Tetanus Presented as Hemiparesis and Facial Dystonia
Received: 11-Dec-2017 / Accepted Date: 29-Dec-2017 / Published Date: 31-Dec-2017 DOI: 10.4172/2314-7326.1000272
Abstract
We report a case of tetanus presenting as the facial dystonia and hemiparesis with complete recovery and video accompanied follow-up. A 78-year-old male, who sustained an abrasion to his right forearm, presented with dysarthria, dysphagia, prominent involuntary painful muscle spasms in the face, blepharospasm, risus sardonicus, trismus (lockjaw), neck muscle rigidity and mild weakness of the distal right upper extremity. The combined treatment of human antitetanus immunoglobulin, tetanus vaccine, penicillin, metronidazole and diazepam were given with no effect. He continued to worsen and due to the risk of the respiratory failure (finally not developed) he was sent to the Intensive Care Unit. The combined treatment was continued, and his symptoms started to improve within 2 weeks. As the muscle rigidity has been improving, the patient developed significant right hemiparesis. The imaging of the brain and cervical spine found no significant pathology. At the follow-up visits the patient presented only slightly impaired dexterity of the right hand that gradually resolved. There are many reports of unusual presentations of tetanus, however, hemiparesis is uncommon, and to our knowledge, only one case was reported in the literature. We highlight the variability of clinical presentation of tetanus, the need to consider tetanus in cases of rapidly evolving muscle spasms following peripheral injuries and provide the guidelines on tetanus prophylaxis.
Keywords: Tetanus; Lockjaw; Dystonia; Hemiparesis; Blepharospasm
Introduction
Tetanus is an infectious disease caused by Clostridium tetani, a gram positive, anaerobic bacillus, which produces spores that occur in the feces of many domestic animals, humans and in soil [1,2]. Once spores enter the body, they germinate and produce tetanus toxin which is internalized into nerves and spreads from the peripheral to the central nervous system by retrograde axonal transport, trans synaptic spread, and additionally by blood and the lymphatic vessels [1]. The toxin exerts its effect by preventing the release of gamma-aminobutyric acid (GABA) and glycine into the synapse and thus causes motor neurons to receive continuous excitatory discharge which result in the motor spasms [1].
Tetanus may occur as a result of a minor trauma and in up to 30% of cases no portal of entry is identified [1]. The disease is preventable and after the introduction of vaccinations its incidence decreased significantly, however, it still poses a significant health threat in the developing countries and still may occur in the developed countries, particularly among the elderly and other inadequately immunized people [1,3]. In 2013, 14 cases were reported in Poland, all of whom were over 60 years old, only 1 received a booster dose of tetanus, 5 received post-exposure prophylaxis, 7 died (50% mortality rate) [4]. The diagnosis of tetanus is clinical, and it is often delayed in areas, where the disease is uncommon [1,2]. Here we report a severe case of tetanus presenting as the facial dystonia and hemiparesis with complete recovery and video presentation at onset and follow-up.
Case Report
A 78-year-old male, with a history of chronic renal disease, hypertension, hypothyroidism and paroxysmal atrial fibrillation, tripped and fell on the sidewalk, sustaining an abrasion to his right forearm. Five days after the accident he developed swallowing problems, followed by prominent involuntary painful muscle spasms in the face, articulation disturbances and weakness of the right upper extremity two days later. He was consulted by his family doctor, who referred him to the neurology outpatient department. The consulting neurologist suspected ulnar nerve injury and referred him to an orthopedic surgeon. Plain X-rays showed no abnormalities and he was then referred to neurological department. On the initial examination, 10 days after the accident, he presented with blepharospasm, risus sardonicus, trismus (lockjaw), dysarthria, dysphagia, neck muscle rigidity and mild weakness of the distal right upper extremity. The computed tomography of the brain was normal.
