Survival Rates of HIV Patients on Antiretroviral Therapy in the Kumba Health District: A Six-Year Retrospective Cohort Study from 2008 To 2013
Received: 15-Sep-2020 / Accepted Date: 14-Oct-2020 / Published Date: 21-Oct-2020 DOI: 10.4172/2161-1165.1000391
Abstract
Anti-Retroviral Therapy (ART) has clearly been shown to be effective in reducing mortality amongst those who remain on treatment and adhere to therapy. Recently, in developing countries where the burden of HIV/AIDS is high, ART has become more available. The outcome of patients with HIV/AIDS has improved dramatically since 1996 for those who have access to the appropriate treatment. This study was carried out to determine the survival rates of HIV/AIDS patients on antiretroviral therapy in the Kumba Health District. A six –year retrospective cohort study involving collection of point of care data from 2008 to 2013 was carried out to assess the survival rate of HIV patients on treatment in the HIV/AIDS treatment centers in the Kumba Health District. The study was carried out in two phases. Phase one assessed the quality of data and phase two involved collection of data from the ARV registers. It was found that the Kumba Health District place a total of 5421 (1524 males, 3897 females) on ARV treatment. An overall data quality score of 72.4% was observed. The overall loss to follow up rate was 18.19%, males having higher loss to follow up rate (27.62%) compared to females (13.99%). Females had a higher five-year survival rate (76.64%) compared to males (65.6%). The five year survival rate was highest in the age-group 31-45 years (77.0%) and least in the age group 0-15 years (47.1%). It was observed that 73.23% of the patients survived five years after initiation into treatment. Earlier initiation on ART through expanded testing and counselling should be encouraged in HIV-infected patients in order to increase the survival rate.
Keywords: Antiretroviral Therapy; HIV; Survival rate; Kumba; Cameroon
Introduction
HIV is a virus that belongs to a sub group of retroviruses known as the lentiviruses (or slow viruses). The virus was first recognized in the early 1980s and has since become a major pandemic [1]. In 1990, there were fewer than 32,000 HIV-positive Cameroonians. By 1995, the number of PLWHA increased more than eight times to 264,000. According to the national AIDS control committee, there will be about 726,000 PLWHA in 2020 [2]. The National AIDS Control Committee/ Central Technical Group (CNLS/GTC) estimates that there are 141 new HIV infections per day in Cameroon, which means six (6) newly infected persons each hour, every day [3]. In 2010, there was an estimated 560,000 Cameroonians living with HIV. Cameroon has more people living with HIV (PLWHA) than other central African countries.
With the advent of free antiretroviral drugs (ARV) in Cameroon, HIV infected persons get access to ARV for the management of the infection. Information about the survival rates of these patients on ARV is very necessary in order to better appreciate the outcome of the patients on ARV therapy. However, lack of good quality and reliable data has been a major obstacle to the assessment of health outcomes in many countries [4]. The availability of antiretroviral treatment (ART) decreases the number of AIDS-related deaths and allows people with HIV to live healthy lives. Access to treatment has continued to expand. Cameroon has more than 150 clinics that provide ART, and since 2007, ARV drugs are free to those who need them. In 2000, more than 50,000 Cameroonians were in need of ART but had no access to it. By 2005, 16,500 of the 86,000 people eligible for treatment had access. In 2010, ART coverage was projected to reach 41% of PLWHA needing treatment. By 2020, program managers plan to provide coverage to more than 80% of the people ages 15 and older who need ART [5]. This component of the national response will require substantial human and financial resources. Preventing new infections would reduce the number of people needing treatment and decrease the resources required for ART into the future. HIV patients are being initiated into ART every month of each year in the Health District but the survival experience of these patients is not documented. It was therefore very important to determine the survival rates of these patients on ARV to have a better understanding of their survival pattern in order to provide valid health data and information required by the health system for the better management of HIV patients.
Materials and Methods
Study site
The Kumba Health District (KHD) is the largest Health District in the South West region with a total population of 258.606 inhabitants as of 2013. This represents about 1/5 of the regional population (Meme Monthly Report, 2013).
