Case Report Open Access
Overlap Syndrome (Systemic Sclerosis and Rheumatoid Arthritis) with Achalasia: An Unusual Association
Daniel Ruiz-Romero*, Alicia Sofia Villar-Chavez, Miguel Angel Valdovinos-Diaz and Enrique Coss-Adame
The National Autonomous University of Mexico, Mexico
- *Corresponding Author:
- Dr. Daniel Ruiz Romero
Specialist in Internal Medicine
The National Autonomous University of Mexico
Mexico
Tel: 525570342850
E-mail: daniel_ruizch@hotmail.com
Rec date: Feb 24, 2016; Acc date: May 5, 2016; Pub date: May 12, 2016
Citation: Ruiz-Romero, Villar-Chavez, Valdovinos-Diaz, Coss-Adame (2016) Overlap Syndrome (Systemic Sclerosis and Rheumatoid Arthritis) with Achalasia: An Unusual Association. J Gastrointest Dig Syst 6: 426. doi:10.4172/2161-069X.1000426
Copyright: © 2016 Ruiz-Romero D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Both patients with achalasia and systemic sclerosis can complain of esophageal dysphagia. Esophageal manometer remains the most accurate method to evaluate esophageal dismotility. The association of achalasia and systemic sclerosis as an overlap syndrome has not been described yet. This entity could be possibly based on common autoimmune mechanisms and an analogous pathogenesis explained mainly by viral association.
Keywords
Systemic sclerosis; Overlap syndrome; Achalasia
Introduction
Patients with some features of systemic sclerosis in combination with manifestations of other rheumatic diseases, such as systemic lupus erythematosus, dermatomyositis, or rheumatoid arthritis, are considered to have an overlap syndrome [1]. Ninety percent of patients with systemic sclerosis have gastrointestinal involvement, being esophageal disease the most common source which is detected by esophageal manometry that remains the most accurate method to evaluate esophageal motor function [2]. Patients complain of heartburn and dysphagia, due to gastroesophageal reflux and to impaired hypomotility of the distal esophagus or occasionally secondary to strictures. The etiology of systemic sclerosis is still unknown. Exposure to viruses or certain toxins may lead to variable disease expression in genetically susceptible hosts. In some individuals, genetic factors may be sufficiently strong to lead to disease expression [3].
Primary achalasia is characterized by loss of peristalsis in the distal esophagus and a failure of lower esophageal sphincter (LES) relaxation and main complaint is esophageal dysphagia [4]. Main finding in achalasia on high-resolution manometry is an impaired esophagogastric junction relaxation defined as a mean four-second integrated relaxation pressure (IRP) =15 mmHg [5].
Both achalasia and systemic sclerosis are associated with esophageal dysphagia as one of the main gastrointestinal manifestation. In the literature there are two cases reported in patients with systemic sclerosis and achalasia; however, these cases were documented only through esophagogram without performing esophageal manometry [6,7]. We present a well-documented case of systemic sclerosis and achalasia.
Case Report
A 77-year-old mexican woman was admitted to our hospital because of complaining of joint pain in hands, knees and ankles; Raynaud's phenomenon; sharp face, reduced opening mouth, telangiectasia in face, skin thickening, sclerodactylia, hyperpigmentation in arms and limitation to flexion hands about 21 years of evolution. Five years ago was diagnosed with hypothyroidism. Her past medical history included use of low dose glucocorticoids at the beginning (10 mg/day of prednisone during six weeks); later she also received omeprazole 20 mg/day with partial response and was changed to pantoprazole 40 mg/day, hydroxychloroquine 400 mg/day and levothyroxine 100 mcg/day. Currently she is taking just the last two drugs since three years ago. She also began with esophageal dysphagia both to solids and liquids in last two years.
Laboratory data revealed: antinuclear antibodies (ANA) speckled pattern 1:5120, ANA Centromere pattern 1:5120, Scl-70 antibodies positive, rheumatoid factor positive. Total leukocytes: 3,600/mm3, Neutrophils 2,500/mm3, hemoglobin 13.5 g/dl, platelets 128/mm3, erythrocyte sedimentation rate 41 mm/h, urinalysis: negative.
She was assessed by rheumatologist who made the diagnosis of overlap syndrome because she had data of both, systemic sclerosis and rheumatoid arthritis.
Approach to dysphagia was initially done with upper endoscopy that showed a dilated and sigmoid esophagus along with multiple raised white plaques >2 mm, edema, hyperemia and no ulceration; these findings were suggestive of esophageal candidiasis graded as Kodsi II classification.
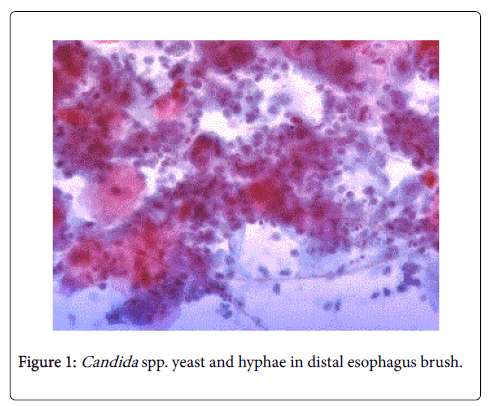
The endoscope was advanced through gastro esophageal junction without difficulty, allowing revising all stomach and duodenum until second portion that showed normal findings. Besides, brushing esophageal mucosa was performed showing Candida spp. yeast and hyphae (Figure 1).