The clinical diagnosis of tetanus was made, and the patient was sent to the local Hospital for Infectious Diseases. On admission to the hospital the patient was given 6000 IU of human antitetanus immunoglobulin (Igantet) and tetanus vaccine (Tetana). The combined treatment of penicillin, metronidazole and diazepam was given as well. Due to the inflammatory changes at the site of the injury, aerobic and anaerobic cultures were taken. They were positive for methicillinresistant Staphylococcus aureus, Enterobacter kobei and Klebsiella oxytoca , therefore ciprofloxacin was added. The patient continued to worsen and due to the risk of the respiratory failure (finally not developed) he was sent to the Intensive Care Unit at day 18th after the accident. The combined treatment was continued, and his symptoms started to improve within 2 weeks. As the muscle rigidity has been improving, the patient developed significant weakness of the right upper extremity and mild weakness of the right lower extremity and was sent to the rehabilitation hospital. On admission he was wheelchair dependent and his Barthel Index of Activities of Daily Living (BI-ADL) was 8 points. After two months he was discharged home walking unassisted, with residual weakness of the right upper extremity and BI-ADL score of 20 points.
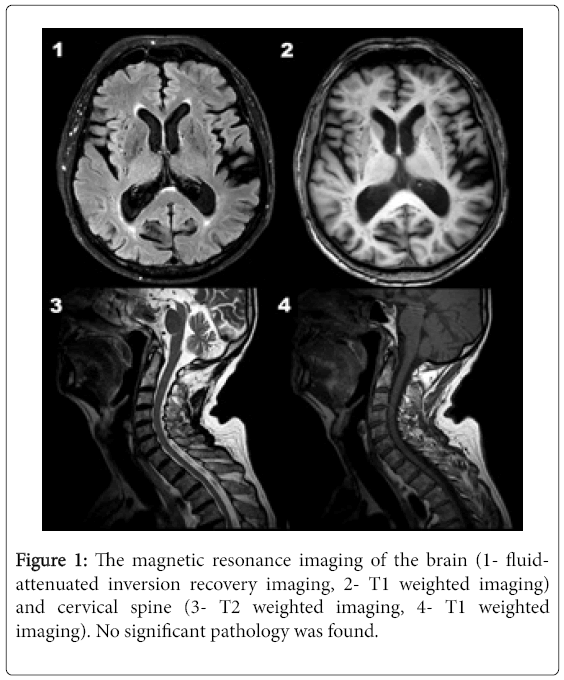
At the successive follow-up visits (10-28 months after the accident) the patient presented only slightly impaired dexterity of the right hand that gradually resolved. Electroneurography demonstrated axonal sensory right ulnar nerve neuropathy, while electromyography and repetitive nerve stimulation were normal. A 3-tesla magnetic resonance imaging of the brain and cervical spine showed no significant pathology (Figure 1).
Discussion
Tetanus may present as generalized (including neonatal) and localized (including cephalic) forms. The spectrum of symptoms is wide and includes rigidity, muscle spasms and dysautonomia that may lead to trismus (lockjaw), risus sardonicus, opisthotonic posturing, dysphagia and respiratory difficulty [1,2,5]. Interestingly, there are many reports of unusual presentations of tetanus including blepharospasm, ptosis, ocular palsies, supranuclear ophtalmoplegia, nystagmus, hemifacial spasm, cranial palsies, camptocormia and spastic paraplegia [6–11]. The pathophysiology underlying muscle paralysis in the course of tetanus is incompletely understood. Clinical and electrophysiological studies confirmed axonal polyneuropathy of “dying back” mode caused by tetanus toxin and was suggested in a series of 34 and 40 patients [12,13]. In a series of 25 patients reversible myopathic changes were found in the acute stage of tetanus [14]. However, hemiparesis is uncommon, and to our knowledge, only one case was reported in the literature. In one of the reports the hemiparesis was attributed to lesions in the cortical and subcortical lesions in the frontal and parietal lobes followed by marked brain atrophy [15]. In our case imaging of the brain and cervical spine detected no lesions that could be responsible for the hemiparesis.
The diagnosis of tetanus is exclusively clinical. The spatula test (positive if severe spasms of the masseter muscles are elicited by touching the posterior pharyngeal wall) was demonstrated to be highly specific (100%) and sensitive (94%) for diagnosis of tetanus. Laboratory tests can demonstrate Clostridium tetani in 30% of patients, however, positive cultures were also found in immune individuals without the disease. Differential diagnosis of tetanus includes strychnine poisoning, orofacial infections, drug-induced acute dystonic reactions, mandibular fractures, progressive encephalomyelitis with rigidity and myoclonus (PERM), hypocalcemic tetany, rabies, Bell’s palsy, stroke, serotonin and neuroleptic malignant syndrome, meningitis, epileptic seizures, psychogenic disorders. Most of the mimics can be discerned by a detailed history (recent injury, even if the presenting symptoms are remote) and physical examination, however, in some cases further investigations are required (e.g. toxicologic testing) [2,16-19].