Study design
A retrospective cohort study was conducted involving the collection of point of care data. The study was carried out in two phases (phase 1 and phase 2). Phase 1 involved assessing the quality of data in all the treatment centres to see if they were of good quality to suite the study. Centres having overall data quality score above 50% were selected for data collection. Phase 2 involved collections of data from ARV registers and monthly report forms to the South West Regional Technical Group for HIV/AIDS (SWRTG) using the adjusted Global Burden of Disease (GBD) check list. Information about all HIV positive persons who were diagnosed positive and placed on treatment from 2008 to 2013 was gotten from the ARV registers. This information included the annual number of people initiated on ARV stratified by age and sex, the annual number of deaths stratified by age and gender, the total number of withdrawals and the start CD4 cell count of the patients. This information was used to generate mortality and survival rates.
Ethical considerations
Ethical approval was gotten from the Faculty of Health Science- Institutional Review Board (FHS-IRB) of the University of Buea. Also administrative authorization was gotten from the South West Regional Delegation of Public Health and from the District Health Service Kumba. Data collected was treated with strict confidentiality through the use of patient codes only.
Sampling
The study was carried out in two phases. Phase one was carried out to assess the quality of data at each treatment centre in the Kumba Health District. This was done using a check list. A 50% overall data quality was set as the threshold for any treatment centre to be included in the second phase. Based on the obtained results data were then collected from the treatment centres. The study duration was six (6) months, starting from March to August 2014.
The Kumba Health District has 3 HIV treatment centre (UPEC units). These centres are: The UPEC unit of the Kumba District Hospital. The UPEC unit of the Presbyterian General Hospital Kumba and The UPEC unit of the Apostolic Health Centre, Banga-Bakundu. Data was collected from the HIV registers of these treatment centres and also from the monthly report forms of the SW RTG of these treatment units.
Data from the HIV clinic pre-ART and ART registers was used. The registers were designed by the National AIDS Control Committee (NACC) for the standardized collection and reporting of data. From pre-ART and ART registers, the numbers of patients ever enrolled in care from 2008 to 2013 were counted, the number initiated on ART and, their dates of ART initiation, the deaths that were recorded per year and the total number of withdrawals. The medical records were designed by the hospital and were stored in the clinic’s records office by year of recruitment, by codes and by patient outcome.
Each person with a unique identification code in the register was followed for the period of time in which the person was alive. That is, a person enrolled in 2008 with a unique identification number was followed from 2008 to 2013. To get the number of deaths per year, when patients were initiated with their specific codes, deaths recorded for a particular year were those that occurred from patients initiated that year. A person was considered to have withdrawn within a specific year if there was no contact 90 days after the last missed appointment of ARV refill. For life table calculation each patient for each specific year was followed over the calendar years till death occurs. All the data from ARV registers and monthly report forms to the SWRTG for HIV/ AIDS were used to calculate the mortality and survival indicators were calculated.
Data analysis
The collected data was stratified by years. For data quality assessment, four of the six core data quality dimensions proposed by DAMA UK Working Group on “Data Quality Dimensions” (availability/ consistency, timeliness and completeness) were used. The data were entered into Microsoft Excel 2010. Calculations of mortality and survival rates were done using SPSS version 20. Information from the check list was used to bring out Mortality and Survival rates. Chisquare test was used to compare the death rate and case fatality rates among groups at 5% significance level.
Results
Data quality
Table 1 shows the summary results of the data quality assessment for the first phase of the study. The overall quality of data in the health district was rated at 72.4% with the Kumba District Hospital ranked top (99.3%) and the Apostolic Health Centre, Banga-Bakundu the least (58.7%).
| Data Quality Assessment Summary (2008-2013) | |||||||||
|---|---|---|---|---|---|---|---|---|---|
| Completeness | Availability | Consistency | Update Status | Data Quality | |||||
| Treatment Center | No. complete | Expected N (%) | % | Available | Expected | % | % consistency across sources | % updated ARV registers | Overall quality % |
| PGHK | 51 | 72(70.8) | 70.8 | 44 | 72 | 70.9 | 61.9 | 33.3 | 59.2 |
| KDH | 72 | 72 | 100 | 72 | 72 | 100 | 97.3 | 100 | 99.3 |
| AHCBB | 43 | 72 | 59.7 | 48 | 72 | 66.7 | 75.2 | 33.3 | 58.7 |
| TOTAL | 166 | 216 | 76.83 | 164 | 216 | 80.6 | 78 | 53.53 | 72.4 |
PGHK=Presbyterian General HospitalKumba, AHCBB= Apostolic Health Center Banga-Bakundu, KDH= Kumba District Hospital.
