Research Article Open Access
Primary Aneurysmal Bone Cyst of Long Bones Treated with a Single Dose of Calcitonin and Methylprednisolone Percutaneous Intralesional Injection: A Case Series and Literature Review
Marcelo Braganca dos Reis Oliveira1,2*, Walter Meohas1, Gustavo Sobral de Carvalho1,2, Ronaldo Rego Rodrigues1, Felipe Cesar Rosa Oliveira1, Ana Cristina de Sa Lopes1, Fernanda Carvalho de Queiroz Mello2 and Marcos Eduardo Machado Paschoal21National Institute of Trauma and Orthopedics, Rio de Janeiro, Brazil
2Federal University of Rio de Janeiro, Rio de Janeiro, Brazil
- Corresponding Author:
- Oliveira MBDR
Trauma and Orthopedics Hospital
University of Clementino Fraga Filho of the Federal University of Rio de Janeiro
Rua Rodolpho Paulo Rocco, 255, University City - Fundao Island
Rio de Janeiro, CEP: 21941-913, RJ, Brazil
Tel: 55 21 3938-2838
Fax: 55 21 3938-2838
E-mail: marceloreis@hucff.ufrj.br
Received Date: July 27, 2016; Accepted Date: August 05, 2016; Published Date: March 28, 2017
Citation: Oliveira MBDR, Meohas W, de Carvalho GS, Rodrigues RR, Oliveira FCR, et al. (2017) Primary Aneurysmal Bone Cyst of Long Bones Treated with a Single Dose of Calcitonin and Methylprednisolone Percutaneous Intralesional Injection: A Case Series and Literature Review. J Orthop Oncol 2:113. doi: 10.4172/2472-016X.1000113
Copyright: © 2017 Oliveira MBDR, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Orthopedic Oncology
Abstract
Aneurysmal bone cyst is a rare benign bone tumor usually treated by surgery, which may in turn result in poor functional outcome and recurrence. This study aims to report a series of cases of primary ABC treated with a single dose of calcitonin and methylprednisolone injection. Six patients treated with a single-dose combination of calcitonin (200 UI) and methylprednisolone (120 mg) at a single institution from January 2011 to December 2013 were clinically and radiologically evaluated. After the follow-up period, all patients presented cyst healing. The mean time to healing was 2.8 months. The final mean overall functional score rating was 89.0%. We conclude that intralesional calcitonin and methylprednisolone injection results in aneurysmal bone cyst healing with good functional outcomes and thus can be an effective treatment method.
Keywords
Aneurysmal bone cyst; Calcitonin; Methylprednisolone
Abbreviations
ABC: Aneurismal Bone Cyst; MMP: Matrix Metalloproteinase
Introduction
Aneurysmal bone cyst (ABC), first described by Jaffe and Lichtenstein in 1942 [1], is an active/aggressive benign bone tumor, which may result in high skeletal morbidity and recurrence if not accurately treated [2,3]. Treatment commonly involves curettage or resection [2-5]. However, other minimally invasive strategies have been previously described, such as radiation therapy, sclerotherapy, embolization, and injection of a variety of enhancer ossification agents [6-13].
The traditional surgical methods result in high recurrence rate, high morbidity, and prolonged recovery period and carry a significant risk of bleeding and damage to surrounding structures essential for the maintenance of function of the affected segment [3,14-16]. Furthermore, for spinal lesions, which can be very vascular, surgical treatment is technically challenging with the risk of significant blood loss, postoperative spinal deformity, and the possibility of recurrence [16-19]. Thus, minimally invasive methods have been initially proposed to treat ABC in sites with difficult surgical access, especially the spine and pelvis, as surgical treatment results in increased morbidity.
In previous reports, intralesional calcitonin and methylprednisolone injection was shown to be a promising alternative to surgical treatment for axial ABC [19-22]. Accordingly, the initial results obtained were satisfactory; thus, we proposed the use of this method in the treatment of long bone lesions to avoid surgical morbidity. Further, considering the positive results for spinal lesions at our institution [22], we promote the use of this treatment method for long bone ABC to avoid surgical treatment. However, only few studies with a significant number of patients exist due to the low incidence of neoplasia and the variety of treatment methods. The purpose of this study is to report our initial experience with this minimally invasive treatment for extraaxial ABC through a series of six cases, which the lesion was healed after a single dose of intralesional calcitonin and methylprednisolone.