According to World Health Organization guidelines, in the case of an injury, a dose of tetanus toxoid should be administered if the last dose was given more than 10 years ago or 5 years in the case of severe injuries [3]. Additionally, tetanus antitoxin may be used for prophylaxis in some patients e.g. insufficiently immunized [3].
Conclusion
In summary, tetanus diagnosis has to be considered in cases of rapidly evolving muscle spasms following peripheral injuries. Tetanus prophylaxis guidelines should be widely implemented as this rare complication may be life-threatening.
Ethical Publication Statement
We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Author Contributions
JD, MS, MD, JS worked on the manuscript.
References
- Farrar JJ, Yen LM, Cook T, Fairweather N, Binh N, et al. (2000) Tetanus. J Neurol Neurosurg Psychiatry 69:292–301.
- Ataro P, Mushatt D, Ahsan S (2011) Tetanus: A review. South Med J 104:613–617.
- WHO (2006) Position paper on tetanus vaccines. Wkly Epidemiol Rec20:197–208.
- Zieliński A, Rudowska J (201 5) Tetanus in Poland in 2013. Przegl Epidemiol 69:263–265.
- Cook TM, Protheroe RT, Handel JM (2001) Tetanus: A review of the literature. Br J Anaesth87:477–487
- Muddappa TM, Rao PN (1982) Ocular tetanus. Indian J Ophthalmol 30:163–165.
- Dastur FD, Shahani MT, Dastoor DH, Kohiyar FN, Bharucha EP, et al. (1977) Cephalic tetanus: Demonstration of a dual lesion. J Neurol Neurosurg Psychiatry 40:782–786.
- Seo DH, Cho DK, Kwon HC, Kim TU (2012) A case of cephalic tetanus with unilateral ptosis and facial palsy. Ann Rehabil Med 36:167–170.
- Kaji S, Shibayama H, Sato S, Fukutake T (2014) Acute camptocormia as the presenting symptom of tetanus. J Neurol Neurosurg Psychiatry 85:936–937.
- Saltissi S, Hakin RN, Pearce J (1976) Ophthalmoplegic tetanus. Br Med J 1:437.
- Jain MK, Khanijo SK, Sharma NW (1982) Motor spastic paraplegia and unilateral infranuclear facial palsy complicating tetanus. Br Med J Clin Res Ed 285:477–478.
- Luisto M, Seppäläinen AM (1989) Electroneuromyographic sequelae of tetanus, a controlled study of 40 patients. Electromyogr Clin Neurophysiol29:377–381.
- Shahani M, Dastur FD, Dastoor DH, Mondkar VP, Bharucha EP, et al. (1979) Neuropathy in tetanus. J Neurol Sci 43:173–182.
- Barua AR, Pal NC, Ghose BP (1976) Tetanus myopathy. Indian J Med Res 64:673–679.
- Ijichi T, Yamada T, Yoneda S, Kajita Y, Nakajima K, et al. (2003) Brain lesions in the course of generalised tetanus. J Neurol Neurosurg Psychiatry 74:1432–1434.
- Kipps CM, Fung VSC, Grattan-Smith P, De Moore GM, Morris JGL (2005) Movement disorder emergencies. Mov Disord Off J Mov Disord Soc 20:322–334.
- Srigley JA, Haider S, Johnstone J (2011) A lethal case of generalized tetanus. CMAJ Can Med Assoc J J Assoc Medicale Can 183:1045–1048.
- Wallet F, Didelot A, Delannoy B, Leray V, Guerin C (2014) Severe PERM syndrom mimicking tetanus. Ann Fr Anesth Reanim33:530–532.
- Apte NM, Karnad DR (1995) Short report: The spatula test: A simple bedside test to diagnose tetanus. Am J Trop Med Hyg 53:386–387.
Citation: Dulski J, Schinwelski M, Dubaniewicz M, Slawek J (2017) Tetanus Presented as Hemiparesis and Facial Dystonia. J Neuroinfect Dis 9: 272. DOI: 10.4172/2314-7326.1000272
Copyright: © 2017 Dulski J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution ande reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6369
- [From(publication date): 0-2018 - Nov 26, 2025]
- Breakdown by view type
- HTML page views: 5466
- PDF downloads: 903