Success in the Treatment of Periapical Implant Lesion: Case Report
Received: 22-Apr-2016 / Accepted Date: 18-Jun-2016 / Published Date: 28-Jun-2016
Abstract
The Implant periapical lesion (IPL=Implant Periapical Lesion) is an infectious-inflammatory alterations surrounding an implant apex. The diagnosis is based on the clinical manifestations as pain, swelling, presence of fistula and radiological findings, where a radiolucent lesion can be seen in the periapical area. It is apparent that IPL has a multifactorial background, mainly caused by the presence of a pre-existing microbial pathology or surgical trauma during implant surgery. To date, there are no clinical protocols for managing IPL. This case report presents a case history related to IPL, which was caused by a pre-existing lesion. For the treatment of the infected form of IPL, a sequential surgical therapy can be utilized, if there is no loss of the implant stability. This includes surgical removal of the implant apical region, through debridement of the infected lesion, systemic antibiotics, and or guided bone regeneration. The intervention was aimed to stop the progression of osteolysis perimplant increasing the survival implant.
Keywords: Implant periapical lesion; Retrograde perimplantitis; Apical perimplantitis; Implant failure
78934Introduction
Implant failure due to apical pathology are conditions that have not been extensively studied nor reported in the literature. The active lesion periapical implant (IPL) or retrograde peri-implantitis has been described as an infectious-inflammatory alterations surrounding an implant apex. It’s an extremely rare event that occurs at a rate between 0.3% -1.8% of Osseo integrated implants [1,2]. IPL is often associated with implants that may have been overheating or excessive tightening the implant during implant surgery, or implants that are located adjacent to a tooth with endodontic/periodontal lesions [1-3]. Diagnosis of IPL is clinic and radiographic. IPL can be classified into the in-active (noninfected) and infected forms [1]. The inactive form is asymptomatic and it is diagnosed because of the presence of radiolucency around the apex of the implant. This radiolucency is an apical scar caused by vertical over-preparation of the implant or by bone necrosis due to overheating during implant insertion.
There is no treatment that is required for the inactive form, but periodic monitoring of the lesion is recommended. In the active form, the lesion is symptomatic and requires treatment to avoid the progress of bone destruction. Symptoms and clinical signs which may appear are pain, swelling, suppuration and fistula; in the radiograph implant periapical radiolucency may be identified in some cases [1-6]. For the treatment of the infected form of IPL, surgical approaches have been advocated, including implant removal, resection of infected implant apices and guided bone regeneration [1-3,5,7-14]. This case report describe the treatment in a periapical lesion active surgical approach by means of excision of the cystic lesion with resection and subsequent implant periapical curettage implant with the glycerin aid.
Case Report
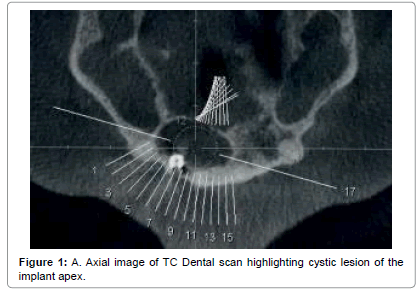
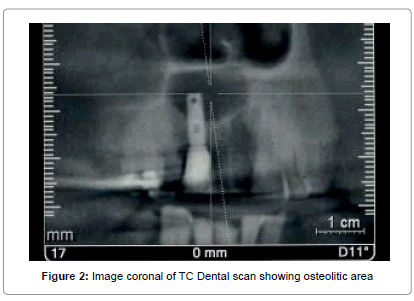
A Caucasian man of 52 year old presented to the Dental Clinic of University of Trieste in September 2014 for a osteolytic lesion of implant 12, detected by 5 years (Figures 1 and 2). The clinical history shows that his private dentist did not treated the lesion present on the element 12 was before replacement with osseointegrated implant titanium.
