Snuff (Tomback) Dipping Verrucous Carcinoma: A Case Report
Received: 10-Feb-2017 / Accepted Date: 25-Feb-2017 / Published Date: 04-Mar-2017 DOI: 10.4172/2161-119X.1000296
Abstract
Oral verrucous carcinoma is a clinico-pathological variant of OSCC. The most frequent affected sites intraoral are the mucosa of the buccal area and alveolus, also the gingiva. It’s a locally aggressive tumor. Generally it is related to tobacco use specially the chewed and snuffed types, hence it named “snuff dipper's cancer’’, the recurrence is high due to the dysplastic cells around the tumor. This is a case of Sudanese male diagnosed with verrucous carcinoma in the Oral and Maxillofacial Clinic.
Keywords: Verrucous carcinoma; Oral cavity; Snuffs dipping
254718Introduction
Verrucous carcinoma is one of squamous cell carcinoma variants that have a low- malignancy grading, it is rarely show distant metastasis, earliest it describe by several names; florid papillomatosis, epithelioma cuniculatum, verrucous squamous cell carcinoma, oral florid verrucosis, verruca acuminata, papillomatosis mucosa carcinoides, snuff dipper's cancer, Buschke-Loewenstein tumor, and carcinoma cuniculatum. In 1970s it names as "verrucous carcinoma" or "Ackerman's tumor" [1,2].
It tends to grow gradually, invade locally with no metastasis. Clinically it resembles a cauliflower and present as white, outward growing plaque attached by a wide base, warty with no pain. Men at the age of sixties to seventies affected more than women. Intraoral, the most frequent sites involved are; the mucosa buccally, the alveolar crest of the mandible, tongue and gingiva [3]. Chewing tobacco is a major etiological factor. Lesions frequently grow at the site of habitually placed tobacco [4].
Surgical excision is the preferred treatment, even though surgery can give satisfactory results, but frequent revision is obligatory due to the increase risk of second tumors [5]. Surgery followed by radiotherapy is second most superior way of management especially in advanced cases; the Recurrence is common in cases managed by single modality treatment [6]. There is high possible presence of adjacent altered mucosa around the tumor, this confirm the importance of a wider surgical excision with adequate margins and need for close follow up [7].
Case Scenario
A Sudanese male 64 years old presented with painless whitish ulcerative lesion started 10 months ago. The patient had a smoking history for 25 years, dipped snuff for more than 20 years (he did not rinse after use the snuff and sleep with it), denied any history of alcohol abuse and he had controlled hypertension.
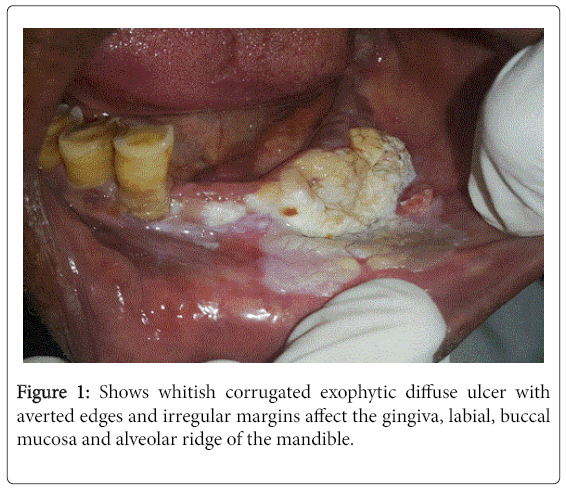
Clinical examinations showed a non-tender whitish corrugated exophytic diffuse ulcer with averted edges and irregular margins without apparent discharge affect the gingiva, labial, buccal mucosa and alveolar ridge from the left side of the mandible and cross the midline (Figure 1). No sub- mandibular or cervical lymphadenopathy.
Incisonal biopsies from different sites (field mapping) were examined Histopathological and revealed characteristic features of verrucous carcinoma with no evidence of squamous cell carcinoma. CT scan with contrast showed no apparent sub-mandibular or cervical lymph nodes with slight bone erosion in the affected region of the mandible.
