Pole Exercise Causes Body Changes in Physical Flexibility and Exercise Function
Received: 27-Dec-2017 / Accepted Date: 23-Jan-2018 / Published Date: 25-Jan-2018 DOI: 10.4172/2165-7025.1000377
Abstract
Background: Theoretical mode of spinal stability and core stability has been introduced previously, which has proceeded to rehabilitative approaches. We have focused on physical flexibility and exercise function, and firstly devised an original pole exercise in sitting position that can be done simply and cost-effectively.
Subjects and Methods: The subjects 11 healthy young adults, 27.0 ± 5.6 years old. Methods included the intervention of pole exercise with Exercise of the thorax, lower thoracic vertebrae and pelvis, upper thoracic vertebrae and pelvis. Before and after the exercise, we investigated examinations. Tests of physical flexibility were Wing Test, Thomas Test, Shoulder Extension Test, straight leg raise (SLR), Body warp prone position, Heel Buttock Distance (HBD) and Finger Floor Distance (FFD). Tests of exercise functions were Back Muscle Strength (BMS), Weight Bearing Index (WBI), Functional Reach Test (FRT) and closed eye leg standing time.
Results: The data of 7 flexibility tests and 4 exercise function tests revealed the significant differences between before and after the pole exercise (p<0.05). These tests would cover detail aspects of several human abilities in physiotherapy.
Discussion and Conclusion: In current study, pole exercise seems to be clinically simple and easy method to perform. These results suggested that pole exercise including 6 movements would have clinical efficacy as to physical flexibility and exercise function in short period. Currently obtained data could become fundamental data for clinical application and research development in the future.
Keywords: Pole exercise; Body changes; Physical flexibility; Exercise function; Vertebrae; Spine curvature
Abbreviation
WBE: Weight bearing exercise; SLR: Straight leg raise; HBD: Heel Buttock Distance; FFD: Finger Floor Distance; BMS: Back Muscle Strength; WBI: Weight Bearing Index; FRT: Functional Reach Test
Introduction
Historically speaking, a new theoretical model has given new inspiration in each era. This situation has been found in also the field of musculoskeletal rehabilitation.
Initially, the discussion had been continued how the central nervous system (CNS) acts on anticipated movement against the stability of the spine and keeps the balance of the body [1]. These findings were reinforced by demonstrating that the stability mechanism will increase its activity proportionally to increases in functional challenge [2]. Subsequently, in order to clarify the stabilization phenomena observed in the body before exercise, EMG has been used [3]. Furthermore, a concept evolution was proposed in which local stability muscles could be separated from the global muscles, and that the different distributions of the outer forces on the body will be managed and explained [4].
In the 1990's, the theory was described about spinal stabilization. Among them, the theoretical model of Panjabi has been widely accepted, and it has become the basis of this area [5].
In other words, Panjabi advocated a revolutionary research at that time [5]. Among them, he summarized the new concept of a theoretical model for spinal stability including three axes of nervous system, active system and passive system. This idea has rapidly developed ideas and treatment models, especially effective for management of low back pain (LBP) [6].
With this model advocacy, LBP revealed problems from patient viewpoint and social viewpoint [7]. Furthermore, in the medical and orthopedic fields, it contributed greatly to the evaluation in the framework of the social psychosocial model [8,9].
After the proposal of Panjabi, the coordination of muscle activity around the lumbopelvic region was reported to be important for the generation of mechanical spinal stability [10,11]. In the light of core stability and stabilization exercise, altered motor control strategies could be a potential cause by several researchers [12,13].
For years, the theory of spinal stability is based on that of Panjabi [5,12]. Spinal stability has consists of three axes, which are passive system, active system and control system [5,12]. Passive system is involved in the control of the movement and stability of the spine by bones, joints and ligaments.
Active system is a function by muscles, and the trunk muscle group which is responsible for the center is roughly classified into two function classifications as inner unit and outer unit [14].The inner unit functions as anchorage of the trunk by applying pressure in the antigravity direction due to tension in the abdominal transverse muscles, the diaphragm, the multifidus muscle, and the pelvic floor muscles [15]. On the other hand, the outer unit is made up of streaks of the surface layer. Its role is to control the balance of motion by linking the trunk and the upper and lower limbs. The outer unit has an anterior oblique system and a posterior diagonal system. The former consists of the connection between the external oblique muscle and the large adductor, and the latter consists of the connection between the wide dorsal muscles and the gluteus maximus [14,15].
Furthermore, control system has the function for the muscle group. By preceding adjoint attitude adjustment, posture is controlled noncontiguously prior to the active muscle [14-16]. These three systems can correlate with each other and acquire spinal stability. In other words, the control system of the upper central organization issues a command to the active system. As a result, it is considered that the spinal joint can move in the neutral zone [15]. Summarized three system together, Lee et al. named the thoracic structure and movement as Thoracic Ring approach, and develop evaluation and treatment [16,17].
In these fields, theoretical and clinical trials have been reported [9], and recent studies include weight bearing exercise (WBE) [18] and curved angles in spinal alignment [19]. Mechanical spinal stability and core stability has been introduced and variously used by clinicians and researches [20]. This has proceeded to some rehabilitative approaches suggesting affecting the neuromuscular control strategies, e.g. stabilization exercise or motor control exercise.