Table 1: Data quality assessment summary.
The data quality assessments at each treatment centres per year are presented in Table 2. It was observed that scores for the attribute for ARV register update were very low (below 50%) for the PGHK and the AHCBB compared to the KDH.
| Data Quality Assessment Summary | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Completeness | availability | Consistency | Update Status | Overall Data Quality | ||||||
| Treatment Center | Year | No. complete | Expected | % | Available | Expected | % | % consistency across sources | % updated ARV register | Overall quality |
| PGHK | 2008 | 0 | 12 | 0 | 1 | 12 | 50 | 82 | 100 | 58 |
| 2009 | 6 | 12 | 50 | 10 | 12 | 83.3 | 70 | 100 | 75.8 | |
| 2010 | 12 | 12 | 100 | 9 | 12 | 75 | 72 | 0 | 61.8 | |
| 2011 | 12 | 12 | 100 | 7 | 12 | 58.3 | 71 | 0 | 57.3 | |
| 2012 | 12 | 12 | 100 | 8 | 12 | 66.7 | 51 | 0 | 54.4 | |
| 2013 | 9 | 12 | 75 | 9 | 12 | 75 | 41 | 0 | 47.8 | |
| % | 51 | 72 | 70.8 | 44 | 72 | 70.9 | 61.9 | 33.3 | 59.2 | |
| KDH | 2008 | 12 | 12 | 100 | 12 | 12 | 100 | 97 | 100 | 99.0 |
| 2009 | 12 | 12 | 100 | 12 | 12 | 100 | 98 | 100 | 99.5 | |
| 2010 | 12 | 12 | 100 | 12 | 12 | 100 | 100 | 100 | 100 | |
| 2011 | 12 | 12 | 100 | 12 | 12 | 100 | 89 | 100 | 97.3 | |
| 2012 | 12 | 12 | 100 | 12 | 12 | 100 | 100 | 100 | 100 | |
| 2013 | 12 | 12 | 100 | 12 | 12 | 100 | 100 | 100 | 100 | |
| % | 72 | 72 | 100 | 72 | 72 | 100 | 97.3 | 100 | 99.3 | |
| AHCBB | 2008 | 7 | 12 | 58.3 | 9 | 12 | 75 | 91 | 0 | 56.1 |
| 2009 | 9 | 12 | 75 | 6 | 12 | 50 | 80 | 0 | 51.3 | |
| 2010 | 8 | 12 | 66.7 | 9 | 12 | 75 | 67 | 100 | 77.2 | |
| 2011 | 6 | 12 | 50 | 7 | 12 | 58.3 | 50 | 100 | 64.6 | |
| 2012 | 3 | 12 | 25 | 10 | 12 | 83.3 | 72 | 0 | 45.1 | |
| 2013 | 10 | 12 | 83.3 | 7 | 12 | 58.3 | 9 | 0 | 58.2 | |
| % | 43 | 72 | 59.7 | 48 | 72 | 66.7 | 75.2 | 33.3 | 58.7 | |
Table 2: Annual data quality assessment per treatment centres.
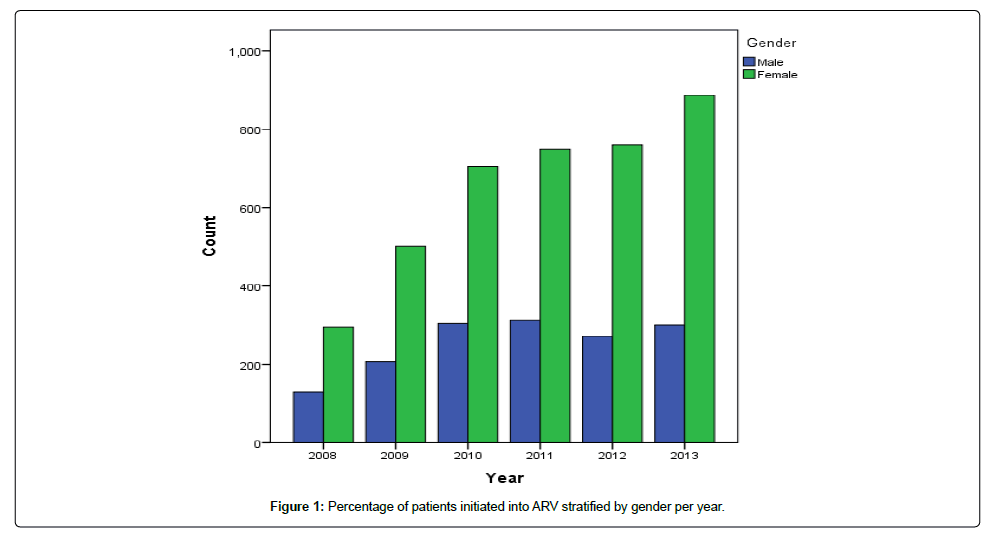
Annual number of persons enrolled stratified by gender
It was observed that females were initiated more on treatment than the males as shown in Figure 1. Across the years the total number of females placed on treatment was twice the number of males.
