Review Article Open Access
Prevention and Treatment of IAN Injuries: A Literature Review
Juan F Martínez-Lage Azorín1*, Gustavo Segura Andrés1, Rosa P Valenzuela Molina1, Carlos Almendro Muries1 and Rubén Agustín Panadero2
1Master in Periodontology, Dental Practice, Murcia, Spain
2Department of Stomatology, University Medical and Dental School, Valencia, Spain
- *Corresponding Author:
- Juan F Martínez-Lage Azorín
Master in Periodontology, Dental Practice
C/Alfonso X El Sabio, 14, 1°B, 30008. Murcia, Spain
Tel: 645988187
E-mail: Yonchu1978@gmail.com
Received date: March 24, 2014; Accepted date: May 30, 2014; Published date: June 06, 2014
Citation: Azorín JFML, Andrés GS, Molina RPV, Muries CA, Panadero RA (2014) Prevention and Treatment of IAN Injuries: A Literature Review. J Interdiscipl Med Dent Sci 2:123. doi:10.4172/2376-032X.1000123
Copyright: © 2014 Martínez-Lage Azorín JF, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
The inferior alveolar nerve (IAN) is one of the most important structures in dentistry. It is a terminal branch that originates from the mandibular root of the trigeminal nerve. This branch courses through the inner aspect of the mandible and innervates teeth and some muscles as the mylohyoid or digastric ones and the gums or lips by its mental branch.
Although the main cause of IAN lesion occurs during third molars extractions, IAN can be injured during implant surgery, especially in cases with an atrophic posterior mandible. It is difficult to sever the nerve due to its large caliber. On the contrary, nerve compression or laceration constitute more common complications.
Diverse preventive methods to avoid IAN injury have been reported such as using a precise diagnostic procedure as computerized tomography (CT), guided implant surgery, or placing short implants.
We may classify nerve injury effects ranging from a light tingling (dysesthesia) to temporary or permanent loss of sensibility (hypoesthesia) or to increased sensibility. These cases require a careful management as these events may increase the patients’ and dental practitioners’ anxiety. When the IAN has not been totally interrupted, healing occurs in the next 3 to 6 month even spontaneously.
Sometimes we can alleviate patients giving them some painkillers or vitamin complexes to minimize symptoms or to improve healing. The use and utility of this kind of treatment is controversial however we should not underestimate its placebo effects.
Keywords
Inferior alveolar nerve; IAN; Injury; Needle lesion; Neurotoxicity; Paresthesia; Dysesthesia; Hypoesthesia; Computed tomographic assessment; Panoramic radiography; Third molar surgery; Coronectomy
Introduction
The Problem
The general dentist must daily face diverse and complex problems related to handling of a richly innervated territory, as is the oral cavity. The trigeminal nerve is the main source of innervation of these structures. The inferior alveolar nerve (IAN) originates from the mandibular branch and innervates teeth, muscles and other soft tissues. Normally, the first step for performing any operation that may cause sensitivity or pain to the patient requires anesthetic blocking of this nerve branch. For this reason, the contact with this anatomical structure constitutes part of our daily professional practice.
Clinical conditions that may potentially injure this nerve carry a negative impact that occasionally is of difficult solution, and that may cause more or less severe problems that might affect our patients��? quality of life. The complications associated with this nerve��?s lesion may vary, and include from pain with functional loss to psychological and social impairment, and may also provoke other less documented effects as increased bruxism associated with loss of sensation [1]. Invasive surgical procedures or the vicinity of the nerve trajectory may provoke neuropathic involvement of diverse nature and degree.