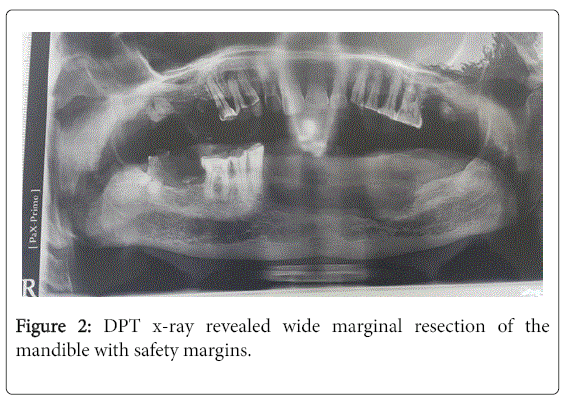
Treatment modality was resection of the tumor and the marginal bone of the mandible anterior, with a safety margins. Post-operative examination of the tumor’s margins histological revealed all margins were free.
Post-operative digital OPG revealed wide marginal resection of the mandible (Figure 2). Patient was planned for continuous meticulous follow-up.
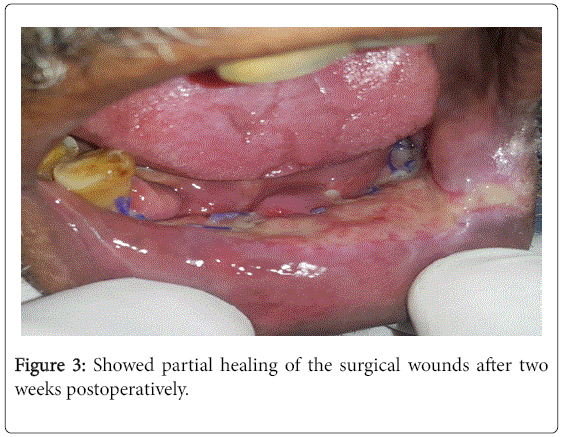
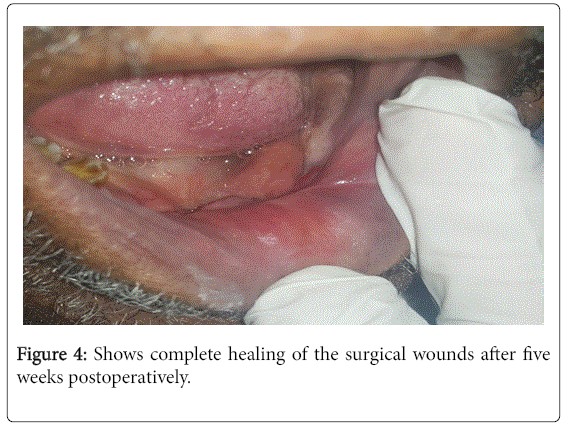
Figures 3 and 4 showed healing of the surgical wound after two and five weeks, respectively.
Discussion
Oral Verrucous carcinoma is a variant of OSCC confirm a squat degree of malignancy, appear most commonly in the oral region with a percentage of 2-12% of all neoplasm’s [2]. It has a unique appearance clinically; it is typically large in size, exophytic, soft, irregular, slow growing tumors. It is usually present as a diffuse, clear bounded, elevated whitish outward growing with no pain looks like a cauliflower [3,8,9].
The most common age group is the sixties and seventies with a male predilection [10]. In literature the most common site reported was the buccal mucosa [11,12] while other authors reported more involvement of the alveolar ridge and gingiva [13,14] in this case the clinical findings are the same as to the above regarding site, age and characteristic features.
In verrucous carcinoma, regional lymph nodes are often tender and enlarged because of inflammatory involvement, simulating metastatic tumor [15], lymph nodes were not affected in our cases.
The causative factors of Verrucous carcinoma could be Human papilloma virus (HPV), Smoking, bad oral hygiene, leukoplakic lesions oral lichenoid [10]. Tobacco was the major origin factorof verrucous lesions often develop at the site where the tobacco was placed habitually [3], which was in agreement with the Sudanese patient causative factor, snuff dipping (tombak).
Surgery is the first line of treatment for verrucous carcinoma [1]. In current case, patient had been treated with surgical excision. Radiotherapy may alter the tumor nature into squamous cell carcinoma poorly differentiated type [16].
In cases of non surgical intervention, other treatment modalities such as cytostatic drugs may be preferred; α interferon (IFN) seems to support the therapy by delaying the growth of the tumor but does not take the place of surgery alone [6].