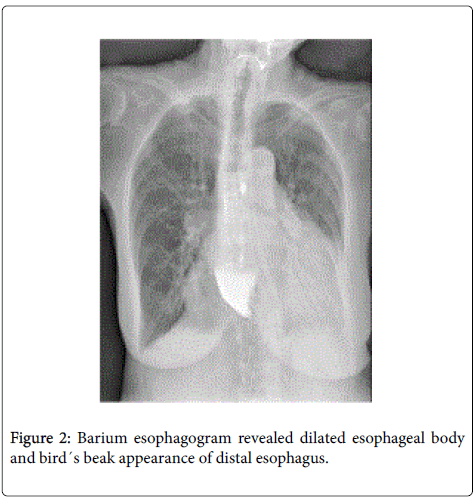
Also, a barium esophagogram revealed dilated esophageal body and bird´s beak appearance of distal esophagus (Figure 2).
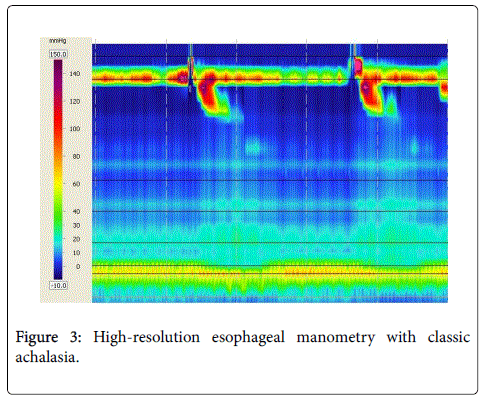
High-resolution esophageal manometer was performed with the following findings: 100% failed peristalsis, distal contractile integral (DCI): 0 mmHg.s.cm, IRP 38 mmHg, LES pressure 47.2 mmHg. The diagnosis of type I achalasia (classic achalasia) was established (Figure 3). With all these data the final diagnosis was overlap syndrome (systemic sclerosis and rheumatoid arthritis) with classic achalasia.
The patient was assessed for esophageal surgeon and gastroenterologist. On March 1st 2016 a Heller myotomy with Dor fundoplication was done; dysphagia had a partial response after procedure. She continues taking levothyroxine 100 mcg/day, pantoprazole 40 mg/day and hydroxychloroquine 400 mg/day. She will be follow up as outpatient by rheumatologist and gastroenterologist very soon.
Discussion
One hallmark symptom of both achalasia and systemic sclerosis is esophageal dysphagia, so it is important to recognize the need for esophageal function testing in the initial evaluation of dysphagia (endoscopy, reflux monitoring and manometer) in both entities. This is because it is well recognized that, in genetically predisposed individuals, an autoimmune response to an unknown inciting agent, perhaps a viral infection, can be the trigger factor [8].
In patients with systemic sclerosis which manifests with dysphagia the manometric findings consist of absent or ineffective distal esophageal peristalsis and hypotensive LES. Motility studies have shown that 40% of patients with abnormal motor activity of the esophagus are asymptomatic [9]. In achalasia there are 3 distinct types. All 3 types are characterized by incomplete LES relaxation, but they differ in pressurization patterns and presence of spastic contractions. Type I is called classic achalasia (absent pressurization), type II is achalasia with panesophageal pressurization and type III is spastic achalasia [10]. It is important to know that these two entities and perform motility studies, because medical treatment is different for each one.
This is the first case that shows the association between achalasia and overlap syndrome (systemic sclerosis and rheumatoid arthritis), where achalasia was evidenced by high-resolution esophageal manometry.
References
- Van den Hoogen F, Khanna D, Fransen J, Johnson SR, Baron M, et al. (2013) 2013 classification criteria for systemic sclerosis: an American college of rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis 72:1747.
- Thoua NM, Bunce C, Brough G, Forbes A, Emmanuel AV, et al. (2010) Assessment of gastrointestinal symptoms in patients with systemic sclerosis in a UK tertiary referral centre. Rheumatology (Oxford) 49: 1770.
- Hamamdzic D, Harley RA, Hazen-Martin D, LeRoy EC (2001) MCMV induces neointima in IFN-gammaR-/-mice: intimal cell apoptosis and persistent proliferation of myofibroblasts. BMC MusculoskeletDisord 2:3.
- Vaezi MF, Pandolfino JE, Vela MF (2013) ACG clinical guideline: Diagnosis and management of achalasia. Am J Gastroenterol 108:1238.
- Kahrilas PJ, Ghosh SK, Pandolfino JE (2008) Esophageal motility disorders in terms of pressure topography: the Chicago Classification. J ClinGastroenterol 42:627.
- Nomoto T, Kikuchi T, Kusunoki Y, Akesaka K, Yano K, et al. (2010) Acute right heart failure and achalasia-like syndrome in a patient with limited cutaneous systemic sclerosis and primary biliary cirrhosis. Intern Med 49:1779-1182.
- Garrigues V, Ponce J, Gálvez C (1996) Achalasia-like syndrome as the first manifestation in a patient with CREST syndrome. Eur J GastroenterolHepatol8: 289-291.
- Gyawali CP
- Carlson DA, Hinchcliff M, PandolfinoJE (2015) Advances in the Evaluation and Management of Esophageal Disease of Systemic Sclerosis. CurrRheumatol Rep 17: 475.
- Van Hoeij FB, Breadboard AJ (2016) Clinical Application of Esophageal High-resolution Manometry in the Diagnosis of Esophageal Motility Disorders. J NeurogastroenterolMotil 22: 6-13.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 13212
- [From(publication date):
June-2016 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 12202
- PDF downloads : 1010