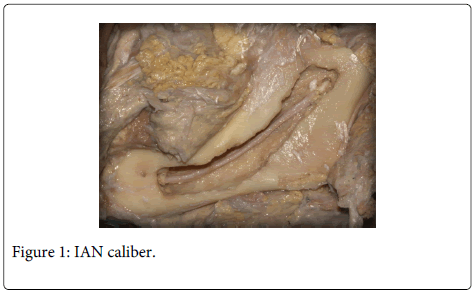
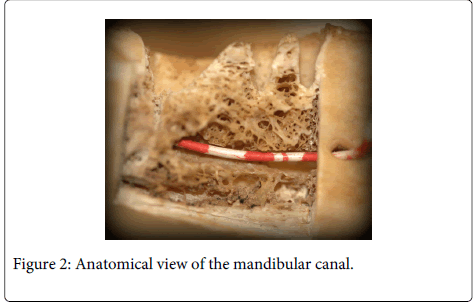
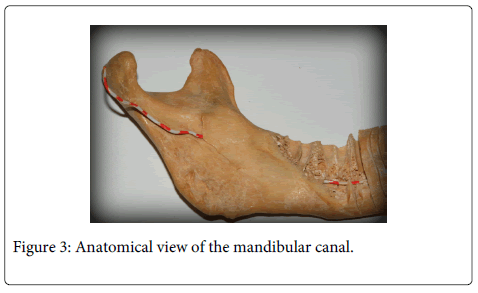
During the iatrogenic accident, anatomic section of the nerve is most improbable due to its large size (Figure 1-3). Usually, diverse degrees of paresthesiae or burning dysesthesia, allodynia and hyperalgesia may appear. Pain occurs in 70% of cases. Surgical invasion of the nerve may trigger the appearance of chronic pain that is accompanied by functional problems. In the worst situation, medico-legal consequences derived from the variable degree of nerve damage may be severe enough to condition the clinical actuation of the clinicians who eventually may avoid performing surgeries that may produce the nerve lesion. This undoubtedly increases work-related stress and limits professional capabilities.
By the present work, we aim to suggest simple guidelines that allow the general dentist to perform an appropriate evaluation of the cases apt to involve the injury of the IAN thus improving the safety of his/her treatments and, in this way, diminish the incidence of lesions to this structure.
There have been descriptions of the diverse causes of injuries to the IAN but we may reduce their classification into four:
Lesions due to the nerve block or to the utilized anesthetic technique
Damage after surgery of dental implants
Injuries due to endodontic treatments
Lesions due to third molar removal surgery
Renton and Yilmaz [2], in a study of 90 patients with IAN lesions found that the main causes of nerve injury were: removal of third molars (60%) followed by local anesthesia use (19%), implant surgery (18%) and endodontic problems (8%).
Material and Methods
We have performed an electronic database search in Medline, PubMed and Cochrane Library and a review of pertinent articles on the subject in the period ranging from 2008 to 2013. The search strategy included the following mentioned keywords. Bibliography inclusion evaluation and validity of articles��? information have been performed independently by five authors with the following selection criteria: pilot studies, systematic reviews, case series, retrospective studies and meta-analysis. Opinion articles as well as those articles with scientific evidence absence and commercial interests were dismissed.
At the end of the searching process, we have included 397 articles, from which 352 were dismissed as they did not meet the selection criteria. We finally selected 45 articles from which we have written up the next review.
Lesions Associated with Nerve block or With the Anesthetic Technique
IAN occurring during the anesthetic block is one of the commonest causes of iatrogenic nerve injury. Although diverse anesthetic techniques do exist, we cannot directly observe the nerve path, and accordingly we commonly resort to anatomical references that usually produce a high failure rate. We can even induce a direct lesion to the nerve bundle by placing the needle within the canal.
A study by Goldberg et al. [3] compared the capability for nervous blocking using a conventional anesthetic technique against the techniques of Gow-Gates and Vazirani-Akinosi and showed slightly worse results with the latter when the degree of block was measured with an electrical test although without existing significant statistical differences. Even though, several technical approaches exist, we might conclude that the ideal anesthetic technique for IAN block is the one with which the clinician feels safer.
During treatment of patients with pulpitis, repeated injections of anesthesia in the IAN may be insufficient for achieving an adequate nerve block and, with it, the ��?precious operating silence��?. Accordingly, in these cases the intraligamentous administration of anesthesia, the reinforcement at the buccal level, or intraosseous anesthesia may constitute the most convenient techniques for avoiding the patient��?s pain [4].
Obviously, local anesthetics used in Dentistry can be regarded as very safe and have a low probability of adverse reactions during their administration [5]. In addition, it seems obvious that the kind of utilized anesthetic may influence the success of the anesthetic technique. A meta-analysis performed by Brandt et al. [6] concluded that articaine was more efficacious than lidocaine for nerve blockage, although when dealing with teeth affected by pulpitis no statistical differences between both substances were found.
