Surgery for Paediatric Laryngotracheal Stenosis: A South Indian Experience
Received: 24-Jan-2019 / Accepted Date: 28-Jun-2019 / Published Date: 05-Jul-2019 DOI: 10.4172/2161-119X.1000373
Abstract
Introduction: Paediatric laryngotracheal stenosis (PLTS) encompasses a variety of congenital and acquired conditions which causes life threatening compromise of the airway, necessitating urgent essential intervention. The incidence of congenital and acquired laryngotracheal stenosis is on the rise. The commonest reason being premature birth owing to prolonged endotracheal intubation.
Methods: This is a retrospective study of 68 children with laryngotracheal stenosis of varied etiology who presented to our tertiary referral institute between June 2006 and December 2017. Various surgical modalities such as laser dilatation, Swiss roll or Montgomery T-Tube insertion, anterior cricoid split, costal cartilage interposition, tracheoplasty etc were employed. A reflection of the surgical management deployed in this cohort is discussed.
Results: All 68 children had meticulous endoscopic evaluation prior to surgical management. 6 (8.8%) patients underwent single stage procedure whereas 62 (91.17%) of patients had multiple procedures. 56 (82.35%) patients had successful decannulation post-treatment. 12 (17.64%) patients had persistent tracheostomy including 5 (7.35%) patients who were lost for follow up.
Conclusion: Paediatric laryngotracheal stenosis continues to pose challenges to the otolaryngologist. This entity requires accurate assessment and treatment needs to be customized for each individual. Our decade of experience managing this difficult entity is based on a rational management protocol as highlighted in this study. Such a systematic approach will give the best outcomes for this difficult entity.
Keywords: Paediatric laryngotracheal stenosis; Laser dilatation; Swiss roll stent; Montgomery T-tube; Costal cartilage interposition; Nitinol stent; Tracheoplasty
Introduction
Paediatric laryngotracheal stenosis (PLTS) encompasses a variety of congenital and acquired conditions which continues to be a challenging field for the otolaryngologist. About 90% of acquired stenosis have a history of intubation [1,2]. Selection of appropriate procedure differs with each case and the type of stenosis [3]. This study highlights a systematic approach to the surgical treatment for PLTS and its efficacy and outcomes, as experienced in the airway unit of a leading tertiary referral care ENT hospital in Chennai, South India [4]. This work proposes an useful management protocol for achieving the most optimal outcomes and thereby reflects on the high standard of care available for PLTS in South India.
Methodology
A consecutive series of 68 children with PLTS who had presented to our institute between June 2006 and December 2017 were retrospectively reviewed for this study, using the electronic medical records of the hospital. Their age ranged between 1 to 18 yrs (Mean age=5.6 yrs). All candidates were informed that their inpatient medical history was used anonymously for this study and appropriate written informed consents were taken. The institutional ethical board approved this work in Jan 2018.
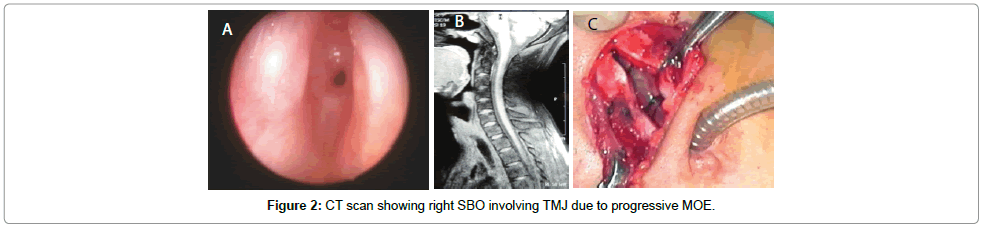
Details of medical history was collected with regards to the demography of the cohort. At first visit, a meticulous clinical history of each of these patients with regards to the aetiology and duration of stenosis had been obtained and a complete clinical assessment of laryngotracheal airway was done. Endoscopic assessment of their airway lumen had been done by rigid or fibre-optic laryngo-tracheobronchoscopy to assess the nature, site and extent of the stenosis. All stenosis were graded endoscopically. Radiological assessment of the airway with air tracheogram, Computerized Tomograms/Magnetic resonance imaging (MRI) scans of neck with upper chest were done, to study the airway lumen and soft tissue planes in order to plan the ideal surgical approach. Fitness for surgery under general anaesthesia was assessed with special emphasis on the pulmonary functions.
