Role of Radiology in the Management of Diabetic Foot Infections: A Report of Three Cases
Received: 28-Apr-2018 / Accepted Date: 07-May-2018 / Published Date: 14-May-2018 DOI: 10.4172/2329-910X.1000267
Abstract
Diabetes because of its diverse effects on the lower extremity via vascular, neural and immunological affects can mask the local and systemic signs of infection, potentially misleading and delaying the diagnosis of infection especially in those with foreign body injuries. Accurate and prompt diagnosis of these anomalies is vital in the early management thus preventing further complications. Careful clinical assessment and imaging modalities are central to the diagnosis, which will help identify radiopaque and radiolucent objects and infections. These help in the better management of foot complications and contribute to better outcomes.
Keywords: Foreign body; Infection; Diabetic foot; Radiology
Introduction
Diabetes Mellitus is a silent disease leading to numerous complications amongst which foot related problems are very common and diverse. Diabetic foot infections (DFI) are one of the main reasons for hospitalization and are also a common cause of amputation worldwide [1]. DFI arises from an array of sub clinical problems including peripheral neuropathy, peripheral arterial disease, infection, high pressure points, deformities, injuries etc. Loss of feeling due to peripheral neuropathy puts the individual at a tremendous risk of infection making the individual ignore their foot even after exposure to trauma or injuries [2]. Foreign body injuries are one of the most common problems that are encountered especially in country like India where barefoot walking is common practice because of sociocultural and religious beliefs. The common foreign bodies that are noticed on a routine basis are sewing needles, wooden splinters, glass particles, cloth fibers, stones etc. Foreign body penetration is considered to be a contamination and there are higher chances of infection appearing as cellulitis, abscesses and if delayed can even result in amputation of the toes or part of the foot [3]. Foreign bodies are commonly found in patients with Diabetic neuropathic foot which can predispose to infection [4,5]. History, careful clinical assessment and radiological imaging are central to the diagnosis process. In DFIs, plain X-ray of foot and ankle can be used to evaluate for foreign bodies, soft tissue gas, bony destruction and deformity [6]. Plain radiography and or ultrasound performed with high frequency linear probes are commonly used to detect and assist with removal of foreign bodies. These are usually hyperechoic on ultrasound with a surrounding rim of hypoechoic inflammatory and granulomatous tissue [7,8]. Aggressive medical management of these infections is crucial to prevent amputation. A thorough debridement, antibiotics, radiographs, ultrasound and local wound care are all essential. Hence early exploration and removal of foreign body will lessen the risk of infection, and help save the foot or a limb.
Case Discussion
Case 1
A 65-year-old man, a case of type 2 diabetes mellitus- an engineer by profession, presented to the outpatient department of Chellaram Diabetes Institute (CDI), Pune with a red swollen hot foot. He had history of fever and chills two days to the presentation and had simultaneously noticed redness and swelling of the right foot. He was known case of type 2 diabetes mellitus and hypertension and has peripheral neuropathy.
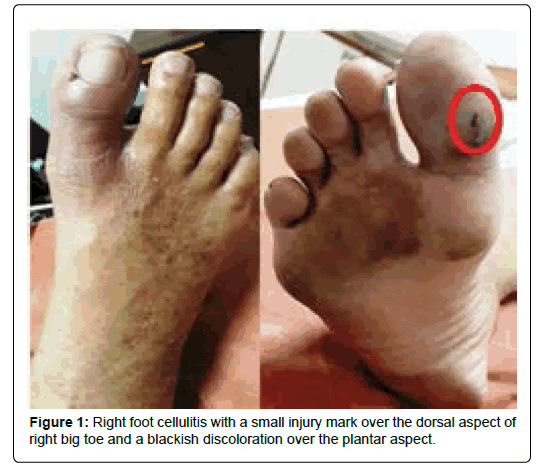
He is on insulin and oral anti-diabetic drugs for diabetes. and Oral anti-diabetic drugs (OADs) for his diabetes. On examination, his vitals were normal except had a temperature of 101° Fahrenheit. He denied any history of injury or trauma. His pedal pulse was palpable with good blood flow with an ankle brachial index (ABI) of 1 on both sides. His neurological evaluation showed inability to perceive 50 volt vibration threshold suggestive of severe peripheral neuropathy. His right foot had cellulitis with a small injury mark over the dorsal aspect of right big toe and a blackish discoloration over the plantar aspect of big toe (Figure 1). Foot was warm and painful on manipulation. His initial blood parameters were normal except the high glycemic levels in blood which showed fasting blood glucose of 280 mg/dl and post prandial blood glucose levels of 326 mg/dl. A plain radiograph and local ultrasound of the foot were ordered.