Rather unusually, permanent injury of the IAN as a consequence of anesthetic block has been reported. According to the study of Progrel et al. IAN injuries due to anesthetic block can occur with any anesthetic although with variable incidence. In their 6-year study, they found that lidocaine was involved in 25%, articaine in 33% and prilocaine in 34% of cases with paresthesiae. Differences, if any, do not seem to be statistically relevant what would explain that paresthesiae night occur with any type of anesthetic [7]. However, the study of Hillerup et al. [8] concludes that articaine provokes a higher neurotoxicity than the rest of anesthetics. In turn, Renton et al. [9] concluded in that there exists a higher proportion of lingual nerve neuropathies after injection but pain was more intense in IAN. On the other hand, rupture of the injecting needle during nerve block must not be regarded as the cause of its injury. Should it happen, needle removal could require more complex surgery to access the fragment, which could increase the risk for injury. This type of accident is more prone to occur in anxious patients and in children after doing brisk or unexpected movements causing the aforementioned complication [10]. For preventing these events, restless patients and children should be premedicated to diminish anxiety and to decrease unnecessary accidents. Nitrous oxyde may constitute a useful method to control these cases, and would also help to obtaining a more effective nerve block even in cases of irreversible pulpitis [11].
Last, we may face anatomical anomalies of the mandibular canal that might have clinical effects as increase of the risk for nerve injury or of an inadequate anesthetic technique. In this connection, there are descriptions of bifid or even trifid canals. Ueda et al. [12] classified IAN canal into three groups according to its morphology: round/oval, teardrop, and dumbbell shapes, being this feature not as significant as the absence of cortication, as the absence of this is intimately related with the dental damage.
Lesions related to Endodontic Treatments
An even more remote possibility of nerve injury may be due to the displacement of small instruments, such as endodontic files towards the inside of the canal. We know that the fracture of files, usually rotating ones, it is a drawback relatively common during the instrumentation of roots, especially when these are very narrow or have abrupt curves.
Gandhi et al. [13] present a case in which a broken file moved to inside the canal. In this case, the authors could remove the fragment without producing a neuropathic lesion. More routinely, there are reported cases of nerve injury by extrusion of endodontic filling materials (cements, thermo-plasticized or melted gutta-percha ...) towards the periapex producing nerve irritation with neuropathic pain or paresthesias that persist over time with minor improvements [14].
The proximity of the roots of the posterior mandibular teeth (2nd premolars and 1st and 2nd molars), should remind us of the possibility of nerve damage as a result of a little careful manipulation of endodontic filling materials. If there is a very close relationship, we should question the need to avoid techniques of hot condensation, which are potentially more extrusive and require greater control, as well as to assess the proper caliber of the apex. In these cases, the MTA sealed apex (in roots with very wide apices) or the realization of cold condensation can avoid uncomfortable complications [15].
Lesions Due to Dental Implant Surgery
Nerve damage as a result of the placement of dental implants in the posterior mandibular region tends to be the result of poor or bad planning of cases. This is usually due to an inadequate radiological diagnosis. Actually we have a lot of possibilities, so this problem should be reduced at its minimum. Nerve injury could also be caused by overconfidence (recklessness) of the clinician. If planning is correct, nerve damage is highly unlikely, and if it happens it is usually due to inflammation or bone remodeling occurring as a consequence of the surgical technique. In these cases, the damage usually is irrelevant and normal sensitivity recovers after an undetermined period but that does not usually exceed a few months [16].
On the other hand, the use of short implants is also increasingly more widespread and today it constitutes a safe technique for the resolution of cases with widely reabsorbed maxillary ridges. Karthikeyan et al. [17] Performed a systematic review of publications from 1991 to 2011, considering short implants those of 7 mm or less in length, unlike most classical studies that include those with a length below 10 mm. The study concluded that in cases of severe mandibular atrophy, the use of short implants constitute a valid alternative. In general, when we reduce the length of implants, compensation would occur by an increase in diameter.
At present, totally mandibular edentulous patients are often planned with a reduced number of implants, sufficient to support a prosthesis. Overdentures are often a convenient and effective solution [18] and require a minimum number (from two to six) of implants. We usually place the implants in the interforaminal area away from the nerve trajectory. Techniques as all on four of Mal�?² allow the use of hybrid prostheses with only four implants, placed ahead of the mental foramen (Figure 4).