The data showed that various surgical modalities such as anterior cricoid split, costal cartilage interposition, laser procedures etc were employed and Hood’s stent, Montgomery T tube, silastic swiss roll or indwelling Nitinol tracheal stent were used. The stents were placed for an average period of 2 to 6 months and then airway was reassessed. Follow-up assessment was based on clinical and airway endoscopic evaluation under general anaesthesia. Majority of the patients had been successfully decannulated, although several patients needed multiple procedures (ranging from 2 to 7 stages). The average follow-up period after surgery was one year. The quantitative data collected as above was categorically analyzed to derive the following observations and results.
Results
A cohort of 68 children up to the age of 18 years who had presented with respiratory distress had undergone initial endoscopic assessment under general anaesthesia, and required subsequent interventions. Tables 1-3 provide a descriptive report of the aetiological spectrum, location and severity of stenosis and the management protocol undertaken.
| Etiology | Number of Patients (%) |
|---|---|
| Congenital | 16 (23.52) |
| Post Intubation | 38 (55.88) |
| Infection | 2 (2.94) |
| Iatrogenic | 2 (2.94) |
| Chemical Injury (Acid) | 2 (2.94) |
| Neoplasia | 4 (5.88) |
| Road Traffic Accident (RTA) | 4 (5.88) |
Table 1: Etiology of laryngotracheal stenosis in our cohort (N=68).
| Type | Number of Patients (%) |
|---|---|
| Supraglottic | 4 (5.88) |
| Glottic | 6 (8.82) |
| Glottic + Subglottic | 6 (8.82) |
| Subglottic | 12 (17.64) |
| Subglottic + Upper Tracheal | 19 (27.94) |
| Tracheal | 15 (22.05) |
| Bilateral Vocal Cord Paralysis with Glottic Web | 2 (2.94) |
| Laryngeal Cleft with SGS | 4 (5.88) |
Table 2: Site and type of PLTS.
| Primary pathology | Endoscopic only (%) | Open only (%) | Combined (%) |
|---|---|---|---|
| Supraglottic | 4 (100) | 0 | 0 |
| Glottic | 1 (16.66) | 2 (33.33) | 3 (50) |
| Glottic + Subglottic | 1 (16.66) | 1 (16.66) | 4 (66.66) |
| Subglottic | 5 (71.24) | 0 | 7 (28.57) |
| Subglottic + Upper Tracheal | 4 (21.05) | 5 (26.31) | 10 (52.63) |
| Tracheal | 4 (26.66) | 9 (60) | 2 (13.33) |
| Bilateral Vocal Cord Paralysis with Glottic Web | 2 (100) | 0 | 0 |
| Laryngeal Cleft with SGS | 4 (100) | 0 | 0 |
Table 3: Comparing site of pathology with treatment modality.