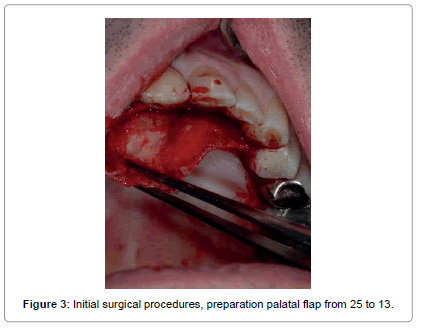
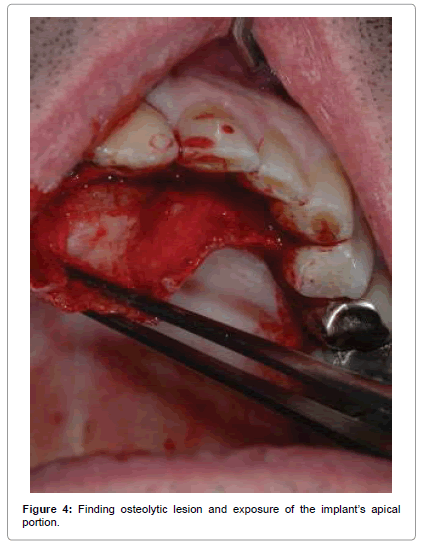
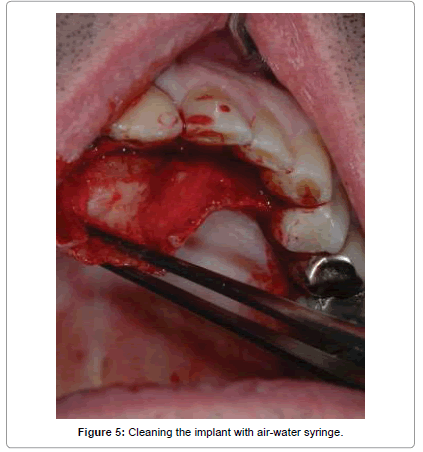
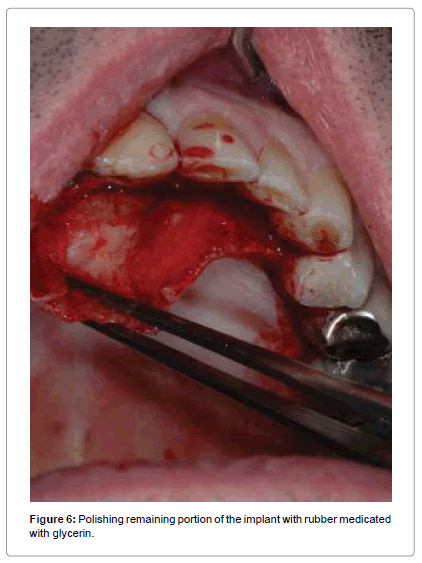
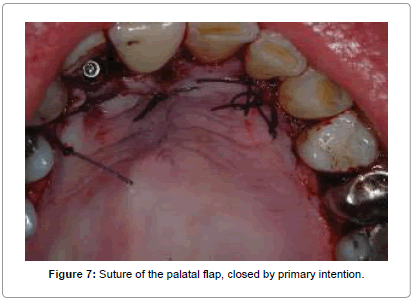
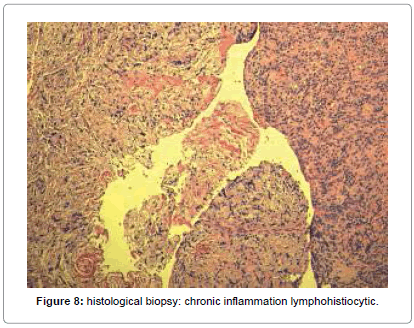
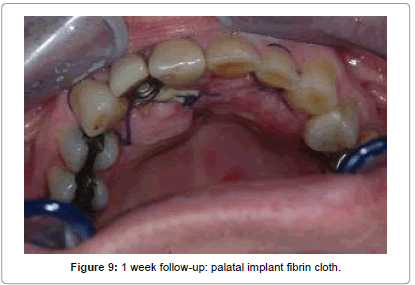
The surgical steps approached were the following: preparation of a total thickness element palatal flap from 13 to 25 (Figure 3), finding of cystic lesion origin on the palatal side (Figure 4), removal of alveolar lesion by Hemingway instruments, implant exposure and apicectomy made with tungsten drills on contra angle dental handpieces to 2 mm apical, cleaning cavity with air-water syringe (Figure 5), the remaining implant was polishing by glycerine medicated rubber mounted on micromotor (Figure 6), absorbable suture in Vicryl® 4.0 (Ethicon, Sommerville NJ, USA) (Figures 7 and 8), home therapy prescribed broad-spectrum antibiotic (amoxicillin associated with clavulanic acid: 1 × 1 g twice a day for 7 days), cortisone, (rinses with chlorhexidine 0.2%) and recommended post-operative home instructions. Planned follow-up at 1 week (Figure 9) for suture removal, at 4, 12 weeks and 24 weeks.