From these background, we have continued sports research [21,22] and focused on physical flexibility and exercise function and continued research [23]. We firstly devised an original pole exercise method that can be done simply and cost-effectively, regardless of the proficiency of the therapist [24]. In this study, we performed the pole exercise to healthy subjects and investigated using physical flexibility tests and exercise function tests.
The hypothesis in this study is that pole exercise including 6 movements would have clinical efficacy as to physical flexibility and exercise function in short period.
Subjects And Methods
The subjects were enrolled 11 healthy adults and the average age was 27.0 ± 5.6 years, 7 males and 4 females. Regarding these backgrounds of the subjects, they were medical staffs in the hospital that cooperated our research as volunteers.
The method includes two projects (Table 1). One is the combination of examination concerning physiotherapy, investigated before and after the intervention performance. The other is a pole exercise performed as an intervention study, which has 6 movements.
| Examination | Before | After | Difference |
|---|---|---|---|
| Physical flexibility tests | |||
| Wing Test (cm) | 16.1 ± 8.9 | 13.3 ± 8.1 | p < 0.05 |
| Thomas Test (cm) | 4.8 ± 5.2 | 3.5 ± 4.7 | p < 0.01 |
| Shoulder Extension Test (°) | 63.5 ± 13.9 | 75.3 ± 13.2 | p < 0.05 |
| Straight Leg Raise (°) | 50.0 ± 12.9 | 58.3 ± 12.0 | p < 0.01 |
| Body warping in prone position (cm) | 39.0 ± 6.8 | 43.8 ± 5.2 | p < 0.01 |
| Heel Buttock Distance (cm) | 2.6 ± 2.7 | 0.5 ± 0.9 | p < 0.01 |
| Finger Floor Distance (cm) | -4.9 ± 9.6 | -1.4 ± 8.6 | p < 0.05 |
| Exercise function tests | |||
| Back Muscle Strength (kg) | 111.9 ± 30.0 | 117.4 ± 29.1 | p < 0.01 |
| Weight Bearing Index | 110.0 ± 16.5 | 127.0 ± 23.3 | p < 0.01 |
| Functional Reach Test (cm) | 37.3 ± 8.7 | 42.6 ± 7.6 | p < 0.05 |
| closed eye one foot standing (sec) | 14.6 ± 10.0 | 20.4 ± 9.5 | p < 0.01 |
Table 1: The changes of data before and after the pole exercise.
General evaluation
We have selected and investigated 11 examinations in order to evaluate the efficacy of pole exercise. The purpose for the examinations has classified into 2 groups.
Former group is for the evaluation for physical flexibility. It has 7 tests such as Wing Test, Thomas Test, Shoulder Extension Test, straight leg raise (SLR), Body warp prone position, Heel Buttock Distance (HBD) and Finger Floor Distance (FFD).
Latter group is for the evaluation for exercise functions tests. It has 4 tests such as Back Muscle Strength (BMS), Weight Bearing Index (WBI), Functional Reach Test (FRT) and closed eye leg standing time.
We measured these tests in the rehabilitation room in the hospital. As for these 11 tests, it took about 15 minutes before and after the pole exercise as an intervention performance.
Specific tests
Specific tests enrolled were 11 tests for physical flexibility and exercise function tests.
1) Wing test: The subject is in a supine positon, raises the upper limits to the utmost position and bend the hip joint and knee joint on one side 90 degrees. After the examiner fixes both shoulder blades, the subject tilts the raised lower limb toward the opposite side. Measure the distance between the inside of the knee joint and the floor by stopping at the final position where the trunk is rotated, the hip joint is inward rolled.
2) Thomas test: The subject is in a supine position, bends the unilateral hip joint, and holds the knee until it reaches the chest. The examiner measures the distance between the popliteal faces on the opposite side and the floor while the knee on one side of the subject is held about the chest.
3) Shoulder extension Test: The subject sits on a sitting position and tilts the trunk forward until the forehead contacts the floor surface From that position, grasp both hands at the back and extend both shoulders to the maximum while extending the elbow. The examiner measures the extension angle of the shoulder against the horizontal line in the subject.
4) Straight leg raise (SLR) test: The subject is in a supine posture. While the examiner grips the subject's unilateral lower limb, subject bends hip joint, with maintaining the knee extension position. The examiner measures the bending angle of the hip joint at the Stretch tightness point in the hamstrings of the subject.
5) Body warp prone position: The subject is in a prone position and warps the body to its fullest extent, with both hands attached to the floor. The examiner measures the distance from the floor to the jaw nearest to the floor as soon as the subject warps the body to the utmost.
6) Hel buttock distance (HBD): The subject is in a prone position. The examiner makes the bending to the maximum extent on one side of the subject's knee. At that point, the examiner measures the distance between the heel and buttocks.
7) Finger floor distance (FFD): The subject stands with his feet about 15 cm apart on the table. The subject let the trunk bend forward as much as possible, with keeping the knees stretched. The examiner measures the distance between the fingertip and the floor of the subject.
8) Back muscle strength (BMS): The subject stands with his feet about 15 cm apart on the table of the back muscle force meter. He grasps the handle of the muscle strength gauge by both hands with the knees stretched. Then tilt your upper body 30° forward with your back stretched out. Pull the handle grasped by both hands while raising the upper body. The examiner performs measurements for 5 seconds, and obtains the single measurement value.