Methods
This study presents a small series of cases of ABCs in long bones treated with a single-dose of calcitonin and methylprednisolone percutaneous intralesional injection at our institution from January 2011 to December 2013. After the Institutional Review Board approval, informed consent was obtained from all individual participants included in the study. We retrospectively evaluated the medical records and radiological exams of six patients who met the inclusion criteria. The radiological and functional results were evaluated with a minimum follow-up period of 24 months.
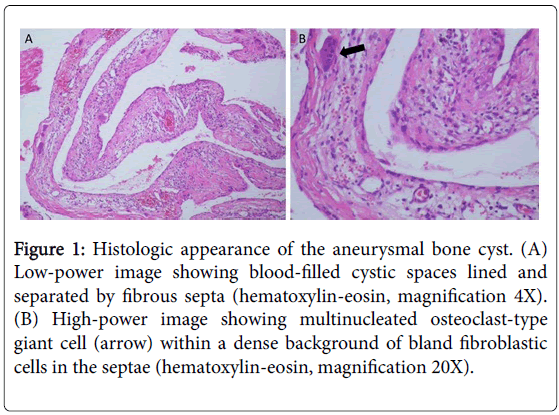
The patients underwent clinical and imaging evaluation, including plain film, CT scan, and magnetic resonance imaging. Histopathologic examination of the specimen obtained from percutaneous biopsy confirmed the diagnosis of primary ABC (Figure 1).
Figure 1: Histologic appearance of the aneurysmal bone cyst. (A) Low-power image showing blood-filled cystic spaces lined and separated by fibrous septa (hematoxylin-eosin, magnification 4X). (B) High-power image showing multinucleated osteoclast-type giant cell (arrow) within a dense background of bland fibroblastic cells in the septae (hematoxylin-eosin, magnification 20X).
The volume of the lesion was measured, and ABCs were classified based on the five morphologic subgroups of Capanna et al. [23]. Type I lesions are centrally located and well contained, with either no outline or a slightly expanded outline. Type II lesions have marked expansion and cortical thinning with involvement of the entire bony segment. Type III lesions are eccentric and metaphyseal and typically involve only one cortex. Type IV lesions are the least common subgroup and develop subperiosteally, expanding away from the bone. Type V lesions occur periosteally and expand peripherally, ultimately penetrating the cortical bone [23]. The Enneking staging system for benign bone tumors was used to classify the lesions as B1 (latent), B2 (active), and B3 (aggressive) [24].
Treatment started 3 months after biopsy to give enough time for spontaneous healing to occur following bone puncture, as reported previously [25]. Intralesional calcitonin and methylprednisolone injection was performed inside the operating room. Patients <15 years were placed under general anesthesia, and 2% xylocaine local anesthetic with sedation was used in older patients. An 11-gauge bone marrow biopsy needle was passed through the expanded outer cortex into the lesion under fluoroscopic guidance. After bloody fluid aspiration, 5 ml of a calcitonin (200 IU) and methylprednisolone (120 mg) mixture was gently injected into the ABC.
The treatment response was evaluated through ossification increase on plain films and pain relief. The end-point of treatment was defined as the time at which the pain had resolved, the cortical thickness of the wall of the cyst had started reforming, and the lesion had stopped growing. Monthly plain radiographs were taken until satisfactory ossification was reached. Subsequent radiographic examinations were performed every 3 months up to 2 years and every 6 months thereafter. At each follow-up visit, the lesions were radiologically graded using a system described by Rastogi et al. as follows: grade I (residual lesion<25% of the initial lesion), grade II (residual lesion 25%-49%), grade III (residual lesion 50%-74%), and grade IV (residual lesion>75%) [8]. Grades III and IV were recorded as unsatisfactory; grades I and II were considered to show a satisfactory radiological outcome. The acceptability of treatment, the occurrence of complications, and a functional assessment were also recorded at each follow-up visit according to the method of Enneking et al. [26].
