 cases of conductive type, 1 case of sensorineural hearing loss and no cases of postoperative deafness. The ABG was about 45.7 dB.
CT finding
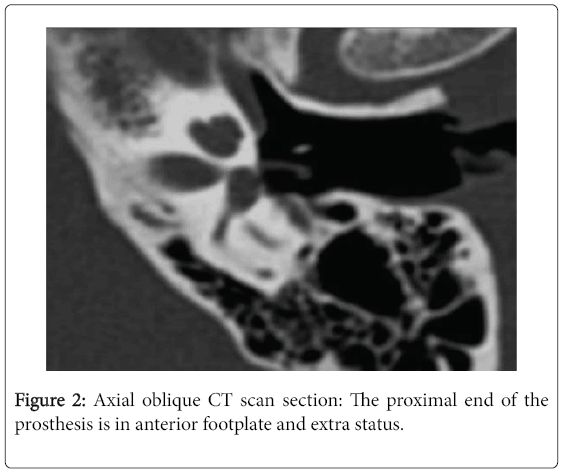
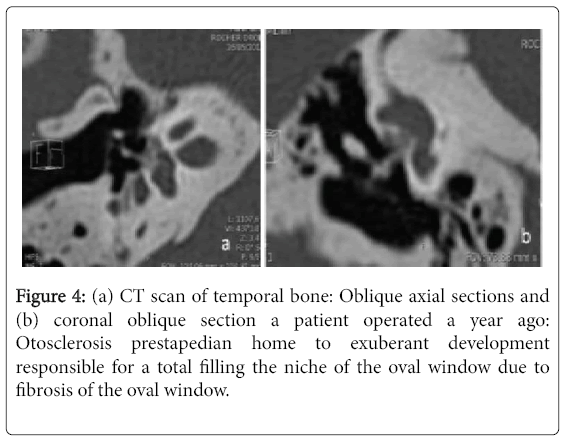
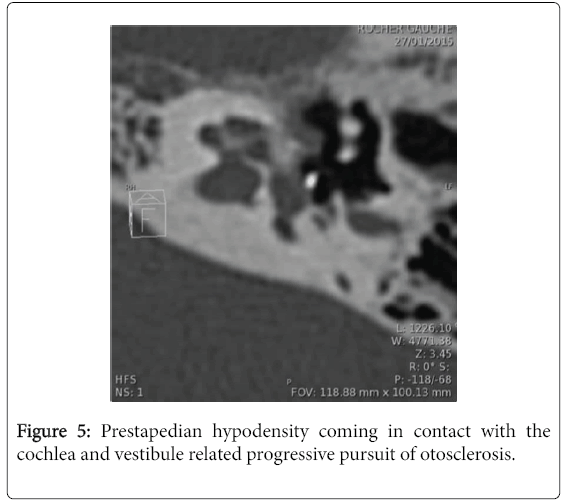
The deadline for completion of the CT scan in late post-operative period and during follow-up was variable with an average of 8.1 years and extremes ranging from 9 months to 26 years. In the latter case, the scanner was indicated for mixed hearing loss progressively worsening with associated vertigo. The dose length product (DLP) averaged 571 milli gray (mGy) per centimeter with a range of 420-1213. Surgical failure was due to erosion of the long process of the incus in four cases (14%), incudo-mallear dislocation in one case (4%) and displacement of the prosthesis in 11 case (39%): Five cases of displacement of the lateral end of the prosthesis from the uncus, two cases of disconnected medial end (Figure 2) and four cases of complete dislocation of the prosthesis (Figure 3). In two case, CT showed a hypodensity of the ovale window due to fibrosis in one case (Figure 4) and a short prosthesis with a medial end does not comes into contact with the oval window in the other case. Progression of otosclerosis (Figure 5), compared to pre-operative imaging, was noticed in 13 cases (46%) associated with displacement of the prosthesis in three cases. No abnormalities were raised only in one CT scan.