9) Weight bearing index (WBI): WBI measures isometric knee extension muscle force, and μTasF-1 manufactured by Anima Inc. was used. For the subjects, the sensor pads were fixed to the anterior surface of the lower leg and directly above the ankle joint, and the belt was attached to the strut of the posterior crus of the lower leg and the distal part of the lower leg. Subject combines the upper limbs at the front of the trunk, and the examiner instructs to extend the knee for about 3 seconds with maximum force. For measurement, we adopt measurement value of both feet at a time. Then, we calculated the isometric knee extension muscle strength body weight ratio divided by body weight.
10) Functional reach test (FRT): The subject stands comfortably with both feet separated by about 15 cm, grasps the hand lightly, and raises both arms straight upward at 90°. Next, he moves the upper limb as far as possible to the forward without bending both knees. The examiner marks the tip of the first finger that lifted the upper limb upward by 90° and from there it measures the distance to the point reached forward.
11) Closed eye leg standing time: The subject stands with both feet aligned, and the hand crosses in front of the chest. He closes his eyes and lifts one foot upward. The examiner starts measuring from the state where the foot of the subject rises in the air and is stationary. Maximum measurement time is 1 minute, measure only once on both sides.
Device of pole
The device of pole was originated by Moriyasu, which has 160 cm in length and 3.6 cm in diameter, 650 g in weight, made of wood.
We have originated another type of pole which was made of metal for different purpose. This is a new type of pole for exercise, which was divided into 4 pieces. It can be combined for the different length of the pole, which are160 cm, 140 cm, 100 cm and 80 cm in length. The weight of 160 cm pole is 610 g, which is close to the wooden pole.
Outline of pole exercise
This pole exercise has been originated and performed by the authors. It has been used in practice already for opportunities such as treatment and education seminars. Six patterns of movements are included in pole exercise. For these movements, the purpose and expected effects include improving the flexibility of the thorax, adjusting the breathing unit, improving the flexibility of the spinepelvis, improving spinal curvature function, and so on.
Furthermore, important points in practice include performing stretching without force, within the no pain range, conscious of each breathing, not separating a stick away from each body and thinking about the image of general movements of the exercise.
In these movements, subjects always keep 5 seconds each position in right and left side, and repeat 3 times in each movement. Then, the examinations of 6 movements overall took about 6 minutes.
Detail of pole exercise
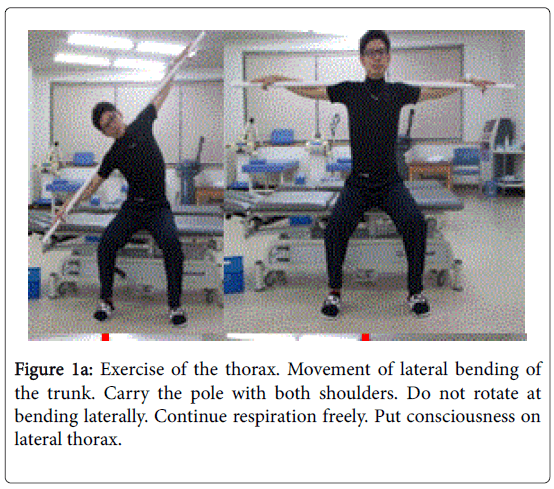
Lateral bending (Figure 1a): The purpose of this movement is to reduce the pain in the shoulder and side flanks, to widen the range of motion of the shoulder joint and thorax, to facilitate breathing and relax the tension around the shoulder blades.
As for the method, while the subject is sitting, it keeps a good posture by stretching a little chest. Next, carry the pole with both shoulders, and remove the power of the shoulders, back and hips. Keep your posture facing the front, and keep your body straight (right) as it is. At that time, on the side of the opposite chest you knocked down (left chest), bend until the point where you feel tension, and hold your posture at this point. At that time, breathe in and out while conscious of the part stretching at the side of the chest (left chest). We will repeat this movement three times in round trip.
There are several points or tips which lead to successful exercise. First of all, the subject feels conscious that the side of the chest on the opposite side spreads out. As soon as you get used to it, keep your consciousness aside and push your body sideways, with the intention of making the pole perpendicular to the ground. In this case, never to defeat by putting strength on the flank. On the contrary, always to pull out the force of the side with lowering your shoulders.
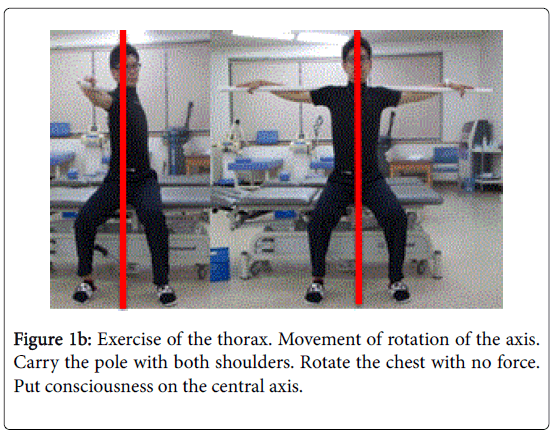
Chest axis rotation (Figure 1b): The purpose of this exercise is to relieve the pain in the shoulder and waist and widen the range of motion of the neck, shoulder, thorax, and spine, to relax the tension in the back and front chest.