Results
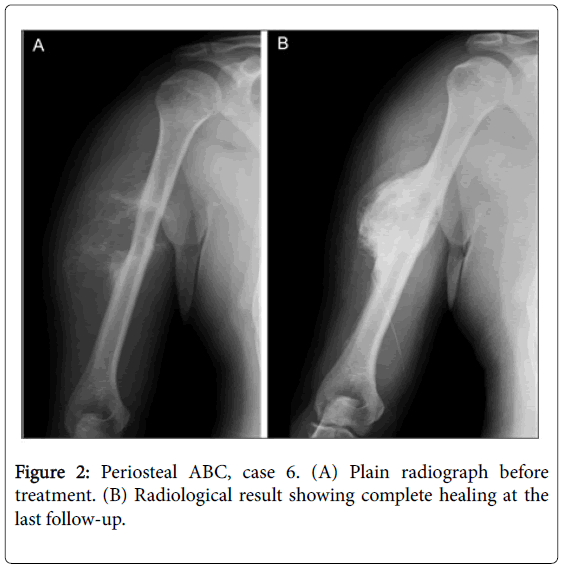
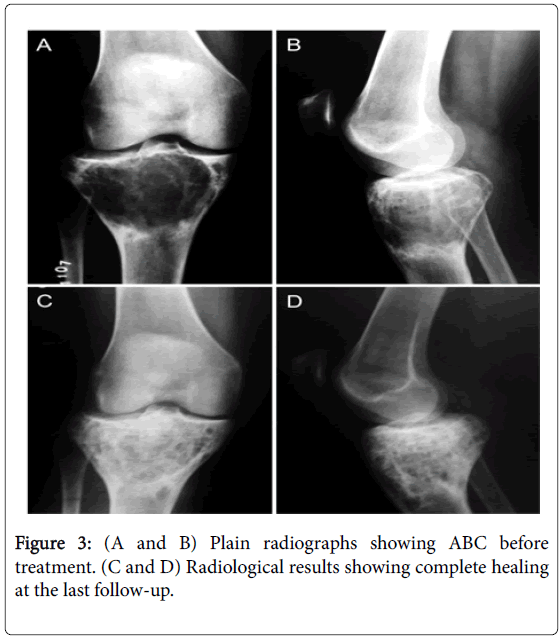
Six patients (3 males, 3 females) with a mean age of 19.7 years (9 to 41) were evaluated. The patient characteristics and treatment course are shown in Table 1. There were 3 lesions in the femur, 1 in the humerus, 1 in the fibula, and 1 in the tibia. The mean follow-up period was 37.7 months (24 to 60). All patients had a satisfactory clinical outcome and returned to full activities. The mean ABC healing time after injection was 2.8 months (2 to 4). The overall mean residual size of the lesion at the final follow-up was 16.3% (8.5% to 30.1%). Good ossification results were found in all 6 patients. Grade I healing was found in 5 patients (83.3%) and grade II in 1 (16.7%). The Figures 2 and 3 show, respectively, case 4 and 6 plain radiographs before and after treatment. Cysts healing can be observed through sclorosis increasing on Figures 1B, 2C and 2D. The functional scores were excellent with a mean overall rating of 79.0% (60% to 86.7%) at the end of treatment and 89.0% (66.7% to 100%) at the final follow-up, as assessed using the system of Enneking et al. Functional score improvement correlated positively with lesion size reduction (Table 2) (Figure 2). Nauseas, hypocalcemia, and hypophosphatemia, the possible side effects of this treatment, were not observed after injection.
| No. | Age | Gender | Location | Enneking | Capanna | Volume | Healing | Healing | Recurrence | |||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| (years) | staging | classification | (cm3) | time (months) | grade | |||||||
| 1 | 11 | F | Femur | B2 | III | 25.2 | 3 | I | No | |||
| 2 | 14 | M | Femur | B3 | III | 28.6 | 2 | I | No | |||
| 3 | 9 | M | Fibula | B2 | III | 10.1 | 4 | II | No | |||
| 4 | 25 | F | Tibia | B2 | II | 30.5 | 3 | I | No | |||
| 5 | 18 | M | Femur | B3 | II | 40.3 | 3 | I | No | |||
| 6 | 41 | M | Humerus | B3 | VI | 60.3 | ||||||
Table 1: Patients characteristics and treatment course
| Parameters | Values (range) |
|---|---|
| Mean age in years | 19.7 (9-41) |
| Gender (M:F) | 3:3 |
| Mean functional score* at the end of treatment | 23.7 (12-30) |
| Mean functional score* at the end of follow-up | 26.7 (20-30) |
| Mean healing time | 2.8 (2-4) |
| Mean volume of lesion in cm3 pretreatment | 32.2 (10.1-60.3) |
| Mean volume of lesion in cm3 at the end of follow-up | 5 (1.1-10.3) |
| Mean residual size of lesion in % | 16.3 (8.5-30.1) |
Table 2: Clinical details and results *Enneking’s method.