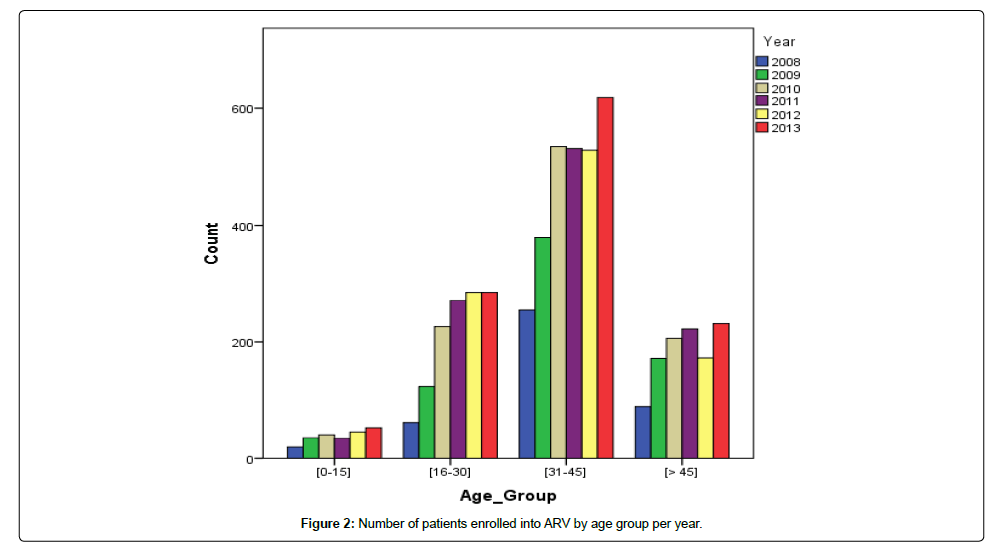
Annual number of HIV patients enrolled into treatment by age group.
The ages of the patients placed on treatment in the Health District ranged from1-99 years. These ages were grouped into 4 major groups.
The highest percentage of patients on treatment was in the agegroup 31-45 years and the least was in the age group 0-15 years. The number of patients placed on treatment in each group increased across the years as seen in Figure 2.
The five-year survival rate
This is the percentage of patients who are alive 5 years after treatment begins. There were 396 patients enrolled into treatment in 2008 and by the end of 2013, 290 of these patients were alive as shown in Table 3.
| Anniversary of the year of treatment. | Number alive in interval | Number of death | Number remaining at the end of the interval |
|---|---|---|---|
| 1(2008-2009) | 396 | 51 | 345 |
| 2(2009-2010) | 345 | 19 | 326 |
| 3(2010-2011) | 326 | 21 | 305 |
| 4(2011-2012) | 305 | 6 | 299 |
| 5(2012-2013) | 299 | 09 | 290 |
Table 3: Follow up of patients initiated in 2008 in the Kumba District Hospital.
Calculation of the five year survival rate gave 73.23%
Five year survival rate= 290/396*100=73.23%
The five-year survival rate by gender
122 male and 274 female patients were enrolled into treatment in 2008 and at the end of 2013, 80 males and 210 females were left as shown in Table 4.
| Anniversary of the year of treatment. | Number alive in interval | Number of death | Number remaining at the end of the interval | |||
|---|---|---|---|---|---|---|
| M | F | M | F | M | F | |
| 1(2008-2009) | 122 | 274 | 25 | 26 | 97 | 248 |
| 2(2009-2010) | 97 | 248 | 08 | 11 | 89 | 237 |
| 3(2010-2011) | 89 | 237 | 04 | 17 | 85 | 220 |
| 4(2011-2012) | 85 | 220 | 02 | 4 | 83 | 216 |
| 5(2012-2013) | 83 | 216 | 03 | 6 | 80 | 210 |
M=Males F=Females
Table 4: Follow up of patients initiated in 2008 stratified by gender in the KDH.