As for the method, the subject is sitting, with the straight posture kept in mind. Next, open both feet to the same level as the shoulder width, and carry the pole with both shoulders. Keeping the face facing the front, the subject removes the power of the shoulder and waist, and rotate the body to the left and right. When the right chest rotates forward and the left chest rotates backwards, stop the movement where you feel the tension on the left front chest. At the point, concentrate consciousness on the left chest on stretch, breathe in and out. We will repeat this movement three times in round trip.
There are important points and tips for this movement. When the subject rotates the left chest backwards, try to feel stretching out at left front chest. As soon as you get used to it, attempt to make the navel for the direction of not to the left, but to the forward. When the subject rotates the pole greatly, he feels that the left front chest is greatly stretched. If he can rotate more than 90 degrees from the first posture, it will be even better. Be careful not to turn too far at the waist position when you rotate the body greatly. It is important to turn from the position of chest or breastbone, keeping the face always facing the front. Continue this movement while aiming for a comfortable degree and range, to the extent with feeling a slight pain.
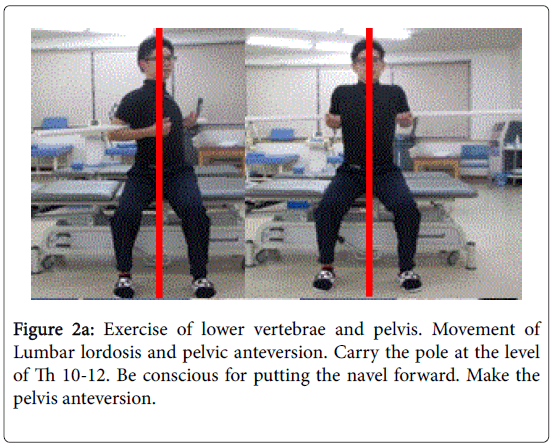
3. Lumbar lordosis and pelvic anteversion (Figure 2a): The purpose of this movement is to promote the physiological lordosis of the lumbar spine and pelvis, reduce the pain in the waist and hip joints, widen the range of motion of the lumbar spine and hip joints, increase the work of the major lumbar muscles and reduce the tightness around the waist.
As for the method, the subject is sitting, with the a little stretch on your chest and a good posture. Bear the pole on the back at the level of epigastrium, and pull out the power of the shoulder and waist. Simultaneously, keep the face for the direction of facing forward, and warps the pelvis and lumbar region. After attempting a posture that warps as much as possible, slowly return to the original position. Perform breathing and rhythm together, repeat 3 round trips.
The important point is to warp the waist and pelvis, with intention to protrude the navel forward. In this case, care should be taken not to strain the muscles of the waist. Breathe when you warp the body, exhale when you return to the original. In this way, if you match the rhythm of exercise and breathing, you can perform this movement smoothly. When you get used to this exercise, try to recover from the warped posture as much as possible, quickly release the tightness of the waist, pull out the force and return it to its original position.
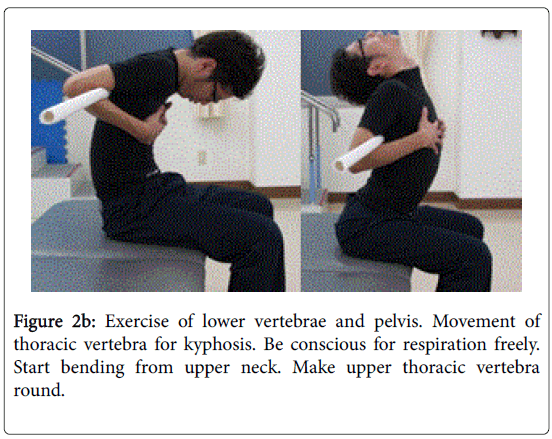
Movement for kyphosis of thoracic vertebra (Figure 2b): The purpose of this movement is to promote the physiological kyphosis of the thoracic vertebrae, to reduce the pain in the scapulae / lumbar region, to widen the range of motion of the thoracic vertebrae / thorax, to facilitate breathing and to reduce the tension around the shoulder blades.
As for the method, the subject is sitting down with a good posture. The subject carries the pole on the back at the level of epigastrium, and lessens the tightness of the shoulder and waist. After that, he rounds the back of the chest, while face keeps facing forward. Try to make round back as much as possible and slowly return to the original position. Repeat this movement 3 round trips, with the accordance rhythm of respiration.
The important point is to gradually roll from the neck and roll the back of the chest. At this time, if the abdominal muscle is tense, the range to be rounded becomes narrower, so the subject will reduce the tension on the abdominal muscles and round the body. The subject exhales when he rounds the back, and inhales when he returns to the original position. In this way, if you match both rhythm, the movement will proceed smoothly. When he is accustomed to this movement, try to be conscious as if each spine becomes to be round.
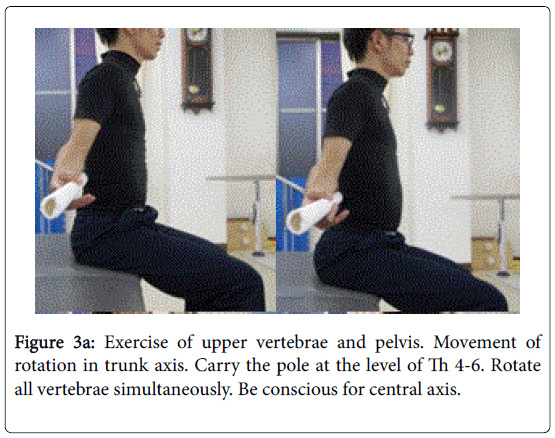
Spine pelvic axis rotation (Figure 3a): The purpose of this exercise is to reduce pain in the neck / shoulder / lumbar region, widen the range of motion of the neck / shoulder band / thorax / spine and reduce the tension in the back and front chest.