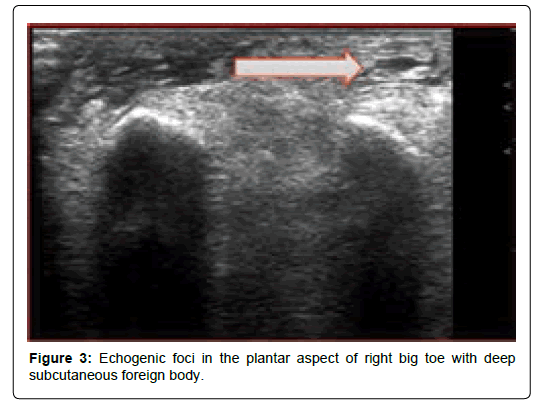
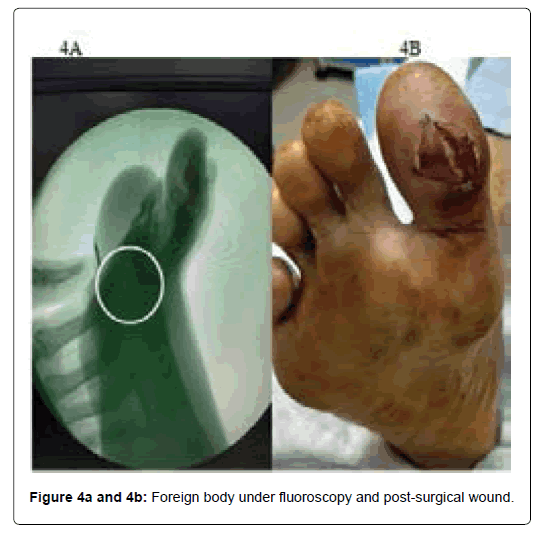
X-ray of the foot showed a radiopaque object of size 5 mm × 1 mm on the plantar aspect of right big toe (Figure 2) and the local ultrasound of the foot showed an echogenic foci on the plantar aspect of right big toe with deep subcutaneous foreign body, intercepted with the deep subcutaneous plane (Figure 3).
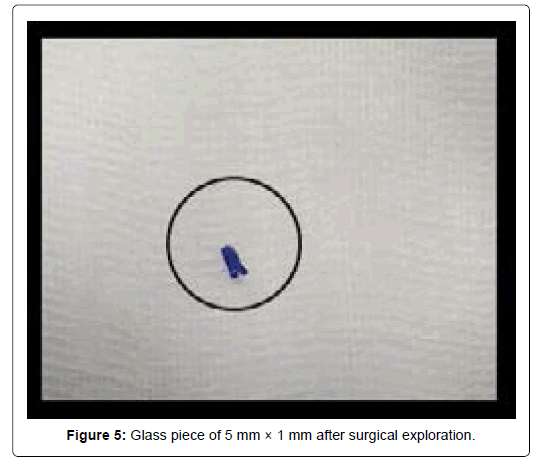
He was taken up for surgical exploration with the help of fluoroscopy (Figure 4a and 4b). There was a glass piece of 5 mm X 1 mm (Figure 5) pierced in with pus pockets and frank pus drained. Pus for culture and sensitivity was sent which showed no growth after 48 hours of incubation period. He was started on empirical intravenous (IV) antibiotics for 7 days. He was advised to do daily dressing, oral antibiotics, pain was better after exploration. After 1 month of surgical exploration of foreign body, his wound healed and he was back for routine daily activities.