Lesions Related to Third Molar Removal Surgery
IAN injury is the worst of the complications that may occur during surgery for removal of mandibular third molars. Moreover, it is the lesion with the greatest medico-legal consequences. During this surgery, the lesion of lingual and buccal nerves may occur.
Very importantly, experience of the clinician can be of great relevance to minimize the problems consequent to this nerve injury. However, we should argue in this case which is the minimum necessary to consider a clinician as a specialist in this type of treatments and which would be a proper learning curve.
After considering his experience of 1000 patients, Smith concluded that both osteotomy and odontosection, and split division lingual technique increase the risk of excessive bleeding that appears to be associated with an increased risk of temporary neurosensorial deficits [19]. Jerjes et al. [20] conducted a study upon removal of 3236 third molars. They concluded that risk factors that could be considered for IAN paresthesia are: the horizontal position of the third molar, as well as the proximity to the alveolar canal, or the lack of experience of the surgeon. Besides, they found more cases in patients aged between 26 and 30 years. Park et al. [21] concluded that an important risk factor to produce lingual and inferior alveolar nerve paresthesiae is the loss of integrity of the cortical bone of the IAN canal.
On the other hand, Kim et al. [22] established that patients of older age, as well as the depth of molar inclusion can be considered high risk factors. Darkening, deflection, roots��? narrowing, the presence of bifid apices, and narrowing of the canal are also considered significant risk factors.
Prevention Methods
Coronectomy, preventive removal, pericoronal ostectomy and orthodontic traction
Coronectomy of the lower third molars has been described as an alternative to the complete removal of these teeth. We may consider this option when they are in close relationship with the nerve and therefore there is an obvious risk of injury. Long et al. [23] carried out a systematic review of this alternative technique. They concluded that coronectomy allows, in a high percentage, the migration of the remaining roots away from the path of the nerve, so reducing its possible damage in comparison with the complete extraction of these pieces that present a high risk of nerve injury.
Therefore, we can conclude that coronectomy may be a safe alternative treatment in these instances. In the majority of cases it is not accurate to perform a second surgery, and in the few cases in which there are associated symptoms, the more than likely migration of the roots, away from the canal path, will likely minimize nerve damage. There are numerous authors that support the coronectomy as an alternative method for preventing the nerve injury [24-27].
Tolstunov et al. [28] proposed an alternative to coronectomy, called pericoronal ostectomy that achieves satisfactory results with only temporary neurodeficiency. This technique is performed by means of an osteotomy at the level of the clinical crown; then, we wait for a third molar eruption into a more occlusal position, away from the danger zone. Obviously, the limitations of this technique are determined by the position of the molar that must be in a vertical or mesioangular situation.
Wang et al. [29] and Bonetti et al. [30] propose the use of orthodontic traction for a period of 3 to 10 weeks, placing microimplants or orthodontic brackets in antagonistic maxillary molars for third molars disimpaction. Once the third molar roots are away from the canal, then they extract them, thus preventing the nerve injury [29,30].
Last, other authors as Zhang [31] support the preventive removal of third molars when they are still immature to avoid late possible complications. With this purpose, they divided the patients that were submitted to cordal extraction in groups according to age. In the group with immature cordals (mean age of 17 years), there were no nerve lesions and there were only temporary manifestations in 2.48%. In the group that included patients with a mean age of 39 years, the complication rate increased to 10%, which were transient, except for two cases that presented loss of sensation lasting more than 6 months.
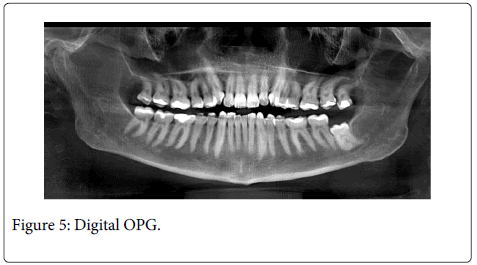
Right radiographic diagnosis
Conventional panoramic radiographs (OPG) have a low predictive value for determining the likely appearance of dental nerve paresthesiae. Classically, signs as interruption of the canal superior cortical line, nerve tract deviation or narrowing, or the presence of a root dark band, are taken into consideration. These signs may warn about a close relationship between third molar roots and the nerve anatomic trajectory. However, some studies show that despite their utility, these signs cannot prevent the appearance of paresthesiae during undertaking the operative maneuvers necessary for their removal. Furthermore, Szalma et al. [32], when comparing conventional OPG with digital OPG (Figure 5), did not describe any significant difference regarding the predictive value of these studies. On the other hand, Guerrero et al. found no significant differences between computerized tomography (CT) and OPG as predictive method for IAN lesions. P�?©cs et al. prefer establishing the diagnosis by appropriate knowledge of the signs on an OPG than using more sophisticated or costly methods that not proved to be more valuable in preventing nerve damage [33]. When there exists a band of darkening in the root when two or more compromising signs are present in OPG, the risk for nerve injury increases significantly [34].