As for the method, the subject is sitting down with a good posture. Subject will open their legs to the shoulder width and carry the pole with the back at the height of the nipple. Subject reduces the tightness of the shoulders and hips, and rotate the body to the left and right, keeping the face facing forward.
When the right chest and abdomen are rotated forward, and the left chest and abdomen are rotated backward, stop the movement where you feel the tension on the left chest and abdomen. At that point, concentrate consciousness on the part where the left chest and abdomen were stretched, breathe in and out. Repeat this movement 3 round trips, with the accordance rhythm of respiration.
The important point is to be conscious so that the abdomen is stretched out greatly from the left chest rotated behind. As the subject gets used to it, gradually increase the operation area and increase the degree of the stretch for the chest and abdomen. When turning, try to turn all the spinal column with conscious of existing of the central axis for the body. Continue the movement for adequate range with feeling comfortable while a little bit tension.
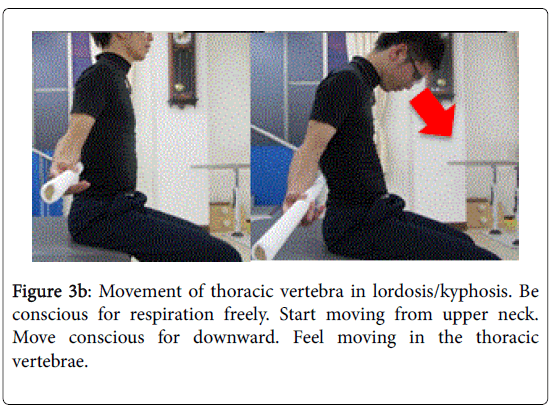
Warp & rounding (Figure 3b): The purpose of this movement is to promote the physiological curvature of the spinal column, to reduce the pain and tightness in the region of neck / chest / abdomen / lower back, and widen the range of motion of the thorax / spine. It reduces the hardness of the abdomen and increases the motive connection between upper body and lower body.
As for the method, the subject is sitting down with a good posture. Open the legs to the shoulder width, carry the pole on the back at the level of nipple, and remove the tightness of the shoulders and waist. With the face facing the front, the subject pivot at the back of the chest with a pole to warp or round the body. He breathes heavily and move back and forth 3 times.
The important point is to eliminate the tension of the whole body, keep your breath away, and move the spine a lot. When the subject gets used to it, be conscious of each spine and enlarge the range and move it. If you he has difficulty to carry it with the height of the papilla, it is safe as the height behind the waist.
Statistical Analyses
In current study, obtained data was shown as the mean ± standard deviation (SD). For statistical analyses, correlation coefficients were calculated using Pearson or Spearman test of the Microsoft Excel analytical tool, which is Four steps Excel Statistics 4th edition [25]. Intergroup comparisons were made using the Wilcoxon rank sum test. A significance level of less than 5% obtained using a two-tailed test was considered to be statistically significant.
Ethical Considerations
Current study was conducted in compliance with the ethical principles of the Declaration of Helsinki and Japan’s Act on the Protection of Personal Information along with the Ministerial Ordinance on Good Clinical Practice (GCP) for Drug (Ordinance of Ministry of Health and Welfare No. 28 of March 27, 1997). No ethical committee meeting was held. Detail explanation was provided to the subjects, and informed consent was obtained from all subjects.
Discussion
There have been lots of discussion concerning the stability of the spine. Three subsystem would be necessary during various postures and movements, which are a passive, an active and a neural control subsystem [5]. Dysfunctional neuromuscular control strategies would result in clinical instability, which means the loss of the ability of the spine to maintain its pattern of displacement [12,26].
Previously, spinal stability has been classified into two along the muscular system of the lumbosacral area involved [4]. One is a local system of muscles which has an origin or insertion directly on the vertebrae. Another is a global system of muscles which transfer the load directly to the thoracic cage and pelvic girdle.
The former has included deep muscles such as the multifidus, transversus abdominis, diaphragm, and pelvic floor muscles. The latter has include generally large superficial muscles such as the erector spinae, rectus abdominis, internal and external obliques, quadratus lumborum, gluteus maximus, and latissimus dorsi [4,13,27,28].
Human muscles and fascia have inner and outer units regarding spinal stability [29,30]. Both play an important role as an active system and have mutual interlocking functions. Clinically, weakening of the inner unit often leads to spasm of the back muscle of the outer unit. According to the previous report [31], when the fixation of the inner unit is insufficient, the outer unit is used as a fixed muscle.
In other words, if the active system is impaired, it is expected that the muscles of the outer unit will become excessively strained and affect the joint function, which is a passive system. Especially in the flexibility of the dorsolateral system, muscle tension has been clearly found, reflecting the function of the joint. Flexibility for outer units can be evaluated by combining several tests [30].
The core stability has been in focus concerning the stability of the spine for years. In order to maintain a static posture and move dynamically, a person must stabilize the lumbar spine and pelvic girdle. The core muscle could be responsible for the stabilization.
For the training these muscles, "stabilization exercise program" including theory and practice has been developed. When we observe the rehabilitation approach widespread in recent years, it seems to be learning a functional movement pattern rather than training a specific muscle. This trend suggests the future direction of training [27,32,33]. As for this situation, pole exercise including our six movements seems to show similar efficacy as these programs to some extent [27,32-35].