Case 2
68 years male, farmer by profession presented to outpatient department of CDI, Pune with a small abscess over the right foot dorsal aspect. He was walking in a farm when he sustained an injury to his right foot dorsum 6 days ago and he found that the foreign body pierced in, and soon the relative who accompanied him removed it, later he learned that there may be a part of the foreign body left embedded deep and noticed swelling after 2 days. He then consulted a local doctor who had removed the foreign body. After 3 days of post removal still there was no clinical improvement and the foot problem was progressing so he decided to visit a diabetic center. Thus presented to Chellaram Diabetes Institute. He was diagnosed to have type 2 diabetes 10 years ago and is on Insulin and OADs for diabetes, he was also diagnosed to have microvascular complications. On physical examination there was no fever, vitals were normal. His right foot was slightly edematous with a small abscess near 5th Metatarsal with pain (Figure 6) and had warmth as compared to the contralateral side. His dorsalis pedis and posterior tibial pulses were palpable and the hand held Doppler study showed absolutely normal blood circulation with an ABI of 0.9 on the right and 0.96 on the left and he had severe peripheral neuropathy when tested with vibrometer.
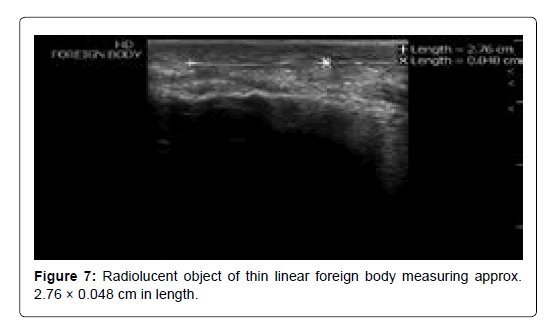
His plain radiograph of the foot showed no evidence of foreign body or osteomyelitis. He was treated with empirical IV antibiotics and incision and drainage of the abscess was performed bedside. The pus was send for culture and sensitivity which showed pseudomonas infection subsequently treated with culture specific antibiotics, the cellulitis reduced but there was still pus discharge from the wound even after 3 days. A local ultrasound of the foot was ordered to look at the radiolucent object and found to have a thin linear foreign body measuring approximately 2.76 X 0.048 cms in length (Figure 7) in subcutaneous plane of dorsal aspect of right foot overlying fifth metatarsal.
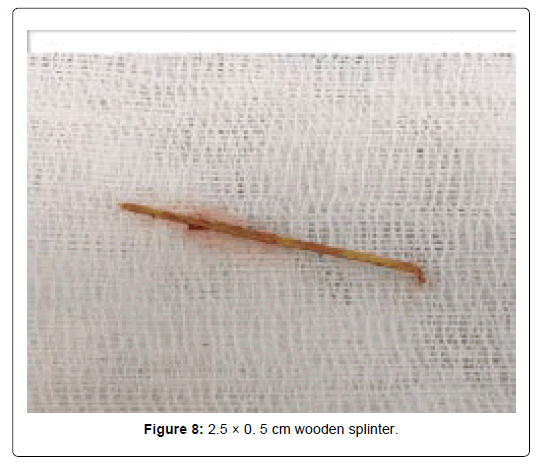
He was taken for surgical exploration of the foreign object with drainage of collection under spinal anesthesia, a 2.5×0. 5 cm wooden splinter (Figure 8) was removed and the wound was left opened (Figure 9). The wound healed completely in 8 weeks time after following all standard care for the management of diabetic foot. He was quite happy and was back to his routine work.
Case 3