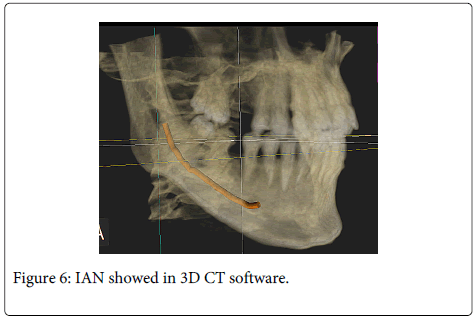
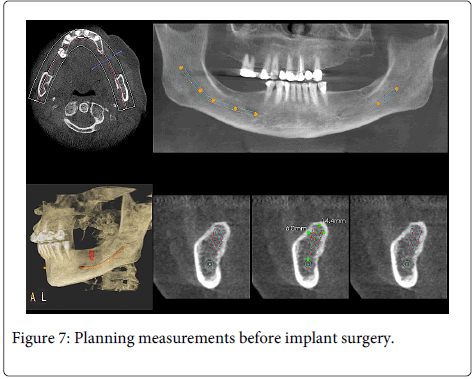
Using diverse types of CT can be a more useful method for planning surgeries related with IAN. Neves et al. [35] found a statistically significant association between nerve exposure and the relationship of third molars with the canal. However, they did not evidence of that a high risk relation between the roots and the nerve for bleeding and/or sensorial involvement. However, Suomlainen et al. [36] studied IAN lesions after third molar surgeries by a generalized CT use in detriment of conventional OPG for planning the cases and contrary to what they previously thought regarding the incidence of nerve lesions. This might correspond to a substitution of the diagnostic method but without optimizing its use. Using CT scans does not significantly decreases the risk for producing an injury to the IAN [37]. Nevertheless, CT use permits the clinician to identify possible individual anatomical variants and to successfully plan cases for implants avoiding damaging important anatomical structures among them, the nerves (Figure 6 and 7).
Umar et al. [38] after the intervention of 185 patients and a total of 200 lower molars, concluded that a careful planning, using traditional radiology (OPG),and supplemented with more sophisticated methods such as CT, shown as a useful strategy to prevent possible damage to the nerve, when the third molar was in a very committed position (high risk cases). With these premises, they not obtained any permanent nerve injury despite the complicated anatomical position of the removed pieces [39].
At present, there are numerous software programs for studying the images obtained with CT that permit marking the IAN course, facilitating real scale measurements that help the clinician to know, before the surgery, the available safety space for a correct placement of the implants in a 3-D disposition. By this method, we can also know the additional needs that might arise during the surgery, for example the need for regenerating the bone. This type of software has a wide catalogue of implants that allows clinicians to simulate the surgery previously, using similar implants and testing which are more appropriate in length and diameter.
Currently, there are programs that are used to elaborate individualized splints, enabling placement of implants assisted by computer (guided surgery). In this way we would take advantage of the reliability of diagnostic image techniques to place implants in the most desired and advantageous position.
Other Causes: Mandibular Fractures
Another of the alveolar nerve injury-related causes is mandibular fracture. In a study conducted by Bede et al. [40], they found that linear displacement and comminuted fractures were which caused more nerve lesions and with a longer period of recovery. However recovery of nerve function in 91% of cases was obtained.
Nerve Lesion
When nerve is damaged, the disorders usually begin immediately after the surgery. Occasionally, but less frequently may appear paresthesia several days later. Borgonovo et al. [41] describe three possible causes of delayed paresthesia: compression of the clot on the nerve trunk, fibrous reorganization of the clot and nerve damage as a result of fragments of bone during the organization of the clot.