In current study, we applied pole exercise and investigated the detail of the efficacy. Pole exercises include exercise therapy, physical therapy, manual therapy, gymnastics therapy, and so on. Pole exercise seems to be with low cost practically, and be one of the simple and effective methods to maintain and improve physical function in a short time.
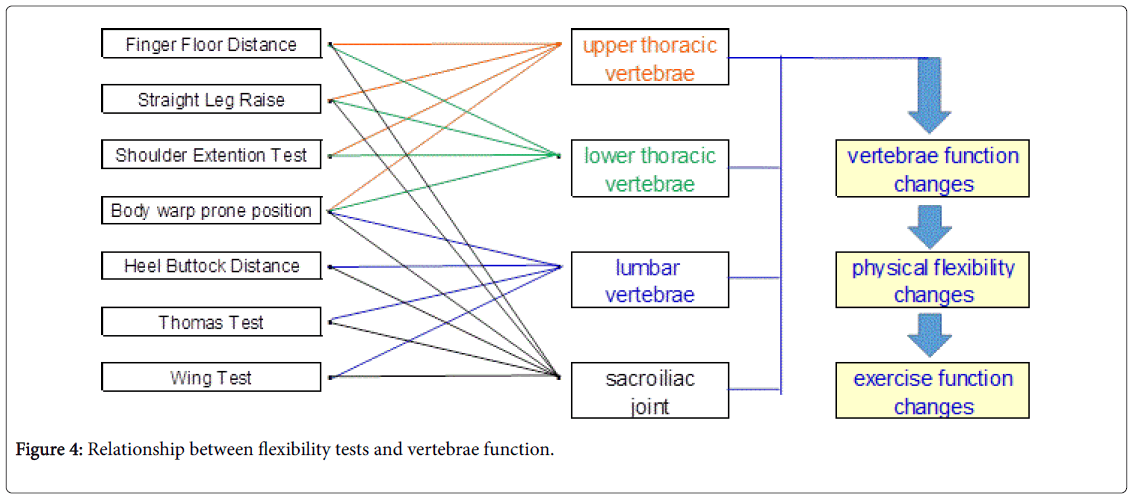
Compared the data before and after the pole exercise, the average value improved in all the exams representing physical flexibility and motor function. These results were compatible for those of previous reports [36,37]. Consequently, current results and characteristics of tests could be summarized to Figure 4. It suggests that the spinal curvature function would be improved, leading to improved flexibility and motor function.
Initially, the motion of the thorax is dominated by the myelinated neural tube branch, which is a mixed nerve including an exercise branch / sensory branch. Sympathetic nerve fibers are mixed in the anterior branch of the spinal nerve. From the above, it is predicted that sympathetic nervous activity will be abnormal due to a decrease in thoracic mobility. Conversely, it seems that there is a possibility that the symptomatic activity abnormality is improved by improvement of thoracic movement range and thoracic mobility.
For spinal flexibility and physical function, three physiological curves in the spinal column are greatly affecting. These are the cervical lordosis, thoracic kyphosis, and lumbar lordosis with a sinusoidal curve. This curvature has the function of absorbing and buffering its reaction when they receive the returning power from another objects.
The drag power of the spinal column increases in proportion to the number of curves, and the drag (R) has the formula of the square of the number of bends (N) +1. In humans, since the number of curves is 3, R=32 + 1=10 [38]. In other words, when the number of curves changes from 1 to 3, the drag becomes 1 to 10. According to these curves, drag force of our spine is 10 times of that of the vertically aligned straight spine. When curves change from 3 to 2 due to impaired spinal column, the drag decreases from 10 to 5.
In the light of evolution, the number of curvatures of the spinal column was 0 in reptiles, 2 in the monkey with no cervical lordosis, and 3 in humans. From these data, improvements in spinal function can be said to be critical for movement and life in humans [38]. Therefore, our pole movement exercises would be effective for the spinal column, enhancing flexibility and physical function, expecting various functions to recover [23].
We have studied about the pole movement including six movements. The examination includes seven flexibility tests and four physical function tests. The result showed improved function of physical flexibility and function, suggesting the usefulness and efficacy of pole movement in short time.
In this study, pole exercise improved flexibility and physical function. Some factors concerning this result would be that the balance of inner and outer unit is improved, the muscle tone of the outer unit is reduced, and the spinal stabilization system is improved. Moreover, outer unit function would influence the facet joint and the vertebral body movement through adhesion to the spinal column.
Among the 11 tests of flexibility and physical function, the most representative one is the Wing test [38,39]. It is an examination that rotates the trunk, and the muscles attached to the spinal column are stretched. In particular, the stretched broad dorsi muscles and gluteus maximus muscles would influence the facet joint and vertebral body movement via attachment to the spinal column. It seems that these are deeply involved in the relationship between the spinal function and the outer unit.
The Wing test is an examination accompanying the rotation of the trunk, and the convoluted elements of the spinal column are deeply involved. In the thoracic vertebra, lumbar vertebra, and sacrum, the rotatable range is the widest in thoracic vertebrae [39]. The thoracic facet joint has adequate structure for maintaining the range of motion. However, there is a thorax present as its characteristic. Movement is restricted to some extent by the costovertebral joint and chest rib joint adjacent to the thoracic facet joint [38]. Therefore, it is thought that the thoracic vertebrae tend to be restricted by the joint constituent in either direction of bending and stretching, side bending, and convolution.