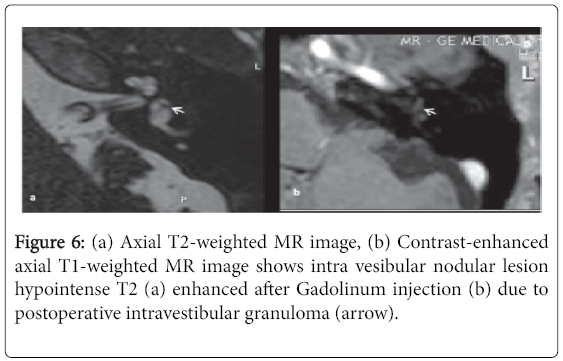
MRI finding
MRI was performed in only two patients within a period not exceeding three months after practicing scanner. It was motivated by the result of CT showing a fibrosis of the oval window and a progression of otosclerosis with the presence of an exuberant hypodensity making suspect of an intravestibular extension. In the first case, no abnormality was raised. In the second case, MRI showed intra vestibular nodular lesion hypointense T2 enhanced after Gadolinum injection due to granulation tissue (Figure 6).
Labyrinthine complication
In 21 ears (43%) labyrinthine complications were retained. In these cases, patients showed signs of functional use in a subsequent period ranging from one to 21 years and an average of 6.6 years.
Clinical finding
Tinnitus was found in 8 cases (29%), associated in all cases with one or more other clinical symptom. Vertigo was found in 10 cases (36%). The hearing loss was described in 14 cases (50%). In the all cases, there was a recurrence of deafness after a temporary improvement over an average period of 7.3 years.
Audiological finding (Figure 1b)
In early postoperative, all patients of this group had ABG between 10 and 15 dB. We only collected the audiological data having been suspected diagnosis of labyrinthine complication, which was occurred after a mean of 6.6 years. During follow-up, 14 patients developed deafness: mixed type (12 ears), conductive hearing loss (1 ear) and sensorineural hearing loss (1 ear).
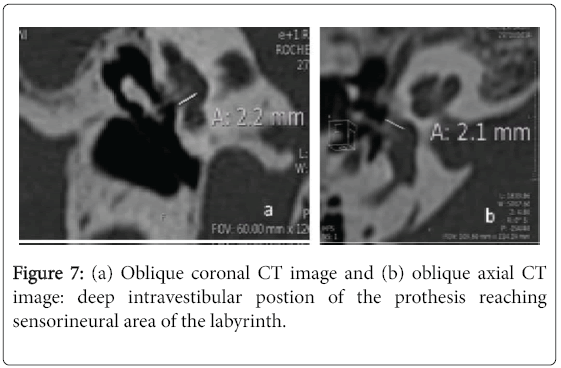
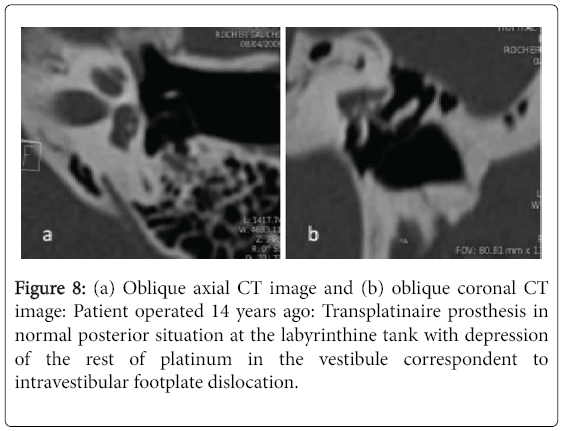
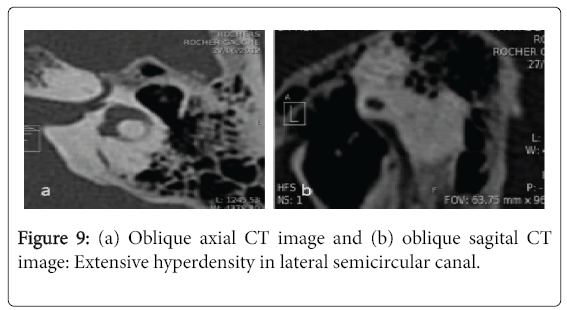
CT finding
In this group, the dose length product (DLP) averaged 665 milli gray (mGy) per centimeter with a range of 398-1242. CT showed a deep intavestibualr position of the medial end of the prosthesis exceeding the external half of the vestibule in 15 cases (71%) (Figure 7). In two cases CT showed a focal hyperattenuation in the vestibule one case due to intravestibular footplate dislocation (Figure 8). An extensive hyperattenuation in lateral semicircular canal was noticed in one case consistent with labyrinthine ossificans (Figure 9).