Patients affected by nerve damage, reported significant changes in their normal life. Problems while eating, speaking, and in their daily relations and the consequential psychological effects, resulting in depression, loss of employment...In general, most of them improved after different types of management with the passage of time [42].
Treatment of Nerve Lesion
When a neurosensorial deficit appears after the removal of third molars, we should assess how the injury has occurred and what nerve has been damaged. Bagheri and Zuniga agree that lingual nerve is damaged less frequently (38.8% of paresthesias) although its lesion courses with a higher severity and a worse recovery. On the other hand, IAN is damaged more frequently (61.1% of paresthesias) but its consequences are usually less severe and have a faster and better recovery [43].
After identifying the damage that has occurred, the clinician may take different positions, all of which must include a proper advice to the patient, who usually presents great concern and anxiety about the uncertain evolution of the problem. There are non-invasive methods aimed to compensate and assist in the recovery of the deficits caused by dental treatment. Such methods, range from adopting an expectant attitude by assessing the evolution of the injury, to the prescription of drugs. In this case, treatment is based on daily oral administration of homeopathy or complexes of vitamin B12 (Nervobion...) up to recovery of the injury. There is much debate regarding the effect caused by these drugs, because there is no scientific evidence of their effectiveness, and some authors attributed the recovery of the injury due to its placebo effect.
When we found a neurosensorial deficit caused by damage to the lingual nerve, and this injury was not recoverable by non- invasive methods, we have the possibility of repairing this lesion with microsurgery. In this case the surgical treatment is more predictable and effective than in the case of injury of the IAN. Successful results have been obtained in more than 80% of cases, if surgery is carried out by an expert neurosurgeon [44].
Microsurgery is a technique that requires training and that tends to be quite effective, although the chances of success decrease when the age of the patient (elderly) increases and when a greater time has elapsed since the lesion (over 12 months) [45].
Conclusions
The most frequent causes of damage of the IAN are the removal of third molars, the placement of implants next to the alveolar canal, the injection of local anesthetics or the extrusion of endodontic materials to the periapex. In addition, there are other less frequent causes such as jaw fractures. The main prevention method will always be to establish a correct diagnosis and to make a correct radiographic planning, with CT or conventional panoramic radiography, before dental treatment. Besides, we should evaluate the possibility of using less invasive methods in the removal surgery of third molars, as are coronectomy or orthodontic extrusion. At the same time, we should perform root shutter techniques, controlled and according to the caliber of the root canals to be treated. In this way, we should avoid using fluid materials for the most complex endodontic cases to prevent their loss to the periapex. Finally, professional experience and proper planning reduces the risk of suffering neurosensorial deficits. Anyway, if they appear, we could treat them from adopting an expectant conduct, accompanied by a correct advice to the patients and registering its evolution, up to the administration of drugs or treatment of lesions with microsurgery.
References
- Melis M, Coiana C, Secci S (2012) Bruxism elicited by inferior alveolar nerve injury: a case report. Int J Periodontics Restorative Dent 32: e29-33.
- Renton T, Yilmaz Z (2011) Profiling of patients presenting with posttraumatic neuropathy of the trigeminal nerve. J Orofac Pain 25: 333-344.
- Goldberg S, Reader A, Drum M, Nusstein J, Beck M (2008) Comparison of the anesthetic efficacy of the conventional inferior alveolar, Gow-Gates, and Vazirani-Akinosi techniques. J Endod 34: 1306-1311.
- Kanaa MD, Whitworth JM, Meechan JG (2012) A prospective randomized trial of different supplementary local anesthetic techniques after failure of inferior alveolar nerve block in patients with irreversible pulpitis in mandibular teeth. J Endod 38: 421-425.
- Bendgude V, Akkareddy B, Jawale BA, Chaudhary S (2011) An unusual pattern of self-inflicted injury after dental local anesthesia: a report of 2 cases. J Contemp Dent Pract 12: 404-407.
- Brandt RG, Anderson PF, McDonald NJ, Sohn W, Peters MC (2011) The pulpal anesthetic efficacy of articaine versus lidocaine in dentistry: a meta-analysis. J Am Dent Assoc 142: 493-504.
- Pogrel MA (2012) Permanent nerve damage from inferior alveolar nerve blocks: a current update. J Calif Dent Assoc 40: 795-797.