Discussion
ABC is a rare, locally destructive benign bone tumor, which has a low incidence rate (0.14-0.32 cases per 100,000 individuals) [27,28]. As defined by the World Health Organization, ABC is an expansile osteolytic lesion that consists of blood-filled spaces and channels separated by connective tissue septa that may contain osteoid tissue and osteoclast-like giant cells [3]. This lesion may occur in any bone at any age [3,28]. However, more than 50% of the ABCs present in the long bones and about 80% of the cases are seen before the age of 20 years [2,28].
ABCs are considered as primary lesions in approximately 70% of cases, with the remaining 30% arising secondary to different primary tumors, including giant cell tumor, unicameral bone cyst, and chondroblastoma [5]. As regards the primary ABC pathogenesis, currently, the presence of a chromosomal translocation t(16;17) (q22;p13), as a recurring abnormality and overexpression of insulinlike growth factor confirms the hypothesis that primary ABC is a true neoplastic lesion [29-31]. Matrix metalloproteinase-9 (MMP) induction in response to the presence of the fusion protein ubiquitin specific protease 6 plays an important role in the pathogenesis and osteoclast destructive activity [32]. These findings can support bone target therapy based on osteoclast and fibroblast inhibitors, such as calcitonin and methylprednisolone, for ABC treatment.
Although ABC is completely benign, this expansile osteolytic lesion may lead to a pathological fracture [14,15,28]. Thus, intralesional procedures, such as curettage with or without the use of burr, bone marrow injection, or bone grafting, are the most common treatment options, and resection is primarily used in expandable bones, such as the fibula, clavicle, or rib [2,3,5]. Recurrence is frequently seen within 24 months following the initial treatment and ranges from 10% to 59% with different surgical removal techniques [3,4,14].
Surgical treatment may result in extensive bone defects and entails a significant risk of bleeding and damage to important adjacent anatomical structures. Besides profuse bleeding, the risk of growth plate lesions in young children and recurrence make the operative treatment challenging [3,15,33]. Therefore, non-surgical methods, including sclerotherapy, selective arterial embolization, and infiltration of enhancer ossification agents, have gained attention in ABC treatment [7-11]. Excellent success rates associated with the use of these modalities were reported with varying complication rates [7,8,34,35]. However, there is paucity of prospective randomized controlled studies directly comparing these methods with conventional surgical treatment. Thus, the choice of technique has generally been guided by the surgeon's experience and preference.
The axial location (pelvic, sacral, and lumbar spine), occurring in about 20% of cases, renders the surgical treatment extremely complex and a risky approach [19-21]. Therefore, minimally invasive procedures as an alternative treatment have been initially described for spine lesions where the risk and morbidity are higher. Selective arterial embolization and sclerotherapy are the most frequently used nonsurgical methods [7,10]. However, calcitonin and methylprednisolone injection is a promising percutaneous method expected to lower the rate of complications [19-21,36].
Percutaneous techniques are increasingly used in ABC treatment to reduce surgical morbidity. Intralesional injection of calcitonin in combination with methylprednisolone is one of the percutaneous treatment methods. It was initially described to treat cervical spine ABC among children, who are at high risk of potentially devastating complications due to inadvertent vertebral artery embolization and surgical treatment resulting in spinal instability—a more undesirable outcome for growing children [20,21,35]. We believe that this treatment offers the least invasive initial therapeutic option, while the more invasive surgical or endovascular strategies are reserved for resistant lesions. Therefore, based on previous reports of a positive treatment outcome, i.e., healing of axial ABC, after calcitonin and methylprednisolone injection, this study aims to promote the use of this method in treating lesions in other locations, such as the long bone.
To the best of our knowledge, five published manuscripts reported on the use of this method, with only 7 cases treated with intralesional injection of a calcitonin and steroid combination [19-22,36]. Although the spine is involved in only 15% of the cases; in the studies, the majority of ABCs are located in the spine [19-22].