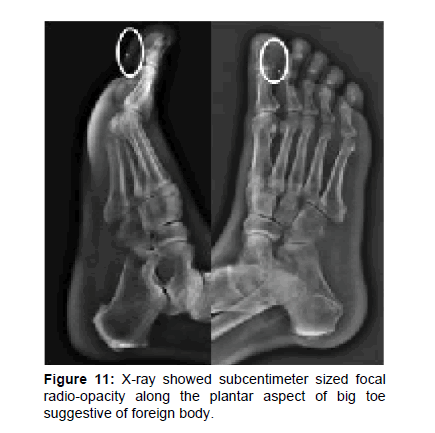
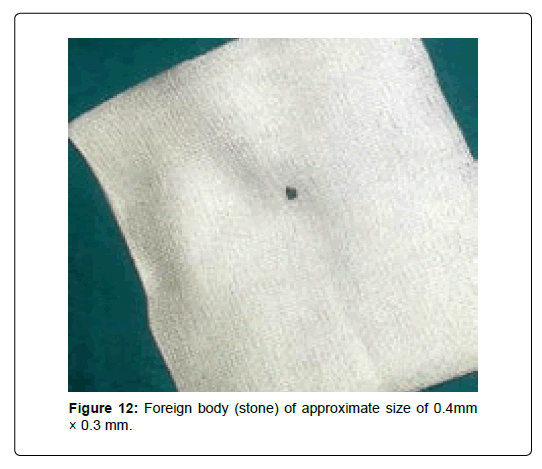
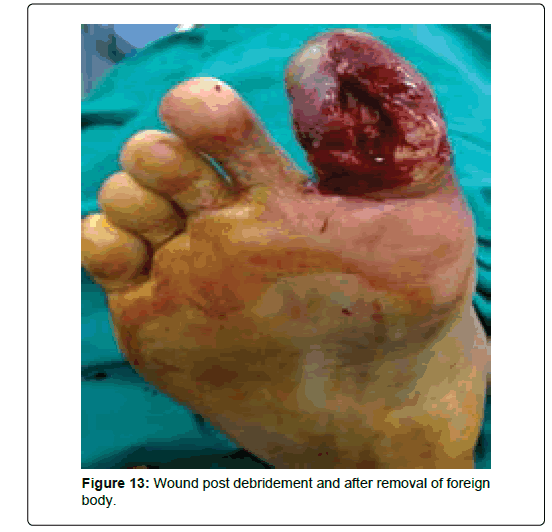
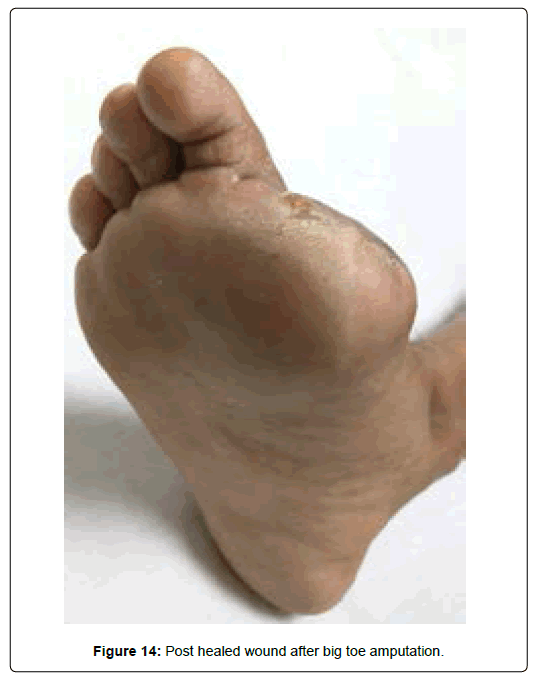
61 year old gentleman, a lecturer by profession presented to CDI, Pune with right big toe infection (Figure 10) since 7 days. He a known case of type 2 diabetes and hypertension since 15 years and he is on combination of Insulin and OADs for the same. On Examination his pedal pulse was palpable, he was febrile on presentation with temperature of 100.2° Fahrenheit, and other vitals were with in normal limits. His other blood parameters except serum creatinine and blood glucose levels was normal. Serum creatinine was 1.3 mg/dl, three month average blood glucose levels i.e., HbA1c was 15.4%, fasting blood glucose value was 335 mg/dl and post prandial blood glucose levels were 295 mg/dl. His foot was hot as compared to contralateral side, the right big toe was red, swollen, and tender and was smelling foul (Figure 10). The toe condition was very bad and was looking dusky on presentation. He gave a history of barefoot walking in temple 5 days prior to the infection and he had consulted a local doctor for the same who had prescribed antibiotics for the same, thus he presented to CDI for further evaluation and management. Upon investigating his blood flow towards the feet was normal. He was diagnosed to have severe peripheral neuroapthy. X-ray was ordered to look at the cause of infection and foreign body penetration. X-ray evaluation showed subcentimeter sized focal radio-opacity along the plantar aspect of big toe suggestive of foreign body (Figure 11). He was started on empirical antibiotics and insulin infusion and other related medications. He was taken up for immediate surgical intervention of foreign body under regional anesthesia and found to have foreign body (stone) of approximate size of 0.4 mm × 0.3 mm (Figure 12), infected tissue debrided and the wound was left open (Figure 13). Pus and deep tissue was send for culture and sensitivity which showed methicillin resistant staphylococcus aureus accordingly culture specific antibiotics were added. After 2 days of post-surgery there was no clinical improvement of the wound and thus right big toe amputation under ankle block was performed. All standard care of wound care management was followed including offloading, dressings etc., after 12 weeks of time patient wound completely healed (Figure 14) and patient was back to routine work with appropriate footwear.