- Hillerup S, Jensen RH, Ersb�?¸ll BK (2011) Trigeminal nerve injury associated with injection of local anesthetics: needle lesion or neurotoxicity? J Am Dent Assoc 142: 531-539.
- Renton T1, Adey-Viscuso D, Meechan JG, Yilmaz Z (2010) Trigeminal nerve injuries in relation to the local anaesthesia in mandibular injections. Br Dent J 209: E15.
- Bacci C, Mariuzzi ML, Ghirotto C, Fusetti S (2012) Local anesthesia needle breakage in a 5-year-old child during inferior alveolar nerve block with the Vazirani-Akinosi technique. Minerva Stomatol 61: 337-40.
- Stanley W, Drum M, Nusstein J, Reader A, Beck M (2012) Effect of nitrous oxide on the efficacy of the inferior alveolar nerve block in patients with symptomatic irreversible pulpitis. J Endod 38: 565-569.
- Ueda-Ueda M, Nakamori K, Shiratori K, Igarashi T, Sasaki T et al. (2012) Clinical significance of computed tomographic assessment and anatomic features of the inferior alveolar canal as risk factors for injury of the inferior alveolar nerve at third molar surgery. J Oral MaxillofacSurg 70: 514-20.
- Gandhi N1, Gandhi S, Bither S (2011) Displacement of endodontic instruments in inferior alveolar canal. Indian J Dent Res 22: 736.
- Gonzalez-Martin-Gonz�?¡lez-Mart�?n M, Torres-Lagares D, Guti�?©rrez-P�?©rez JL, Segura-Egea JJ (2010) Inferior alveolar nerve paresthesia after overfilling of endodontic sealer into the mandibular canal. J Endod 36: 1419-21.
- L�?³pez-L�?³pez J, Estrugo-Devesa A, Jan�?©-Salas E, Segura-Egea JJ (2012) Inferior alveolar nerve injury resulting from overextension of an endodontic sealer: non-surgical management using the GABA analogue pregabalin. IntEndod J 45: 98-104.
- Renton T, Dawood A, Shah A, Searson L, Yilmaz Z (2012) Post-implant neuropathy of the trigeminal nerve. A case series. Br Dent J 212: E17.
- Karthikeyan I1, Desai SR, Singh R (2012) Short implants: A systematic review. J Indian SocPeriodontol 16: 302-312.
- Mart�?nez-Lage-Azor�?n JF1, Segura-Andr�?©s G2, Faus-L�?³pez J3, Agust�?n-Panadero R4 (2013) Rehabilitation with implant-supported overdentures in total edentulous patients: A review. J ClinExp Dent 5: e267-267e272.
- Smith WP (2013) The relative risk of neurosensory deficit following removal of mandibular third molar teeth: the influence of radiography and surgical technique. Oral Surg Oral Med Oral Pathol Oral Radiol 115: 18-24.
- Jerjes W, Upile T, Shah P, Nhembe F, Gudka D, et al. (2010) Risk factors associated with injury to the inferior alveolar and lingual nerves following third molar surgery-revisited. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 109: 335-45.
- Park W, Choi JW, Kim JY, Kim BC, Kim HJ, et al. (2010) Cortical integrity of the inferior alveolar canal as a predictor of paresthesia after third-molar extraction. J Am Dent Assoc 141: 271-278.
- Kim JW, Cha IH, Kim SJ, Kim MR (2012) Which risk factors are associated with neurosensory deficits of inferior alveolar nerve after mandibular third molar extraction? J Oral MaxillofacSurg 70: 2508-2514.
- Long H, Zhou Y, Liao L, Pyakurel U, Wang Y, et al. (2012) Coronectomy vs. total removal for third molar extraction: a systematic review. J Dent Res 91: 659-665.
- Ahmed C, Wafae el W, Bouchra T (2011) Coronectomy of third molar: a reduced risk technique for inferior alveolar nerve damage. Dent Update 38: 267-268, 271-2, 275-6.
- Monaco G, de Santis G, Gatto MR, Corinaldesi G, Marchetti C (2012) Coronectomy: a surgical option for impacted third molars in close proximity to the inferior alveolar nerve. J Am Dent Assoc 143: 363-369.
- Leung YY, Cheung LK (2010) Coronectomy as the treatment of choice in wisdom teeth showing radiographic signs of close proximity to inferior dental nerve. Ann R AustralasColl Dent Surg 20: 93-94.