Discussion
This case report illustrates treatment by removal of only the involved portion of the implant, thereby maintaining the prosthesis. It has been proposed that the most likely causes are bacterial infection from either remnant of extracted natural teeth. The definitive histological examination showed the presence of a chronic inflammatory lesion sometimes a pattern granulomatoide at the apex implant, and negative prognostic factor predisposing to implant failure. The initial physical examination supported by the imaging excluded perimplantitis, while suggesting two diagnostic hypotheses: perimplantitis periapical retrograde versus implant insertion of pre-existing lesion. The situation inflammatory on going called for intervention in order to stop the perimplant osteolysis and stabilize the inevitable bone resorption at the injury that would be progressed within a year. As the stability implant is related directly to the quantity and quality of bone osseointegrated, in the case treated corresponded with a third of the size of the implant, in this case sufficient to maintain the stability also in relation with the respective masticatory load. The most studied treatment of implant apical lesions with no associated implant mobility is implant apical surgery [10]. Most authors curettage the lesion and irrigated with saline solutions [2-3,11,16-17]. Several agents have been applied for decontamination of the implant surgery, such as chlorexidine [3] or tetracycline pastes [3,7,16] but there is no evidence of the efficiency of any of them. The cavity was filled only by coagulation without affixing filler material in order to facilitate the healing, since the spirals implant may consider the bacterial biofilm responsible for the previous lesion and make failure a bone graft contextual. Properties of glycerine have been used to further decontaminate the coils implant.
Sometimes, bone regeneration materials are used, accompanied or not with tissue regeneration barriers, in order to achieve complete bone regeneration [2,8]. Other authors suggest sectioning the implant apex in those cases in which total removal of the granular tissue is not assured [7,11]. Scarano et al. [12] removed an implant in a patient because of pain persistence after treatment with analgesics. Oh et al. [18] decide to remove one implant which presented mobility. The optimal implan therapy would be minimizing the occurrence or consequences of implant periapical lesions by careful diagnosis, systematic treatment planning, and appropriate treatment procedures.
Conclusion
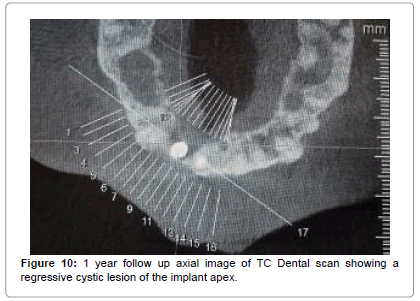
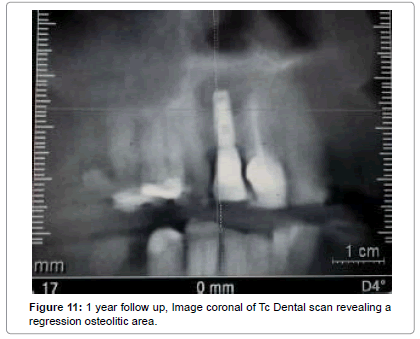
The intervention was aimed to stop the progression of osteolysis perimplant increasing the survival implant. The follow-up to one year has confirmed the healing post- intervention and the formation of new bone at the area of rarefaction (Figures 10 and 11). Within one year, given the resolution of the disease, we evaluated the opportunity to reintervene in order to fill the bone defect and align the prognosis to that of a plant in healthy tissue.