Discussion
Foreign body injuries are a routinely encountered problem in diabetic foot care. Most of these injuries occur due to thorn or wooden splinters embedded inside the soft tissue [9]. Apart from the thorn and wooden splinters, fishhooks, glass particles, pencil lead or graphite and metallic foreign bodies are also commonly reported. Penetrating injuries through footwear are also seen on a regular basis especially in farmers and labourers. Suspected foreign body injuries require careful clinical examination and prompt evaluation. Foreign body injuries are frequently missed on initial evaluation [10,11]. A positive history of a foreign body may be obtained in some cases while taking history. An unrecognized or unnoticed foreign body can lead to acute or chronic infection [12]. Delayed diagnosis of foreign bodies can present as localized cellulitis, abscesses, or in the worse scenario the individual may require amputation of the toes or part of the foot. Imaging technique that are commonly used for detecting foreign bodies are plain radiographs, fluoroscopy, computer tomography (CT), magnetic resonance imaging (MRI) and ultrasound [13]. Radiological evaluation plays an important role in detecting radiopaque and radiolucent objects. Thus it should be carried out in all the subjects with suspected foreign body injuries after a careful physical examination [14]. Radiographs are considered to be the first line investigation when it comes to foreign body evaluation, as radiographs are noninvasive, inexpensive, widely available, easy to interpret, and they can provide positional information which helps in foreign body removal [13,15]. Radiolucent objects may not be traced on radiographs, thus ultrasound, computed tomography or magnetic resonance imaging for foreign body detection is recommended [16,17]. The information on the depth, location and number of foreign bodies can be identified by radiological evaluation which will help the appropriate line of treatment plan.
Radiographs are most useful in detecting radiopaque foreign bodies with sensitivities above 95% with adequate penetration and multiple views [13] but sensitivity of non-radiopaque foreign bodies is low [18,19]. Another study showed a sensitivity of 100% in detecting metal particle but missed 93% of wood and 25 percent of glass particle [19].
Fluoroscopy can be useful in foreign body removal with C-arm. This technique helps real-time radiographic visualization and help in precisely locating the foreign body thus making it easy for removal [20]. Ultrasound (US) allows detection of a variety of soft-tissue foreign bodies, including wooden splinters, glass particles, metal, and plastic objects, along with evaluation of their associated soft-tissue. The use of ultrasound for detecting foreign bodies has been widely used because of increased availability, lack of radiation exposure, safety, and sensitivity with detection of certain types of foreign bodies [21,22]. US is a highly sensitive and accurate modality in detecting radiolucent foreign bodies that are difficult to be visualized on standard radiographs with and accuracy of 90.2%, sensitivity of 97.9%, and positive predictive value (PPV) of 92% [23]. Reports have shown improved sensitivities of using ultrasound in identifying foreign bodies like gravel, metal, wood, glass, and plastic [24]. In a randomized blinded study done on chicken thigh model, use of ultrasound has shown to have a sensitivity of 90% in identifying non-radiopaque foreign bodies, such as wood and rubber [24]. Emergency ultrasound guidelines recognize foreign body detection and removal as a unique and evolving application of emergency ultrasound [25]. All the above investigation help in appropriate diagnosis and early management of foreign bodies, thus preventing major issues of infection, even amputation by saving the limb.
Conclusion
The treatment of DFI should be aimed at proper diagnosis with the help of radiological tools which help in the appropriate treatment plan. Right decision on surgical exploration to remove the foreign body is vital for which imaging plays an important role in the assessment and management of diabetic foot infections. The first line evaluation in case of foot infection is radiogram of the foot. The real‑time high‑frequency USG is a highly sensitive and accurate tool for detecting and removing radiolucent foreign bodies which are difficult to be visualized by routine radiography.
Conflict of Interest
Authors declare that there is no conflict of interest.
References
- Lipsky BA, Tabak YP, Johannes RS, Vo L, Hyde L, et al. (2010) Skin and soft tissue infections in hospitalized patients with diabetes: Culture isolates and risk factors associated with mortality, length of stay and cost. Diabetologia 53: 914-923.
- Alfred RH, Jacobs R (1984) Occult foreign bodies in the foot. Foot Ankle 4: 209-211.