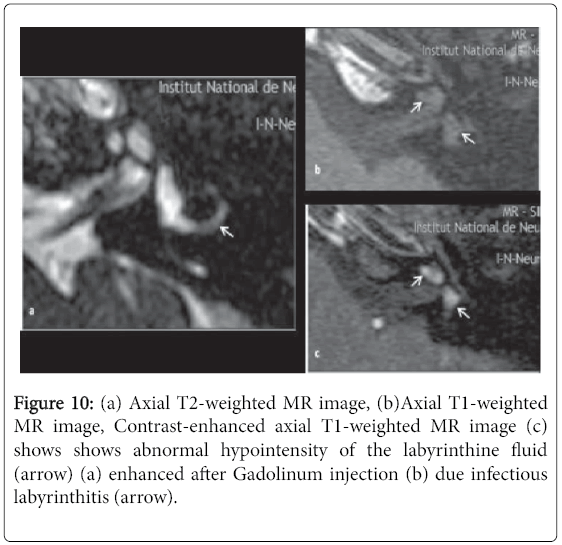
MRI Finding
In only three cases, MRI was performed. In two cases, no abnormalities were raised in CT scan conducted in first-line. MRI was requested to complement the research of any other cause that may explain the functional symptoms described showing an infectious labyrinthitis (Figure 10) in one case and no abnormalities in the other case. In the third case, the patient complained of recurrent hearing loss and vertigo. MRI confirmed perilymphatic fistula suspected on CT.
Discussion
The essential limitations of our study was the small number of patients included in our study and the lack of correlation of imaging results to the results of the surgery Failures and complications affect less than 10% of patients operated on for otosclerosis. Recurrent hearing loss or deafness after a period of improvement hearing is the most common symptom described in 91% of cases on average in the literature [3,4]. Persistent deafness has been described in average 21%. Tinnituses are associated in all cases reviewed in the literature [3] to another functional symptom. Recurrent deafness is often conductive type, but most often it degrades to become mixed type and even deafness. This evolution is variable over time with deadlines that can go up to 7 years and over in the literature [5]. Vertigo is infrequent and is only present in 10 to 20.1% of cases in literature [6]. In our study, hearing loss was found in 79% and vertigo in 25%. It was a recurrent hearing loss in 54.4%. The failures are the most common reasons for revision surgery. These failures are due to a displacement of the prosthesis, the progression of otosclerosis, lysis/erosion of the descending branch of uncus, fibrosis of the oval window and incudomallear dislocation. Several studies [7-11] examined the causes of failures found at the post-operative CT scan. Table 1 summarized their results comparing to our findings [11-15]. The labyrinthine complications are less common causes of revision surgery. The main causes of labyrinthine suffering are secondary to migration of the prosthesis from the center portion of the oval widow, peri-lymphatic fistula, reparative granuloma extending into the vestibule, labyrinthitis or bleeding intra-vestibular. Table 2 summarized their results comparing to our findings [9,10,16-18]. The results of our series were comparable with previously published studies. On suspicion of failure or post-operative complication, clinical and audiometric results conclude in some cases in suffering or a labyrinthine destruction without any etiological specificity. CT and MRI are extremely useful in the etiological diagnosis. Based on clinical results, audiometric and the imaging findings, retaining conclusion of complications and failures of the primary surgical treatment of otosclerosis may require medical treatment cochlear support and/or vestibular, recovery surgical or hearing aid fitting [19,20]. However, several studies have reported that the CT scan data were not always correlated with operative findings, especially in case of lysis of uncus or fibrosis of the oval window [21]: Ayache et al. about 26 cases of revision surgery, showed a discrepancy between the conclusions of the radiologist and surgeon observations in 50% of cases while the correlations were excellent in 37.5% of cases and partial in 12.5% of cases. However, the helical acquisition techniques and MPR reconstruction, which were not used in this series, significantly improve the reliability of imaging and used to dictate the surgical procedure or take medical treatment. Moreover, according to some articles [10,22], simple erosion of uncus, frequently observed during surgical revision regardless of the type of prosthesis is usually not detected on CT.