Calcitonin injection for ABC was first described by Szendroi. Successful results in 6 of 7 cases treated with intralesional calcitonin injection without methylprednisolone, performed three times per week for a total of 5 weeks, were reported. In this series, three cysts completely and the remaining three partially healed. In one case, the treatment was discontinued because of hypersensitivity, leading to the recurrence of the lesion [11].
In 2000, Gladden et al. postulated that methylprednisolone and calcitonin combination could have a synergistic effect on ABC healing, owing to the angiostatic and fibroblastic inhibitory effects of methylprednisolone combined with osteoclast inhibition and increased bone trabeculae formation mediated by calcitonin [21]. A case of ABC at the first cervical vertebra in 3-year-old children was reported. Treatment included two CT-guided intralesional injections of calcitonin (100 IU) combined with methylprednisolone (80 mg) with an interval of 6 months, resulting in sclerosis, lesion size reduction, and resolution of symptoms without complications. During the last follow-up visit, 2 years and 7 months after the initiation of therapy, CT demonstrated approximately 95% resolution of the lytic component without adverse effects. This result suggests that methylprednisolone and calcitonin have a synergistic effect. Therefore, the use of this combination therapy need not be as frequent as that of calcitonin alone therapy.
Rai and Collins [19] and Ohashi et al. [20] reported that a combination of calcitonin (200 UI) and methylprednisolone (125 mg) results in the following favorable outcomes similar to those of this study: progressive ossification and the absence of complications, such as hypocalcemia and hypophosphatemia. Only two injections were performed over several months in both studies. Despite the lower number of injections than that initially described for calcitonin injection, healing was still achieved.
At our institution, three cases of ABC at the second cervical vertebral that healed after two injections, following the same dose protocol as the present study, were reported [22]. In a more recent published case report regarding this technique by Meohas et al, parosteal ABC at the diaphyseal humerus healed after a single-dose injection of a combined drug [36]. The study is the first to report extraaxial ABC treated by a combination therapy.
To our knowledge, the present study has the largest ABCs series treated with percutaneous injection of calcitonin and steroid combination. Here, extra-axial ABC healing was achieved after a single injection of calcitonin (200 UI) and methylprednisolone (120 mg), while majority of the related studies reported ABC healing after two injections. Calcitonin and methylprednisolone doses were decided empirically. Similar to the previous study, fixed doses were injected regardless of the lesion size [19-22,36]. Subsequent sclerosis and shrinkage of the lesion and resolution of symptoms were observed. In all cases, the follow-up radiographs and CT scans showed that the osteoblastic activity was persistent, with progressive ossification of the cavities in a concentric manner, thickening the walls and reducing the blood volume inside them. At the end of the treatment, most of the ABC were ossified, with shrinkage of the lesions, pain relief, and good functional results.
Although spontaneous ABC regression is described [25], we believe in the positive effect of injection on promoting ABC healing. Spontaneous regression is extremely rare in relatively older patients with ABCs, and only few reports of spontaneous ABC regression in younger patients currently exist [25]. McQueen et al. described some improvement in relatively young patients after a simple biopsy; however, in these cases, radiographs showed an increase in the tumor size several months after the procedure. In contrast, the present cases showed no enlargement or recurrence at least 2 years after treatment.
The proposed mechanism of action of calcitonin is primarily the suppression of osteoclast activity and promotion of new bone formation in the connective tissue septa of the cyst wall. On the other hand, some data suggest that methylprednisolone has angiostatic and fibroblastic inhibitory effects and may exert a synergistic effect when used with calcitonin. Based on previous studies, it may be hypothesized that ABC healing after intralesional infiltration of calcitonin and methylprednisolone is due to the following: (1) inhibition of extracellular lysosomal protease production, (2) apoptotic steroid action in osteoclast-like giant cells, and (3) inhibition of transcription factors in cell proliferation. These three mechanisms cause bone reabsorption reduction, cell proliferation inhibition, reduced vascularization, and pro-inflammatory factor inhibition. Furthermore, the anti-neoplastic activity of corticosteroids and apoptosis induction by various human cells were also described [37]. It is also possible that the drug combination has a direct cytotoxic effect on the mesenchymal component of ABC. Furthermore, as described, the agents have a multifactorial action, which is related to the inhibition of MMP production, angiogenesis, and osteoclast function, as well as to the induction of osteoclast apoptosis and promotion of osteoblast regeneration. These findings are consistent with the description of ABC as a clonal tumor expressing high levels of MMPs and vascular endothelial growth factor, which has a high osteoclast activity and presents a blockage in osteoblast maturation [28-32,38].