- Russell JM, Peterson JJ, Bancroft LW (2008) MR imaging of the diabetic foot. Magn Reson Imaging Clin N Am 16: 59–70.
- Peterson JJ, Bancroft LW, Kransdorf MJ (2002) Wooden foreign bodies: Imaging appearance. Am J Roentgenol 178: 557–562.
- Wukich DK, Armstrong DG, Attinger CE, Boulton AJ, Burns PR, et al. (2013) Inpatient management of diabetic foot disorders: A clinical guide. Diabetes Care 36: 2862-2871.
- Boyse TD, Fessell DP, Jacobson JA, Lin J, van Holsbeeck MT, et al. (2001) US of softtissue foreign bodies and associated complications with surgical correlation. Radiographics 21: 1251–1256.
- Fessell DP, van Holsbeeck MT (1999) Foot and ankle sonography. Radiol Clin North Am 37: 831–858.
- Borgia CA (1963) An unusual bone reaction to an organic foreign body in the hand. Clin Orthop 30: 188-193.
- DeBoard RH, Rondeau DF, Kang CS, Sabbaj A, McManus JG (2007) Principles of basic wound evaluation and management in the emergency department. Emerg Med Clin North Am 25: 23-39.
- Anderson MA, Newmeyer WL, Kilgore ES (1982) Diagnosis and treatment of retained foreign bodies in the hand. Am J Surg. 144: 63-67.
- Greene WB (1989) Unrecognized foreign Body as a focus for delayed serratia marcescenes osteomyelitis and septic arthritis: Two case reports. J Bone Joint Surg Am 71: 754–757.
- Capellan O, Hollander JE (2003) Management of lacerations in the emergency department. Emerg Med Clin North Am 21: 205-231.
- Naraynsingh V, Maharaj R, Dan D, Hariharan S (2011) Puncture wounds in the diabetic foot: importance of X-ray in diagnosis. Int J Low Extrem Wounds 10: 98–100.
- Bradley M (2012) Image guided soft-tissue foreign body extraction success and pitfalls. Clin Radiol 67: 531-534.
- Banerjee B, Das RK (1991) Sonographic detection of foreign bodies of the extremities. British J Radiology 64: 107-112.
- Mizel MS, Steinmetz ND, Trepman E (1994) Detection of wooden foreign bodies in muscle tissues: Experimental comparison of C.T, MRI and ultrasonography. Foot Ankle International15: 437-443.
- Blankstein A, Cohen I, Heiman Z, Salai M, Heim M, et al. (2000) Localization, detection and guided removal of soft tissue in the hands using sonography. Arch Orthop Trauma Surg 120: 514-517.
- Levine MR, Gorman SM, Young CF, Courtney DM (2008) Clinical characteristics and management of wound foreign bodies in the ED. Am J Emerg Med 26: 918-922.
- Crawford R, Matheson AB (1989) Clinical value of ultrasonography in the detection and removal of radiolucent foreign bodies. Injury 20: 341-343.
- Teng M, Doniger SJ (2012) Subungual wooden splinter visualized with bedside sonography. Pediatr Emerg Care 28: 392-394.
- Kim SW, Youn SK, Kim JT, Cho SH, Kim YH, et al. (2012) Management of an unusual craniofacial impalement injury by a metallic foreign body. J Craniofac Surg 23: 140-146.
- Tahmasebi M, Zareizadeh H, Motamedfar A (2014) Accuracy of ultrasonography indetecting radiolucent soft tissue foreignbodies. Indian J Radiol Imaging 24: 196-200.
- Turkcuer I, Atilla R, Topacoglu H, Yanturali S, Kiyan S, et al. (2006) Do we really need plain and soft-tissue radiographies to detect radiolucent foreign bodies in the ED? Am J Emerg Med 24: 763-768.
- American College of Emergency Physicians (2009) Emergency ultrasound guidelines. Ann Emerg Med 53: 550-570.
Citation: Kavitha KV, Tathare S, Kumbhar V, Bidaye A, Panse R, et al. (2018) Role of Radiology in the Management of Diabetic Foot Infections: A Report of Three Cases. Clin Res Foot Ankle 6: 267. DOI: 10.4172/2329-910X.1000267
Copyright: © 2016 Kavitha KV, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 9686
- [From(publication date): 0-2018 - Aug 20, 2025]
- Breakdown by view type
- HTML page views: 8731
- PDF downloads: 955