Calculating the five-year survival rate per gender it was observed that females (76.64%) had a higher five year survival than males (65.6%).
Five year male survival rate =65.6%
Five year female survival rate = 76.64%
The five-year survival rate by age-group
In the year 2008 17 patients were initiated in the age group 0-15 years, 59 patients in the age-group 16-30 years, 235 in the age group 31-45 and 85 patients in the age group >45 years. By the end of 2013, 8 patients were left in the age group 0-15 years, 42 patients in the agegroup 16-30 years, 181 patients in the age group 31-45 and 59 patients in the age group >45 years.
Calculating the five year survival rate by age-group, it was observed that the age-group 0-15 had the lowest five year survival rate (47.1%) and the age-group 31-45 had the highest five year survival rate (77%).
Five-year survival rates:
0-15 years=47.1%
31-45 years=77%
16-30 years=71.2%
>45 years= 69.4%
Observed survival
Due to the incompleteness of the data in Presbyterian General Hospital and the Apostolic Health Center Banga-Bakundu, only data from the Kumba District Hospital was used as shown in Table 6.
| Year | Age-group / years | No. alive in the interval | No. deaths | No. remaining at end of interval |
|---|---|---|---|---|
| 1(2008-2009) | 0-15 | 17 | 2 | 15 |
| 16-30 | 59 | 7 | 52 | |
| 31-45 | 235 | 29 | 206 | |
| >45 | 85 | 13 | 72 | |
| 2(2009-2010) | 0-15 | 15 | 3 | 12 |
| 16-30 | 52 | 6 | 46 | |
| 31-45 | 206 | 08 | 198 | |
| >45 | 72 | 2 | 70 | |
| 3(2010-2011) | 0-15 | 12 | 1 | 11 |
| 16-30 | 46 | 2 | 44 | |
| 31-45 | 198 | 10 | 188 | |
| >45 | 70 | 8 | 62 | |
| 4(2011-2012) | 0-15 | 11 | 1 | 10 |
| 16-30 | 44 | 1 | 43 | |
| 31-45 | 188 | 3 | 185 | |
| >45 | 62 | 1 | 61 | |
| 5(2012-2013) | 0-15 | 10 | 2 | 08 |
| 16-30 | 43 | 1 | 42 | |
| 31-45 | 185 | 4 | 181 | |
| >45 | 61 | 2 | 59 |
Table 5: Follow up of patients initiated in 2008 stratified by age-group in the KDH.
| Interval since beginning treatment | Alive at beginning of treatment | Died during Interval | Withdraw during interval | Effective number exposed to risk of dying during interval | Proportion who died during interval | Proportion who did not die during interval | Cumulative proportion who survived from enrollment to end of interval |
|---|---|---|---|---|---|---|---|
| 1st year | 396 | 51 | 96 | 376 | 0.136 | 0.864 | 0.864 |
| 2nd year | 373 | 19 | 62 | 342 | 0.056 | 0.944 | 0.816 |
| 3rd year | 354 | 21 | 26 | 341 | 0.062 | 0.938 | 0.765 |
| 4th year | 333 | 6 | 39 | 313 | 0.019 | 0.981 | 0.751 |
| 5th year | 327 | 09 | 31 | 311 | 0.029 | 0.71 | 0.533 |
Table 6: Classical life table of HIV/AIDS on ARV in the Kumba District Hospital.
To generate the classical life table the following assumptions were made: 1-there was no temporal change in the effectiveness of treatment or in survivorship over the calendar time and 2-the survival experience of those who are lost to follow up is the same as the experience of those who are followed up. Following these assumptions, a classical life table was generated as shown in table 6. The survival of these patients increased from the first year to the fourth year of treatment then decreased in the fifth year.