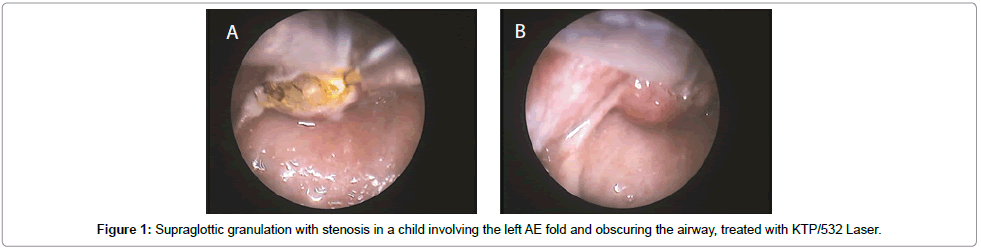
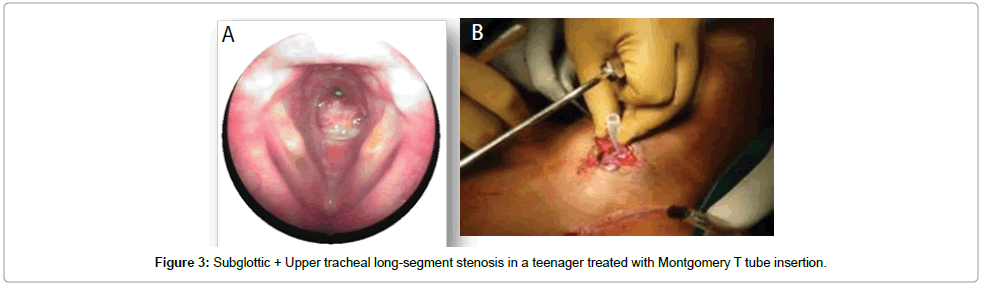
Surgical interventions for PLTS followed included endoscopic and external approaches predominantly focused on cricoid/sub-cricoid/ upper tracheal expansion. The endoscopic techniques includeddilatation procedures (with rigid dilators, bronchoscopes, or balloons), endoscopic radial resection (using KTP, CO2 laser) and endoscopic stent placement. The external or combined external + endoscopic approaches used included-laryngotracheal reconstruction with anterior costal cartilage grafting with stenting (silastic swiss-roll insertion in younger children and Montgomery T–tube or Hood’s stent in adolescents (Figures 1-3) and rarely posterior crico-tracheal resection with primary end-to-end anastomosis. The primary intervention and the subsequent interventions were both decided upon as per the meticulous assessment of the stenotic segment at that point in time, taking into consideration factors like the primary aetiology, previous intervention, current scarring/cicatrization (short vs. long segment, A-frame, etc.), associated evidence of infection, granulation and tightness of the stenotic segment. There was also the incidence of new segmental stricture due to repeated laryngotracheal surgery, especially due to collateral damage around the stenotic segment which had been operated upon and due to tracheostomy associated trauma, granulations and infections.
A total of 245 procedures were performed on these 68 patients with a mean of 3.6 procedures per patient. 56/68 (82.35%) patients had successful decannulation eventually. 6 (8.8%) patients underwent single-stage procedure whereas 62 (91.17%) patients had multiple surgical procedures on an average of 3.5 times (range 2 to 7 times). 12 (17.64%) patients had persistent tracheostomy including 5 (7.35%), who were lost for follow up. Re-stenosis was the most common complication, followed by excessive granulation and recurrent airway infections, which all together lead to the need for multiple interventions. Post-procedure wound care and tracheostomy care was paramount and was delivered by a dedicated pediatric airway allied rehabilitation team. Table 4 describes the cohort’s site-wise pathology with the primary and subsequent interventions attempted prior to achieving successful airway patency and eventual decannulation.
| No of Pts: N=62 | Site | Primary Procedure | Subsequent Procedures | Outcome | |||||
|---|---|---|---|---|---|---|---|---|---|
| 4 | Supra | L | L | L | L | L | L | No Trach | |
| 7 | G+SG | ACS, CCI, SR | L | D | L | De | |||
| 3 | G+SG | HS | SR | L | SR | SR | D | ACS, CCI, SR |
De |
| 4 | G+SG | L, ACS, CCI | L | L | L | L | De | ||
| 10 | SG | ACS, CCI, SR | D | T | Trach (No follow up) | ||||
| 6 | SG | ACS, CCI, SR | L | D | De | ||||
| 7 | SG+T | ACS, CCI, SR | SR | D | SR | De | |||
| 6 | SG+T | L, T-t | ACS, CCI, SR | D | D | L | D | D | Trach |
| 3 | SG+T | L, T-t, PCTR | T-t | De | |||||
| 4 | T-upper | L, T-t | D | T-t | De | ||||
| 2 | T-mid | L, T-t | TS | D | L, D | D | Trach | L | Trach |
| 2 | T-mid | L, T-t | T-t | D | D | De | |||
| 3 | T-lower | L, T-t | D | T-t | D | Trach (No follow up) | |||
| 3 | T-lower | L, T-t | L | L | De | ||||
Table 4: Site-wise multiple surgical interventions until eventual outcome.