On the other hand, in the lumbar vertebra, the influence of the restriction of the joint constituent on the rotation and the side bending is great. Conversely, there are few restrictions in joint components on flexion and extension movements [38-40].
For the muscles attached to the lumbar vertebrae, the dorsalis muscle and gluteus maximus are indirectly attributed to the lumbar spine function through adhesion to the thoracolumbar fascia [40]. In other words, flexion and extension of the lumbar vertebrae are indirectly susceptible to latissimus dorsi and gluteus majorus, with large muscular restriction.
Conventionally, flexibility tests have been used in clinical practice, in which many of them frequently evaluate the limb muscles. However, there are few ways to evaluate the function of body trunk muscles. There are some tests for evaluate the entire back, but few tests for evaluate specifically. Under such circumstances, wing test would be a useful examination method to evaluate spinal function [39,40]. For evaluation of flexibility in the future, it is recommended to combine multiple tests with wing test as in this report.
As to related studies concerning pole, we could find heart dynamics [41], heart rate and autonomic responses [42,43], flexible and nonflexible poles [44], walking or Trekking poles [44-46], but not find the studies like this report associated with detail evaluation by several tests. One of the limits of this research is small numbers of cases. We would develop our research in which subjects will be the aged or athletes, or patients with orthopedic or metabolic syndrome in the future.
Conclusion
In this study, we proposed the pole exercise including 6 movements which can be easily performed. We investigated 11 tests before and after pole exercise, and there were significant improvement of physical flexibility and exercise function. These results showed the improved function of spinal stability, suggesting that the pole exercise would be effective to relieve problems of vertebrae. Currently obtained data could become fundamental data for clinical application and research development in the future.
Acknowledgement
The content of this article was presented at 9th and 10th Scientific Meeting of Integrative Medicine Japan, Shikoku division, Tokushima, Japan, 2016 and 2017. The authors would like to appreciate the subjects and staff for their co-operation and support.
Conflicts of Interest
The authors declare that they have no conflicts of interest.
References
- Belenkii VY, Gurfinkel VS, Paltsev YI (1967) Elements of control of voluntary movements. Biofizika 12: 135-141.
- Grillner S, Nilsson J, Thorstensson A (1978) Intra-abdominal pressure changes during natural movements in man. Acta Physiol Scand 103:275-287.
- Bouisset S, Zattara M (1981) A sequence of postural movements precedes voluntary movement. Neurosci Lett 22: 263-270.
- Bergmark A (1989) Stability of the lumbar spine. A study in mechanical engineering. ActaOrthopScandSuppl 230: 1-54.
- Panjabi MM (1992) The stabilizing system of the spine. Part I. Function, dysfunction, adaptation, and enhancement. J Spinal Disord 5: 383-389.
- Hoffman J, Gabel P (2013) Expanding Panjabi’s stability model to express movement: A theoretical model. Medical Hypotheses 80: 692-697.
- Maas ET, Juch JN, Groeneweg JG, Ostelo RWJG, Koes BW, et al. (2012) Cost-effectiveness of minimal interventional procedures for chronic mechanical low back pain: design of four randomised controlled trials with an economic evaluation. BMC Musculoskelet Disord 13: 260.
- Melloh M, Elfering A, Presland CE, Röder C, Hendrick P, et al. (2011) Predicting the transition from acute to persistent low back pain. Occup Med 61: 127-131.
- Hendrick P, Milosavljevic S, Bell ML, Hale L, Hurley DA, et al. (2009) Does physical activity change predict functional recovery in low back pain? Protocol for a prospective cohort study. BMC Musculoskelet Disord 10: 136.
- Cholewicki J, McGill S (1996) Mechanical stability of the in vivo lumbar spine: implications for injury and chronic low back pain. Clin Biomech 11: 1-15.
- McGill S, Grenier S, Kavcic N, Cholewicki J (2003) Coordination of muscle activity to assure stability of the lumbar spine. J Electromyogr Kinesiol 13: 353-359.
- Panjabi M (1992) The stabilizing system of the spine. Part II. Neutral zone and instability hypothesis. J Spinal Disord 5: 390-396.
- Barr K, Griggs M, Cadby T (2005) Lumbar stabilization: core concepts and current literature. Part 1. Am J Phys Med Rehabil 84: 473-480.
- Lee LJ, Lee DG (2008) An Integrated Multimodal Approach to the Thoracic Spine and Ribs. In: Magee et al, Pathology and Intervention in Musculoskeletal Intervention, Elsevier, UK.
- Lee DG (2013) The Pelvic girdle – an integration of clinical expertise and research. 4th Edition, Churchill Livingstone publisher, London, UK.
- Grisaffi D (2007) Ed.by Howard LA. Posture and Core conditioning. Grisaffi D & Fitness Development, USA.
- Lee LJ (2012) The essential role of the thorax in whole body function and the “Thoracic Ring Approachâ€. Linda-Joy Lee Physiotherapist Corp (www.ljlee.ca).
- Madhavan S, Shields RK (2007) Weight-bearing exercise accuracy influences muscle activation strategies of the knee. J Neurol Phys Ther 31: 12-19.