From the table above the percentage survival per year was gotten by taking the proportion of patients who did not die during the years as shown in Table 7. It was observed that the proportion of those who survived increased from the first year up to the 4th year of follow up then decreased in the fifth year.
| Year | Proportion of patients who survived from enrolment to end of interval | Percentage survival (%) |
|---|---|---|
| 1(2008-2009) | 0.864 | 86.4 |
| 2(2009-2010) | 0.944 | 94.4 |
| 3(2010-2011) | 0.938 | 93.8 |
| 4(2011-2012) | 0.981 | 98.1 |
| 5(2012-2013) | 0.71 | 71.0 |
Table 7: Percentage survival across the years.
Discussion
The Kumba Health District had an overall data quality score of 72.4% with the Kumba District Hospital (KDH) having the highest (99.3%). This is probably because in the KDH, there exist an internal data quality control team that checks the data in the treatment centre on monthly basis. In the KDH, the ARV registers and monthly report forms are recorded by the head of the HIV/AIDS unit who is specially trained by the NACC, for filling the forms and registers. After he fills the registers and the monthly report forms, the coordinator of the unit then checks if the information is well entered/presented. This makes the data reliable. In the PGHK and AHCBB, the data are managed only by the personnel in charge. Looking at the annual data quality in each treatment centre it could be observed that there was a variation in the data quality across the years (2008 to 2013) in the PGHK and the AHCBB. In the KDH there exists very little variation across the years.
The high number of female initiation in this study is similar to a study carried out by Felix et al. [6] in Rwanda which showed that 70% of those initiated into ARV were women. This is still in line with another study carried out in Thailand by Le Coeur et al, who found out that a higher percentage of women were on ART compared to the men [7]. According to Braitstein et al. women are often more likely than men to be enrolled into treatment because of reproductive and child health clinics [8]. This makes most women of child bearing age to know their status and when positive they are immediately initiated into treatment to prevent mother to child transmission. Most males know their status and get initiated only when they are sick and seek care in the hospital.
The highest percentage of patients initiated was in the age group 31-45years (52.5%) and the lowest percentage in the age group 0-15 years (4.24%). This is probably because those in the age-group 31- 45 years are a very sexually active age group. According to UNAIDS (2011), half of all new infections worldwide occur in young people. Young people are more at risk of HIV because they become sexually active at a young age and often go about without any preventive measures. The loss to follow up rate (18.19%) in this study is higher than the loss to follow up rate (15.3) that was reported by Kelechi et al. but its comparable to a study carried out by Alemu et al. with a loss to follow up rate of 18% [9,10].
Males had a higher loss to follow up rate (27.6%) than females (13.99%). This is comparable to a study carried out by Onoka et al. who reported high loss to follow up rates in males than females [11]. Loss to follow up cases in the Kumba Health District is probably due to the fact that most patients come from far distant places to get drugs, not because they don’t have treatment centres nearer to them but because of stigmatization.
A study in Zimbabwe found that many women felt unable to disclose their sero-status, forcing them to take their ARV in secret and to do so without the support of their partners, affecting the adherence to treatment. A study by Skovdal et al. found that men saw HIV/AIDS as a threat to their manhood and their lack of participation in HIV services, made them at times be lost to follow up [12]. Looking at the survival rates in terms of 5-year survival rate and the life table, it was observed that the survival rate was 73.23%. This implies that out of 100 HIV cases initiated into treatment 73 will survive after five years of treatment. Stratifying the five year survival rate by gender, females had a higher five year survival rate (76.64%) compared to males (65.6%). This was similar to a study carried out by Skovdal et al. in Zimbabwe; men survived less after five-years of start of treatment. The study also reported that men will only come to the treatment centres when they are bedridden and brought in a wheelbarrow. It was also observed that patients in the age-group 31-45 years had the highest five year survival rate compared to patients in the other age-groups, the least five year survival rate was in the age group 0-15 years. This is probably due to the fact that, the age group consist of children who need strong support from the care givers because they cannot take cannot take care of themselves. Looking at the observed survival and the percentage survivorship of the patients across the years, we observed that the percentage of those surviving is increasing. That is more HIV/AIDS patients are surviving for a long period of time (five years from start of treatment).