- Cilasun U, Yildirim T, Guzeldemir E, Pektas ZO (2011) Coronectomy in patients with high risk of inferior alveolar nerve injury diagnosed by computed tomography. J Oral MaxillofacSurg 69: 1557-1561.
- Tolstunov L, Javid B, Keyes L, Nattestad A (2011) Pericoronalostectomy: an alternative surgical technique for management of mandibular third molars in close proximity to the inferior alveolar nerve. J Oral MaxillofacSurg 69: 1858-1866.
- Wang Y, He D, Yang C, Wang B, Qian W (2012) An easy way to apply orthodontic extraction for impacted lower third molar compressing to the inferior alveolar nerve. J CraniomaxillofacSurg 40: 234-237.
- Bonetti GA, Parenti SI, Checchi L (2008) Orthodontic extraction of mandibular third molar to avoid nerve injury and promote periodontal healing. J ClinPeriodontol 35: 719-723.
- Zhang QB, Zhang ZQ (2012) Early extraction: a silver bullet to avoid nerve injury in lower third molar removal? Int J Oral MaxillofacSurg 41: 1280-1283.
- Szalma J, Lempel E, Jeges S, Szab�?³ G, Olasz L (2010) The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 109: 294-302.
- Guerrero ME, Nackaerts O, Beinsberger J, Horner K, Schoenaers J et al. (2012) Inferior alveolar nerve sensory disturbance after impacted mandibular third molar evaluation using cone beam computed tomography and panoramic radiography: a pilot study. Oral Surg Oral Med Oral Pathol Oral Radiol 114: 294-302.
- Leung YY, Cheung LK (2011) Correlation of radiographic signs, inferior dental nerve exposure, and deficit in third molar surgery. J Oral MaxillofacSurg 69: 1873-1879.
- Neves FS, de Almeida SM, B�?³scolo FN, Haiter-Neto F, Alves MC et al. (2012) Risk assessment of inferior alveolar neurovascular bundle by multidetector computed tomography in extractions of third molars. SurgRadiolAnat 34: 619-24.
- Suomalainen A, Apajalahti S, Vehmas T, Vent�?¤ I (2013) Availability of CBCT and iatrogenic alveolar nerve injuries. ActaOdontolScand 71: 151-156.
- Sanmart�?-Garcia G, Valmaseda-Castell�?³n E, Gay-Escoda C (2012) Does computed tomography prevent inferior alveolar nerve injuries caused by lower third molar removal? J Oral MaxillofacSurg 70: 5-11.
- Umar G, Obisesan O, Bryant C, Rood JP (2013) Elimination of permanent injuries to the inferior alveolar nerve following surgical intervention of the "high risk" third molar. Br J Oral MaxillofacSurg 51: 353-7.
- Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, et al. (2011) The use of cone beam CT for the removal of wisdom teeth changes the surgical approach compared with panoramic radiography: a pilot study. Int J Oral MaxillofacSurg 40: 834-839.
- Bede SY, Ismael WK, Al-Assaf DA, Omer SS (2012) Inferior alveolar nerve injuries associated with mandibular fractures. J CraniofacSurg 23: 1776-1778.
- Borgonovo A, Bianchi A, Marchetti A, Censi R, Maiorana C (2012) An uncommon clinical feature of IAN injury after third molar removal: a delayed paresthesia case series and literature review. Quintessence Int 43: 353-359.
- Pogrel MA, Jergensen R, Burgon E, Hulme D (2011) Long-term outcome of trigeminal nerve injuries related to dental treatment. J Oral MaxillofacSurg 69: 2284-2288.
- Zuniga JR (2009) Management of third molar-related nerve injuries: observe or treat? Alpha Omegan 102: 79-84.
- Meyer RA, Bagheri SC (2011) Nerve injuries from mandibular third molar removal. Atlas Oral MaxillofacSurgClin North Am 19: 63-78.
- Bagheri SC, Meyer RA, Cho SH, Thoppay J, Khan HA, et al. (2012) Microsurgical repair of the inferior alveolar nerve: success rate and factors that adversely affect outcome. J Oral MaxillofacSurg 70: 1978-1990.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 28700
- [From(publication date):
June-2014 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 23388
- PDF downloads : 5312