Discussion
The uniqueness of pediatric laryngotracheal anatomy makes laryngotracheal stenosis, a surgical challenge. The intricate mucosal integrity within the cartilage framework makes reconstitution of the airway lumen quite difficult, as every attempt at restoring it surgically may lead to further narrowing due to inflammatory reaction which heals by further fibrosis and cicatrisation. The main problem in pathophysiology in this entity is that we are fighting against nature which heals all insults with scarring leading to stenosis [1,2].
Laryngotracheal stenosis has been a challenging problem to manage with numerous surgical procedures devised to treat this condition, which clearly reflects the lack of a standardized surgical approach which could solve this problem. It has for long been the aim of otolaryngologists around the world, to device an ideal modality of treatment but till date no single treatment of choice has come into vogue [5,6]. Repeated endoscopic dilatations and endoscopic removal of scar or granulations often provide only temporary relief with subsequent restenosis, especially in a tender airway as in children. Medical treatment with intra-lesional steroids, mitomycin-C and immunomodulatory drugs have been tried with some success especially in cases with severe restenosis [3].
The choice of surgical procedure depends upon the age & general condition of the patient, in addition to the aetiology, site & nature of stenosis [1,5,6]. Open surgical techniques like laryngotracheal reconstruction with swissroll insertion or laryngeal stenting, provide a better option than conventional endoscopic dilatations for subglottic stenosis in children. The advantage of the swiss-roll is that it is custommade by meticulous calibration of the stenotic segment to snuggly fit into the pediatric airway after laser dilatation. This customized approach offers better results and avoids re-stenosis [4].
Earlier external surgical approaches like cartilage excision and auto-grafting or end to end anastomosis have more often ended up with complications of restenosis & granulations at the site of surgery. 8 Endoscopic laser dilatation has proved much safer in such cases due to less trauma to laryngeal mucosa and subsequent healing without fibrosis. Recent literature favours the use of laser for endoscopic dilatation with intraluminal stenting as a single stage procedure of choice for a large variety of stenosis [3,4]. KTP/532 Laser has proved to be the ideal laser for excising stenotic segments with high precision, effective coagulability & minimal collateral tissue damage. It can be delivered through hand held devices, micromanipulators or rigid and flexible endoscopes providing easy access to the sites of stenosis [3]. Combined procedures are the standard of care today and they are performed by laserizing the stenotic segment endoscopically followed by external approach for widening the stenotic segment using indwelling stents and by using costal cartilage grafts, which is secured to the airway along with the soft tissues in the neck, thereby integrating securely into the laryngotracheal framework [4].
Stents are either of temporary or permanent types. Temporary laryngotracheal stents are made of various biomaterials like silastic, silicone, polyvinyl chloride, glass polymers or bioceramics [3,5]. The most popularly used one is the Montgomery’s silastic T-tube ideal in cases with long stenotic segments involving the subglottis upto mid trachea. Specialized solid stents like the Hood’s laryngeal stent or Dumon’s silicone stent have added advantages like unique shape with flanges for support, but have not been widely used in our practice [4]. Temporary stents like silastic swissrolls are usually left insitu for six to eight weeks and silastic T-tubes left from six months to one year with frequent re-assessment of airway prior to decannulation. Silastic swissrolls have been successful as stents due to their bio-inert property causing no local inflammation and easy malleability which makes them best suited for each individual airway. These are best indicated for subglottic stenosis in children and they are placed insitu and anchored externally to the neck by buttons, above the tracheostomy [4]. If there is extensive irrepairable scarring inspite of above interventions to this region, then the further option would be to proceed with an posterior cricotracheal resection as an external approach which may help solve the problem [7,8].