Intralesional calcitonin and methylprednisolone injection is a promising method for the treatment of primary ABC. Complete ossification, maintained at least 2 years after the treatment, was observed. The lesions had a significant reduction in the initial lytic area, requiring only one injection per patient. There were no reports of adverse effects (vomiting and/or seizures) or hypersensitivity. However, factors related to the treatment response exist; therefore, one injection, as described previously, is not always sufficient to reach satisfactory results. Younger patients, B3 classification, and high mitotic indices are considered risk factors for ABC recurrence in other treatment modalities and could be potential risk factors for the combination therapy [3,39,40]. Therefore, further studies with a larger sample of patients are necessary to evaluate whether risk factors predict treatment response, a greater number of injections is required, and a more prolonged treatment period is needed to obtain satisfactory results.
Preliminary results show consistently successful results of the largest series of patients with primary ABC treated with a calcitonin and methylprednisolone percutaneous intralesional injection. The outcome of this case series confirms that the injection of calcitonin need not be as frequent as previously reported, especially when used in a combination therapy. It was also suggested that methylprednisolone may exert a synergistic effect when used with calcitonin. The potential advantages of the treatment method are as follows: minor local morbidity, especially in lesions with difficult surgical access; better treatment acceptance by the patient; and less time. We believe that two to three infiltrations at intervals of 2-3 months are sufficient to address the large majority of ABCs without causing damage; surgery is only necessary in cases of residual or recurrent lesions. Low ABC incidence is a major challenge for further studies, which in turn results in the difficulty to fully understand and prove the real effectiveness of the different treatment modalities. The low incidence of this tumor is the limiting factor in conducting a prospective randomized comparative study between percutaneous and conventional surgical treatments. Nevertheless, we believe in the importance of comparing the results between the two treatment modalities to increase the level of evidence of the results obtained.
In conclusion, the direct injection of methylprednisolone and calcitonin inside the ABC cavities appears to be a safe and effective treatment, with no side effects similar to those usually seen in cases of infiltration of fibrosing agents. While it may appear promising, this treatment method requires further studies with a relevant sample to establish its true efficacy and safety. Our results lead us to the idea that surgery can be replaced in the future by hormone therapy. However, further experience with this treatment in this rare, aggressive bone tumor is needed. It remains unclear whether coadministration of methylprednisolone with calcitonin is advantageous; however, we conclude that intralesional calcitonin and methylprednisolone injection is an effective and minimally invasive method for an ABC treatment.
Ethical Approval
All procedures involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments.
Competing Interests
The authors declare that there is no conflict of interest regarding the publication of this paper.
References
- Jaffe HL, Lichtenstein L (1942) Solitary unicameral bone cyst: with emphasis on the roentgen picture, the pathologic appearance and the pathogenesis. Arch Surg 44: 1004-1025.
- Rapp TB, Ward JP, Alaia MJ (2012) Aneurysmal bone cyst.J Am AcadOrthopSurg 20: 233-241.
- BaÅŸarir K, PiÅŸkin A, George B, Yildiz Y, SaÄŸlik Y (2007) Aneurysmal bone cyst recurrence in children: a review of 56 patients.J PediatrOrthop 27: 938-943.
- Wang EH, Marfori ML, Serrano MV, Rubio DA (2014) Is curettage and high-speed burring sufficient treatment for aneurysmal bone cysts?ClinOrthopRelat Res 472: 3483-3488.
- Cottalorda J, Bourelle S (2006) Current treatments of primary aneurysmal bone cysts.J PediatrOrthop B 15: 155-167.
- Zhu S, Hitchcock KE, Mendenhall WM (2015) Radiation Therapy for Aneurysmal Bone Cysts.Am J ClinOncol.
- Varshney MK, Rastogi S, Khan SA, Trikha V (2010) Is sclerotherapy better than intralesional excision for treating aneurysmal bone cysts?ClinOrthopRelat Res 468: 1649-1659.
- Rastogi S, Varshney MK, Trikha V, Khan SA, Choudhury B, et al. (2006) Treatment of aneurysmal bone cysts with percutaneous sclerotherapy using polidocanol. A review of 72 cases with long-term follow-up.J Bone Joint Surg Br 88: 1212-1216.