Conclusion
Verrucous carcinoma is characteristic because it tends to invade locally, no metastasize and has unique clinical features. Multiple biopsies must be done to exclude classic squamous cell component. Also recommends complete excision and close follow-up, more care must be achieved by clinicians regarding warty and exophytic lesions intraorally.
References
- Walvekar RR, Chaukar DA, Deshpande MS, Pai PS, Chaturvedi P, et al. (2009) Verrucous carcinoma of the oral cavity: A clinical and pathological study of 101 cases. Oral Oncol 45: 47-51.
- Alkan A, Bulut E, Gunhan O, Ozden B (2010) Oral verrucous carcinoma: a study of 12 cases. Eur J Dent 4: 202-207.
- Kamala KA, Sankethguddad S, Sujith SG (2015) Verrucous carcinoma of oral cavity-a case reportwith review of literature. Int J Health Sci Res 5: 330-334.
- Kaushal N, Madan N (2009) Verrucous carcinoma of the oral cavity: Case report. The Internet Journal of Geriatrics and Gerontology 6: 1-4.
- Liao CT, Kang CJ, Chang JT, Wang HM, Ng SH, et al. (2007) Survival of second and multiple primary tumors in patients with oral cavity squamous cell carcinoma in the betel quid chewing area. Oral Oncol 43: 811-819.
- McClure DL, Gullane PJ, Slinger RP, Wysocki GP (1984) Verrucous carcinoma--changing concepts in management. J Otolaryngol 13: 7-12.
- Slaughter DP, Southwick HW, Smejkal W (1953) Field cancerization in oral stratified squamous epithelium. Clinical implications of multicentric origin. Cancer 6: 963–968.
- Schrader M, Laberke HG, Jahnke K (1987) Lymphatic metastases of verrucous carcinoma (Ackerman tumor). HNO 35: 27-30.
- Rajendran R (2006) Benign and malignant tumors of the oral cavity. In: Rajendran R, Sivapathasundaram B (eds.) Shafer's textbook of oral pathology. 5th. edition. Elsevier, pp: 309-356.
- Chen HM, Chen CT, Yang H, Lee MI, Kuo MY, et al. (2005) Successful treatment of anextensive verrucous carcinoma with topical 5 aminolevulinic acid mediated photodynamic therapy. J Oral Pathol Med 34: 253-256.
- Rekha KP, Angadi PV (2010) Verrucous carcinoma of the oral cavity: A clinico-pathologic appraisal of 133 cases in Indians. Oral Maxillofac Surg 14: 211-218.
- Huang TT, Hsu LP, Hsu YH, Chen PR (2009) Surgical outcome in patients with oral verrucous carcinoma: Long-term follow-up in an endemic betel quid chewing area. ORL J Otorhinolaryngol Relat Spec 71: 323-328.
- Gandolfo S, Castellani R, Pentenero M (2009) Proliferative verrucous leukoplakia: A potentially malignant disorder involving periodontal sites. J Periodontol 80: 274-281.
- Bagan JV, Jiménez-Soriano Y, Diaz-Fernandez JM, MurilloCortés J, Sanchis-Bielsa JM, et al. (2011) Malignant transformation of proliferative verrucous leukoplakia to oral squamous cell carcinoma: A series of 55 cases. Oral Oncol 47: 732-735.
- Shafer WG, Hine MK, Levy BM (1983) Benign and malign tumors of the oral cavity. In: A Textbook of Oral Pathology. Philadelphia, WB: Saunders Company, pp: 127-130
- Kawakami M, Yoshimura K, Hayashi I, Ito K, Hyo S (2004) Verrucous Carcinoma of the Tongue: Report of two cases. Bulletin of the Osaka Medical College 50: 19-22.
Citation: Eltohami YI, Alim NE, Suleiman AM, Abuaffan AH (2017) Snuff (Tomback) Dipping Verrucous Carcinoma: A Case Report. Otolaryngol (Sunnyvale) 7:296. DOI: 10.4172/2161-119X.1000296
Copyright: © 2017 Eltohami YI, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4954
- [From(publication date): 0-2017 - Jul 12, 2025]
- Breakdown by view type
- HTML page views: 4040
- PDF downloads: 914