Permanent stenting is indicated in short segment/annular and multiple stenosis of the trachea wherein no decannulation is required. Self expanding metal stents like Ultraflex or Gianturco are made of a cylindrical mesh of single stranded nitinol, which has the dynamic radially expanding property called the ‘Marmen effect’. These have great advantage over other stents, as these promote mucosal ingrowth, allow muco-ciliary clearance and provide maximum lumen patency. This has not been tried in the growing airway as in children due to the risk of migration and in the Indian clinical scenario, the deterrent for use among adults for long has been their cost factor [4,6].
Hallmarks in the successful management of PLTS lies in the meticulous evaluation of the patient’s airway, a carefully performed surgery, proper selection of stent and its appropriate intra-luminal placement. Long-term follow-up with regular endoscopic airway assessment remains paramount in order to procure the best results [4]. To effectively decannulate a child and allow it to breathe and speak like a normal peer individual, will the best dream to foresee for any paediatric airway team.
Conclusion
This retrospective study has shown that pediatric laryngotracheal stenosis can be ideally managed by endoscopic laser dilatation with intraluminal stenting. Laryngeal stents like silastic swissrolls and tracheal T-tubes have been efficient in the treatment of subglottic and upper tracheal stenosis. Endoscopic laser dilatation and stenting technique has provided better results in contrast to the earlier external reconstruction procedures which had high morbidity rates and required prolonged hospitalization. Early decannulation with preservation of adequate airway and good phonatory function were achieved by this technique in most of our children. Restenosis and extensive granulations were successfully managed carefully by revision laser dilatation and restenting with subsequent decannulation over time.
Our study also highlights translaryngeal intubation as the leading cause for pediatric laryngotracheal stenosis in our practice. Hence, it is vital to emphasise the use of atraumatic intubation techniques by personnel in OTs/ICUs with high volume, low pressure cuffs in order to prevent inadvertent laryngotracheal injury. The future lies in the development of dynamic, cost-effective, drug-eluting intraluminal stents with anti-microbial and biodegradable properties, which would provide the ideal solution to treat this extremely difficult entity.
Ethical Considerations
None.
Conflict of Interest
Nil.
Financial Disclosure
Nil.
References
- Stern Y, Cotton RT (1999) Evaluation of the noisy infant. In: Cotton RT, Myer III CM (Eds) Practical pediatric otolaryngology. (1st edn), Lippincott-Raven, Philadelphia, New York, USA. pp. 471–476.
- Kryger M, Bode F, Antic R, Anthonisen N (1976) Diagnosis of obstruction of the upper and central airways. Am J Med 61: 85–93.
- Monnier P, George M, Monod ML, Lang F (2005) The role of the CO2 laser in the management of laryngotracheal stenosis: a survey of 100 cases. Eur Arch Otorhinolaryngol 262: 602–608.
- Shekar A, Natarajan K, Raghunandhan S, Kameswaran M, Murali S, et al. (2012) Outcomes in the management of pediatric laryngotracheal stenosis: Our experience. Int J Phonosurg Laryngol 2: 14-19.
- Wiet GJ, Long FR, Shiels IW, Rudman DT (2000) Advances in pediatric airway radiology. Otolaryngol Clin North Am 33: 15–28.
- Cotton R (1978) Management of subglottic stenosis in infancy and childhood: A review of a consecutive series of cases managed by surgical reconstruction. Ann Otol Rhinol Laryngol 87: 649–657.
- Cotton RT, Evans JN (1981) Laryngotracheal reconstruction in children. A five-year follow-up. Ann Otol Rhinol Laryngol 90: 516–520.
- Monnier P, Lang F, Savary M (2003) Partial cricotracheal resection for pediatric subglottic stenosis: ?A single institution’s experience in 60 cases. Eur Arch Otorhinolaryngol 260: 295–297.
Citation: Devarasetty A, Raghu Nandhan S, Rathnaraajan S, Vijaya Krishnan P, Kameswaran M (2019) Surgery for Paediatric Laryngotracheal Stenosis: A South Indian Experience. Otolaryngol (Sunnyvale) 9: 373. DOI: 10.4172/2161-119X.1000373
Copyright: © 2019 Devarasetty A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4033
- [From(publication date): 0-2019 - Nov 29, 2025]
- Breakdown by view type
- HTML page views: 3099
- PDF downloads: 934