Conclusions
Based on the results gotten from this study it can be concluded that data in the HIV/AIDS treatment centres in the Kumba Health District are of good quality and available for use. The Kumba District Hospital has the best data with respect to the attributes of data qualities that were used. Most patients on treatment in the Health District are in the agegroup 31-45. Females have a more health seeking behaviour than males in the health district since more females are initiated into treatment than males. The five year survival rate of the health district is 73.23% and females have a higher five year survival rate than males. This study was conducted only in the Kumba Health District; it is recommended that similar studies should be carried out in other health districts in the region and the country at large. The NACC should carry out regular visits to treatment centres/Health Districts to ensure that data entry is in accordance with their guidelines. Information, education and communication on ARV and their side effects should be intensified to avoid defaulting and drop outs from treatment. Each treatment centres should try to establish an internal team for data quality assessment. For easy access of the data in the treatment centres data should be computerized. Voluntary counselling and testing should be expanded as good strategies for the early detection of cases for prompt initiation on ARV.
Competing interests
The authors had no competing interest
Authors’ contributions
Achangwa Chiara initiated the study, and collected the data. Achangwa Chiara and Fomboh Richard did the data analysis and report writing, while Fomboh Richard prepared the manuscript. Both author proofread and corrected the manuscript
Acknowledgements
We thank the District medical officer for the Kumba Health District, Dr. Mbamoulou Achu for allowing this study to be carried out in the Health District and all other forms of advice he provided to me. Sincere appreciation to the staff of the HIV/AIDS treatment centres-Unite de pris en charge des personnel vivant avec le VIH/SIDA (UPEC units) of the Kumba District Hospital, the Presbyterian General Hospital kumba and the Apostolic Health Centre Banga-Bakundu for their collaboration and the information they placed at my disposal.
References
- Marks G, Crepaz N, Senterfitt JW, Janssen RS (2005) Meta-analysis of high-risk sexual behaviors in persons aware and unaware they are infected with HIV in the United States. J Acquir Immune Defic Syndr 39: 446-453.
- National Institute of Statistics, ORC Macro (2011) Cameroon Demographic and Health Survey and Multiple Indicators Cluster Surveys (DHS-MICS). Calverton Maryland USA, NIS and ORC Macro.
- Setel PW, Macfarlane SB, Szretzer A (2007) A scandal of invisibility: making everyone count by counting everyone. Lancet 370: 1569-1577.
- Republic of Cameroon, Ministry of Public Health, CLNS/GTC, Permanent Secretariat and Planning Monitoring and Evaluation Unit. National AIDS control committee. Central technical group. September (2010), pp: 17-18.
- Felix RK, Mirjam IB, Hadassa F, Veronicah M, Anita A, et al. (2012) Patient Enrolment into HIV Care and Treatment within 90 Days of HIV. Plos one 7: e36792.
- Le Coeur S, Collins I, Pannetier J, Lelievre E (2009) Gender and access to HIV testing and antiretroviral treatments in Thailand: Why do women have more and earlier access? Soc Sci Med 69: 846-853.
- Braitstein P, Boulle A, Nash D, Martin W, Dabis F et al. (2008) Gender and the use of antiretroviral treatment in resource-constrained settings: Findings from a Multicenter Collaboration. J Womens Health 17: 47-55.
- Kelechi NE, Lawal CE, Eseigbe G, Chisara CU (2014) Determinants of Mortality among Adult HIV-Infected Patients on Antiretroviral Therapy in a Rural Hospital in Southeastern Nigeria: A 5-Year Cohort Study. AIDS Res Ther 2014: 1-6.
- Alemu WA, Sebastian MS (2010) Determinants of survival in adult HIV patients on antiretroviral therapy in Oromiyaa, Ethiopia. Glob Health Action 3: 539.
- Onoka CA, Uzochukwu BS, Onwujekwe OE (2012) Retention and loss to follow-up in antiretroviral treatment programmes in South East Nigeria. Pathog Glob Health 106: 46-54.
- Skovdal M, Campbell CJ, Madanhire C, Zivia M, Simon G, et al. (2011) Masculinity as a barrier to mens use of HIV services in Zimbabwe. Glob Health 7: 13.
Citation: Chiara A, Richard F, Wickelema AW (2020) Survival Rates of HIV Patients on Antiretroviral Therapy in the Kumba Health District: A Six-Year Retrospective Cohort Study from 2008 To 2013. Epidemiol Sci 10: 391. DOI: 10.4172/2161-1165.1000391
Copyright: © 2020 Chiara A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2613
- [From(publication date): 0-2020 - Dec 09, 2025]
- Breakdown by view type
- HTML page views: 1732
- PDF downloads: 881