| Han, et al. [16] | Wiet, et al. [10] | Lesinski[7] | Betsch,et al. [9] | Lippy,et al. [5] | Our study | |
|---|---|---|---|---|---|---|
| n=74 | n=1147 | n=279 | n=73 | n=49 | ||
| Displacement of prosthesis | 17.5 | 45 | 81 | 37.1 | 58.1 | 24 |
| Lysis/Erosion of uncus | 43.2 | 23.6 | 31 | 8.5 | - | 8 |
| Progression of otosclerosis | 24.3 | 10.5 | 13.5 | 7.1 | - | 20 |
| Fibrosis of oval window | 44.6 | 2.9 | - | 32.8 | 2.7 | 2 |
| Uncudo-mallear dislocation | - | 0.8 | 4 | 5.7 | - | 4 |
| Short prosthesis | 20.3 | 4.5 | 5 | 5.7 | - | 0 |
Table 1: Underlying causes of surgical failures of our study comparing to litterature (p. 100).
| Han, et al. [16] | Wiet, et al. [10] | Shea, 1998 [18] | Lesinski[7] | Betsch, et al. [9] | Our study | |
|---|---|---|---|---|---|---|
| n=74 | n=1147 | n=308 | n=279 | n=73 | n=49 | |
| Peri-lymphatic fistula | 5.4 | 10 | 2 | 5.4 | 5.7 | 2 |
| Intravestibular protrusion of prosthesis | 1.4 | 0.4 | 0.8 | 2 | 5.7 | 22 |
| Reparative granuloma extending into the vestibule | - | 2.3 | 0.4 | - | 5.7 | 2 |
| Labyrinthitis | - | - | - | - | - | 4 |
| Floating platinium | - | - | 0.8 | - | - | 2 |
Table 2: Underlying causes of labyrinthine complications of our study comparing to litterature (p. 100).
Conclusion
To ensure maximum efficiency in the postoperative monitoring and the management of complications and post-operative failures, the clinician is required to take into account both the functional findings, results audiometric and radiological data. However, in some cases during the postoperative period, imaging may be insufficient in the search for an etiology for the patient's symptoms. In the future, technological advances in imaging and the confrontation between the imaging data and operative findings should help increase the reliability of imaging.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Consent Statement
As our article is a retrospective study and did not publish any personal photo or information regarding any of the patient in our manuscript thus the consent is not required for the article publication.
References
- Chaturvedi AK, Anderson WF, Lortet-Tieulent J, Curado MP, Ferlay J, et al. (2013) Worldwide trends in incidence rates for oral cavity and oropharyngeal cancers.J ClinOncol 31: 4550-4559.
- Rakesh S, Janardhanan M, Vinodkumar RB, Vidya M (2010) Association of human papilloma virus with oral squamous cell carcinoma-A brief review.Oral & Maxillofacial Pathology Journal 1: 1-9.
- Jamaly S, Khanehkenari MR, Rao R, Patil G, Thakur S, et al. (2012) Relationship between p53 overexpression, human papillomavirus infection, and lifestyle in Indian patients with head and neck cancers. TumourBiol 33:543-550.
- Navarro Silvera SA, Rohan TE (2007) Trace elements and cancer risk: a review of the epidemiologic evidence.Cancer Causes Control 18: 7-27.
- GuhaMazumder DN (2008) Chronic arsenic toxicity & human health.Indian J Med Res 128: 436-447.
- Su C, Lin Y, Chang T, Chiang C, Chung J, et al. (2010) Incidence of oral cancer in relation to nickel and arsenic concentrations in farm soils of patients’ residential areas in Taiwan.Bio Med Central Public Health 10:67.
- Patra M, Halder A, Bhowmick N, De M (2005) Use of black tea in modulating clastogenic effects of arsenic in mice in vivo, West Bengal, India.Journal of Environmental Pathology, Toxicology and Oncology 24: 201-210.
- Chakraborti D, Das B, Rahman MM, Chowdhury UK, Biswas B, et al. (2009) Status of groundwater arsenic contamination in the state of West Bengal, India: a 20-year study report.MolNutr Food Res 53: 542-551.