- Wakimoto K, Dakeshita T, Tatejima T (2011) Comparison of curved angles in spinal alignment between patients with chronic pain disease and physically unimpaired persons. International Society of Biomechanics. Brussels, Belgium.
- Bruno P (2014) The use of “stabilization exercises†to affect neuromuscular control in the lumbopelvic region: a narrative review. J Can Chiropr Assoc 58: 119-130.
- Bando H, Nakamura T, Yonei Y, Takenaka Y, Seki K (2015) Lipid profile of masters athletes in ice-skating, a model of anti-aging research. Glycative stress research 2: 52-57.
- Bando H, Kan M, Konoike K, Bando M (2017) Squat exercise therapy-effective for diabetics by HiSquat. J Nov Physiother 7: 353.
- Moriyasu A (2016) The influence of spine function for body – Focus on spine dynamics and approach method. J Integr Med Jap Shikoku 18-21.
- Moriyasu A (2017) Clinical application of pole exercise and changes of biomarkers. Spine Dynamics Symposium, Tokyo.
- Yanai H (2015) Four step excel statistics, 4th Edition, Seiun-sha Publishing Co.Ltd, Tokyo.
- Panjabi MM (2003) Clinical spinal instability and low back pain. J ElectromyogrKinesiol 13: 371-379.
- McGill S (2006) Ultimate Back Fitness and Performance. 2nd Ed. Waterloo, BackfitproInc, USA.
- Wilson J, Ferris E, Heckler A, Maitland L, Taylor C (2005) A structured review of the role of gluteus maximus in rehabilitation. N Z J Physiother 33: 95-100.
- Izzo R, Guarnieri G, Guglielmi G, Muto M (2013) Biomechanics of the spine. Part I: spinal stability. Eur J Radiol 82: 118-126.
- Magee DJ (2014) Orthopedic Physical Assessment – Ed 6. Elsevier Saunders, St.Louis, Missouri.
- Hodges PW, Richardson CA (1997) Contraction of the abdominal muscles associated with movement of the lower limb. Phys Ther 77: 132-144.
- McGill S (2002) Low Back Disorders: Evidence-Based Prevention and Rehabilitation. Champaign: Human Kinetics.
- Liebenson C, editor. (2007) Rehabilitation of the Spine: A Pracitioner’s Manual. 2nd Ed. Lippincott Williams & Wilkins, Baltimore.
- Ikeda D, McGill S (2012) Can altering motions, postures, and loads provide immediate low back pain relief: a study of 4 cases investigating spine load, posture, and stability. Spine 37: E1469-75.
- AbouHassan J, Milosavljevic S, Carman A (2010) Can postural modification reduce kinetic and kinematic loading during the bowing postures of Islamic prayer? Ergonomics 53:1446-1454.
- Boudreau S, Farina D, Falla D (2010) The role of motor learning and neuroplasticity in designing rehabilitation approaches for musculoskeletal pain disorders. Man Ther 15: 410-414.
- Barr K, Griggs M, Cadby T (2007) Lumbar stabilization: a review of core concepts and current literature. Part 2. Am J Phys Med Rehabil 86: 72-80.
- Kapandji IA (2008) The Physiology of the Joints: The Spinal Column, Pelvic Girdle and Head volume 3: Annotated Diagrams of the Mechanics of the Human Joints. 6th Revised edition, Churchill Livingstone, USA.
- White AA, Panjabi MM (1990) Clinical Biomechanics of the Spine, 2nd ed. JB Lippincott, Philiadelphia.
- Neumann DA (2017) Kinesiology of the Musculoskeletal System, 3rd Ed, Mosby.
- de Oliveira LS, Moreira PS, Antonio AM, Cardoso MA, de Abreu LC, et al. (2015) Acute effects of flexible pole exercise on heart rate dynamics. Rev Port Cardiol 34:35-42.
- Ogata CM, Navega MT, Abreu LC, Ferreira C, Cardoso MA, et al. (2014) A single bout of exercise with a flexible pole induces significant cardiac autonomic responses in healthy men. Clinics (Sao Paulo) 69: 595-600.
- Dos Santos António AM, Navega MT, Cardoso MA, Abreu LC, Valenti VE (2014) Cardiac autonomic responses induced by a single bout of exercise with flexible pole. Int Arch Med 7: 40.
- Gonçalves M, Marques NR, Hallal CZ, van Dieën JH (2011) Electromyographic activity of trunk muscles during exercises with flexible and non-flexible poles. J Back Musculoskelet Rehabil 24: 209-214.
- Collins EG, Oʼconnell S, McBurney C, Jelinek C, Butler J, et al. (2012) Comparison of walking with poles and traditional walking for peripheral arterial disease rehabilitation. J Cardiopulm Rehabil Prev. 32: 210-218.
- Howatson G, Hough P, Pattison J, Hill JA, Blagrove R, et al. (2011) Trekking poles reduce exercise-induced muscle injury during mountain walking. Med Sci Sports Exerc 43: 140-145.
Citation: Moriyasu A, Bando H, Murakami M, Inoue T, Taichi A, et al. (2018) Pole Exercise Causes Body Changes in Physical Flexibility and Exercise Function. J Nov Physiother 8: 377. DOI: 10.4172/2165-7025.1000377
Copyright: © 2018 Moriyasu A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 9167
- [From(publication date): 0-2018 - Oct 14, 2025]
- Breakdown by view type
- HTML page views: 8120
- PDF downloads: 1047