References
- Reiser GM, Nevins M (1995)The implant periapical lesion: etiology, prevention, and treatment. Compend Contin Educ Dent 16: 768-772.
- Quirynen M, Vogels R, Alsaadi G, Naert I, Jacobs R, et al.(2005) Predisposing conditions for retrograde peri-implantitis, and treatment suggestions. Clin Oral Implants Res 16: 599-608.
- Peñarrocha-Diago M, Boronat-Lopez A, GarcÃa-Mira B (2009) Inflammatory implant periapical lesion: etiology, diagnosis, and treatment-presentation of 7 cases. J Oral Maxillofac Surg J 67:168-73.
- Piattelli A, Scarano A, Balleri P, Favero GA (1998) Clinical and histologic evaluation of an active "implant periapical lesion": a case report. IntJ Oral Maxillofac Implants 13: 713-716.
- Rosendahl K, Dahlberg G, Kisch J, Nilner K (2009) Implant periapical lesion: A case series report. Swed Dent J 33: 49-58.
- Casado PL, Donner M, Pascarelli B, Derocy C, Duarte ME, et al. (2008). Immediate dental implant failure associated with nasopalatine duct cyst. Implant Dent 17: 169-175.
- Balshi SF, Wolfinger GJ, Balshi TJ (2007) A retrospective evaluation of a treatment protocol for dental implant periapical lesions: long-term results of 39 implant apicoectomies. Int J Oral Maxillofac Implants 22: 267-272.
- Quaranta A, Andreana S, Pompa G, Procaccini M (2014) Active implant peri-apicallesion: a case report treated via guided bone regeneration with a 5-year clinicaland radiographic follow-up. J Oral Implantol 40: 313-319.
- Dahlin C, Nikfarid H, Alsèn B, Kashani H (2009) Apical peri-implantitis: possible predisposing factors, case reports, and surgical treatment suggestions. Clin Oral Implant Res 11: 222-227.
- Peñarrocha-Diago M, Maestre-Ferriìn, Cervera-Ballester J, Peñarrocha-Oltra D (2012) Implant peripaical lesion: diagnosis and treatment. Med Oral Patol Cir Bucal 117: e1023-1027.
- Ayangco L, Sheridan PJ (2001) Development and treatment of retrograde peri-implantitis involving a site with a history of failed endodontic and apicoectomy procedures: a series of reports. Int J Oral Maxillofac Implants 16: 412-417.
- Scarano A, Di Domizio P, Petrone G, Iezzi G, Piatelli A (2000) Implant periapical lesion: a clinical and histologic case report. J Oral Implantol 26: 109-113.
- Ferreira JP, Santiago JF Jr, de Faria Almeida DA, Verri FR, et al. (2015) Existence of and predisposing factors for implant periapical lesions. de Souza Batista VE, J Craniofac Surg 26: 319-322.
- Jafarian M, Rayati F, Najafi E (2016) Successful treatment of a large implant periapical lesion that caused paraesthesia and perimandibular abscess. J Dent Res 13: 188-192.
- Qu C, Meng H, Han J (2014) Implant periapical lesion--a review and a case report with histological evaluation. Clin Oral Implants Res 25: 1099-1104.
- Attualluah K, Chee LF, Peng LL, Lung HH (2006) Management of retrograde perimplantitis: A clinical case report. J Oral Implantol 32: 308-312.
- Romanos GE, FroumS, Costa-Matins S, Meitner S, Tarnow DP (2011). Implant pericapical lesions: etiology and treatment options. J Oral Implantol 37: 53-63.
- Oh TJ, Yoon J, Wang HL (2003) Management of the implant periapical lesion: a case report. Implant Dent 12: 41-46.
Citation: Giulio M, Dennis V, Lorenzo B, Roberto MM (2016) Success in the Treatment of Periapical Implant Lesion: Case Report. J Med Imp Surg 1: 106.
Copyright: © 2016 Giulio M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 12683
- [From(publication date): 11-2016 - Aug 15, 2025]
- Breakdown by view type
- HTML page views: 11742
- PDF downloads: 941