- Bui TC, Tran LT, Markham CM, Huynh TT, Tran LT, et al. (2015) Self-reported oral health, oral hygiene, and oral HPV infection in at-risk women in Ho Chi Minh City, Vietnam.Oral Surg Oral Med Oral Pathol Oral Radiol 120: 34-42.
- Young D, Xiao CC, Murphy B, Moore M, Fakhry C, et al. (2015) Increase in head and neck cancer in younger patients due to human papillomavirus (HPV). Oral Oncol51: 727-730.
- Chawla JP, Iyer N, Soodan KS, Sharma A, Khurana SK, et al. (2015) Role of miRNA in cancer diagnosis, prognosis, therapy and regulation of its expression by Epstein-Barr virus and human papillomaviruses: With special reference to oral cancer. Oral Oncol51: 731-737.
- Sun Y, Zhang Y, Liu L, Song X, Li G (2015) Genetic polymorphisms and HPV infection in oral squamous cell carcinomas.CurrOpinVirol 14: 1-6.
- Anderson KS, Dahlstrom KR, Cheng JN, Alam R, Li G, et al. (2015) HPV16 antibodies as risk factors for oropharyngeal cancer and their association with tumor HPV and smoking status.Oral Oncol 51: 662-667.
- Gupta S, Gupta S (2015) Role of human papillomavirus in oral squamous cell carcinoma and oral potentially malignant disorders: A review of the literature.Indian J Dent 6: 91-98.
- Reyes M, Rojas-Alcayaga G, Pennacchiotti G, Carrillo D, Muñoz JP, et al. (2015) Human papillomavirus infection in oral squamous cell carcinomas from Chilean patients.ExpMolPathol 99: 95-99.
- Li Y, Wang YB, Gou X, Su YB, Wang G (2006) Risk assessment of heavy metals in soils and vegetables around non-ferrous metals mining and smelting sites, Baiyin, China.J Environ Sci18: 1124-1134.
- Ghosh P, Basu A, Mahata J, Basu S, Sengupta M, et al. (2006) Cytogenetic damage and genetic variants in the individuals susceptible to arsenic-induced cancer through drinking water. Int J Cancer 118: 2470-2478.
- Saha JC, Dikshit AK, Bandyopadhyay M, Saha KC (1999) A review of arsenic poisoning and its effects on human health. Critical Reviews in Environmental Science and Technology 29: 281-313.
- Das D, Samanta G, Mandal BK, Roy Chowdhury T, Chanda CR, et al. (1996) Arsenic in groundwater in six districts of West Bengal, India.Environ Geochem Health 18: 5-15.
- Yuan TH, Lian IB, Tsai KY, Chang TK, Chiang CT, et al. (2011) Possible association between nickel and chromium and oral cancer: a case–control study in central Taiwan. Sci Total Environment 409:1046–1052.
- Kazi TG, Wadhwa SK, Afridi HI, KaziN, Kandhro GA, et al. (2010) Interaction of cadmium and zinc in biological samples of smokers and chewing tobacco female mouth cancer patients. J Hazard Mater 176:985–991.
- Su CC, Lin YY, Chang TK, Chiang CT, Chung JA, et al. (2010) Incidence of oral cancer in relation to nickel and arsenic concentrations in farm soils of patients’ residential areas in Taiwan. BMC Public Health.
- Kazi TG, Wadhwa SK, Afridi HI, Kazi N, Kandhro GA, et al. (2010) Evaluation of cadmium and zinc in biological samples of tobacco and alcohol user male mouth cancer patients.Hum ExpToxicol 29: 221-230.
- Feki-Tounsi M, Olmedo P, Gil F, Khlifi R, Mhiri MN, et al. (2013) Cadmium in blood of Tunisian men and risk of bladder cancer: interactions with arsenic exposure and smoking.Environ SciPollut Res Int 20: 7204-7213.
Citation: Pal P, Halder A (2016) Oral Carcinoma, HPV Infection, Arsenic Exposure-their Correlation in West Bengal, India. Otolaryngol (Sunnyvale) 6:266. DOI: 10.4172/2161-119X.1000266
Copyright: © 2016 Pal P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11996
- [From(publication date): 10-2016 - Aug 18, 2025]
- Breakdown by view type
- HTML page views: 11096
- PDF downloads: 900