- Adamsbaum C, Mascard E, Guinebretière JM, Kalifa G, Dubousset J (2003) IntralesionalEthibloc injections in primary aneurysmal bone cysts: an efficient and safe treatment.Skeletal Radiol 32: 559-566.
- Rossi G, Rimondi E, Bartalena T, Gerardi A, Alberghini M, et al. (2010) Selective arterial embolization of 36 aneurysmal bone cysts of the skeleton with N-2-butyl cyanoacrylate. Skeletal Radiol 39: 161-167.
- Szendröi M, Antal I, Liszka G, Kónya A (1992) Calcitonin therapy of aneurysmal bone cysts.J Cancer Res ClinOncol 119: 61-65.
- Shiels WE, Beebe AC, Mayerson JL (2016) Percutaneous Doxycycline Treatment of Juxtaphyseal Aneurysmal Bone Cysts.J PediatrOrthop 36: 205-212.
- Batisse F, Schmitt A, Vendeuvre T, Herbreteau D, Bonnard C (2016) Aneurysmal bone cyst: A 19-case series managed by percutaneous sclerotherapy.OrthopTraumatolSurg Res 102: 213-216.
- Gibbs CP, Hefele MC, Peabody TD, Montag AG, Aithal V, et al. (1999) Aneurysmal bone cyst of the extremities. Factors related to local recurrence after curettage with a high-speed burr.J Bone Joint Surg Am 81: 1671-1678.
- Rizzo M, Dellaero DT, Harrelson JM, Scully SP (1999) Juxtaphyseal aneurysmal bone cysts. ClinOrthopRelat Res: 205-212.
- Garg S, Mehta S, Dormans JP (2005) Modern surgical treatment of primary aneurysmal bone cyst of the spine in children and adolescents.J PediatrOrthop 25: 387-392.
- Seller K, Jäger M, Krämer R, Krauspe R, Wild A (2004) Occurrence of a segmental kyphosis after laminectomy of C2 for an aneurysmatic bone cysts--course and treatment strategy.Z OrthopIhreGrenzgeb 142: 83-87.
- Boriani S, De Iure F, Campanacci L, Gasbarrini A, Bandiera S, et al. (2001) Aneurysmal bone cyst of the mobile spine: report on 41 cases.Spine 26: 27-35.
- Rai AT, Collins JJ (2005) Percutaneous treatment of pediatric aneurysmal bone cyst at C1: a minimally invasive alternative: a case report.AJNR Am J Neuroradiol 26: 30-33.
- Ohashi M1, Ito T, Hirano T, Endo N (2008) Percutaneous intralesional injection of calcitonin and methylprednisolone for treatment of an aneurysmal bone cyst at C-2.J NeurosurgPediatr 2: 365-369.
- Gladden ML, BL Gillingham, W Hennrikus, LM Vaughan (2000) Aneurismal bone cyst of the first Cervical Vertebrae in a Child treated with percutaneous intralesional injection of calcitonin and methylprednisolone. A case report. Spine 25: 527-530.
- Tonomura ET1, Ramos P, Hemais PM, Marchiori E, Gasparetto EL (2008) Aneurysmal bone cyst at C2: imaging evaluation after intralesional injection of calcitonin and methylprednisolone.ArqNeuropsiquiatr 66: 711-715.
- Capanna R, Bettelli G, Biagini R, Ruggieri P, Bertoni F, et al. (1985) Aneurysmal cysts of long bones.Ital J OrthopTraumatol 11: 409-417.
- Enneking WF (1986) A system of staging musculoskeletal neoplasms.ClinOrthopRelat Res pp: 9-24.
- McQueen MM, Chalmers J, Smith GD (1985) Spontaneous healing of aneurysmal bone cysts. A report of two cases.J Bone Joint Surg Br 67: 310-312.
- Enneking WF, Dunham W, Gebhardt MC, Malawer M, Pritchard DJ (1993) A system for the functional evaluation of reconstruction procedures after surgical treatment of tumors of musculoskeletal system. ClinOrthop 286: 241-246.
- Zehetgruber H1, Bittner B, Gruber D, Krepler P, Trieb K, et al. (2005) Prevalence of aneurysmal and solitary bone cysts in young patients.ClinOrthopRelat Res 439: 136-143.
- Leithner A, Windhager R, Lang S, Haas OA, Kainberger F, et al. (1999) Aneurysmal bone cyst. A population based epidemiologic study and literature review. ClinOrthopRelat Res : 176-179.
- Panoutsakopoulos G, Pandis N, Kyriazoglou I, Gustafson P, Mertens F, et al. (1999) Recurrent t(16;17)(q22;p13) in aneurysmal bone cysts.Genes Chromosomes Cancer 26: 265-266.
- Leithner A1, Lang S, Windhager R, Leithner K, Karlic H, et al. (2001) Expression of insulin-like growth factor-I (IGF-I) in aneurysmal bone cyst.Mod Pathol 14: 1100-1104.
- Oliveira AM, Perez-Atayde AR, Dal Cin P, Gebhardt MC, Chen CJ, et al. (2005) Aneurysmal bone cyst variant translocations upregulate USP6 transcription by promoter swapping with the ZNF9, COL1A1, TRAP150, and OMD genes. Oncogene 24: 3419-3426.
- Ye Y, Pringle LM, Lau AW, Riquelme DN, Wang H, et al. (2010) TRE17/USP6 oncogene translocated in aneurysmal bone cyst induces matrix metalloproteinase production via activation of NF-kappaB.Oncogene 29: 3619-3629.
- Bollini G, Jouve JL, Cottalorda J, Petit P, Panuel M, et al. (1998) Aneurysmal bone cyst in children: analysis of twenty-seven patients.J PediatrOrthop B 7: 274-285.
- Topouchian V, Mazda K, Hamze B, Laredo JD, Penneçot GF (2004) Aneurysmal bone cysts in children: complications of fibrosing agent injection.Radiology 232: 522-526.
- Peraud A, Drake JM, Armstrong D, Hedden D, Babyn P, et al. (2004) Fatal ethibloc embolization of vertebrobasilar system following percutaneous injection into aneurysmal bone cyst of the second cervical vertebra. AJNR Am J Neuroradiol 25: 1116-1120.
- Meohas W, de Sá Lopes AC, da SilveiraMöller JV, Barbosa LD, Oliveira MB (2015) Parosteal aneurysmal bone cyst.Rev Bras Ortop 50: 601-606.
- Funakoshi Y, Shiono H, Inoue M, Kadota Y, Ohta M, et al. (2005) Glucocorticoids induce G1 cell cycle arrest in human neoplastic thymic epithelial cells.J Cancer Res ClinOncol 131: 314-322.
- Pelle DW, Ringler JW, Peacock JD, Kampfschulte K, Scholten DJ 2nd, et al. (2014) Targeting receptor-activator of nuclear kappaB ligand in aneurysmal bone cysts: verification of target and therapeutic response.Transl Res 164: 139-148.
- Docquier PL, Delloye C, Galant C (2010) Histology can be predictive of the clinical course of a primary aneurysmal bone cyst.Arch Orthop Trauma Surg 130: 481-487.
- Steffner RJ, Liao C, Stacy G, Atanda A, Attar S, et al. (2011) Factors associated with recurrence of primary aneurysmal bone cysts: is argon beam coagulation an effective adjuvant treatment?J Bone Joint Surg Am 93: e1221-1229.
Relevant Topics
- 3D Printing in Limb-Sparing Surgery
- Adamantinoma
- Aneurysmal Bone Cysts
- Chondrosarcoma
- Chordomas
- Cryosurgery
- Enchondroma
- Ewing’s Sarcoma
- Fibrous Dysplasia
- Giant Cell Tumor of Bone
- Immunotherapy for Osteosarcoma
- Liquid Biopsy in Orthopedic Oncology
- Malignant Osteoid
- Metastatic Bone Cancer
- Molecular Profiling of Bone Tumors
- Multilobular Tumour of Bone
- Orthopaedic Oncology
- Osteocartilaginous Exostosis
- Osteochondrodysplasia
- Osteoma
- Osteonecrosis
- Osteosarcoma
- Primary Bone Tumors
- Sarcoma
- Secondary Bone Tumours
- Targeted Therapy in Bone Sarcomas
- Tumours of Bone
Recommended Journals
Article Tools
Article Usage
- Total views: 16549
- [From(publication date):
March-2017 - Sep 02, 2025] - Breakdown by view type
- HTML page views : 15496
- PDF downloads : 1053