The Frequency of Association between Pathologic Subtalar Joint Alignment in Patients with Recalcitrant Plantar Fasciopathy-A Retrospective Radiographic Evaluation
Received: 07-Nov-2018 / Accepted Date: 01-May-2019 / Published Date: 08-May-2019
Abstract
Background: Heel pain associated with a disease process of the medial band of the plantar fascia, Plantar Fasciopathy (PF), is a frequently complaint among patients presenting to foot care specialists. Excessive foot pronation, subtalar joint instability, has been cited as a leading biomechanical factor in the development of PF. The frequency of association between excessive hind foot motion and chronic heel pain has not been studied. The purpose of this retrospective study was to evaluate the occurrence of subtalar joint instability, as evidenced by radiographic angular measurements, in patients diagnosed and surgically treated for recalcitrant PF.
Method: Pre-operative relaxed stance weight bearing radiographs for one-hundred eight patients diagnosed with recalcitrant PF, who had partial or full, of the plantar fasciotomy, were retrospectively and independently reviewed. Subtalar joint instability was measured objectively via the Talar second Metatarsal angle (T2M) on the dorsoplantar radiograph for transverse plane alignment and the Talar Declination angle (TD) on the lateral radiograph for sagittal plane alignment.
Results: 93.52% (101 feet) had at least one angle (T2M or TD) greater than normal accepted values. T2M angles were greater than the normal values 79.63% (86 feet) of the feet examined. With respect to TD angles, 75.93% (82 feet) showed greater than normal values. 17.59% (19) of the feet showed only higher T2M angles, indicating transverse plane dominance, while 13.89% (15 feet) indicated only higher TD angles, indicating sagittal plane dominance. 62.04% (67 feet) had both higher T2M and TD angles.
Conclusion: The data from this study showed a statically significant number of patients with recalcitrant heel pain also exhibited excessive subtalar joint pronation. This could explain the rational for a subset of patients who are unresponsive to typical treatments aimed at healing the diseased fascial tissue, without addressing the co-deformity of subtalar joint instability. Patients who develop recalcitrant PF should be evaluated for subtalar joint instability and options to realign and stabilize the subtalar joint should be incorporated as part of the treatment protocol.
Keywords: Plantar fasciitis; Plantar fasciopathy; Plantar fasciosis; Subtalar joint instability; Hyperpronation; Peri-talar subluxation talotarsal joint displacement
Introduction
Plantar Fasciopathy (PF) is a rather common, painful condition that alters the quality of life of patients. Symptoms are generally most prevalent with the first steps upon waking in the morning and then subside shortly thereafter, only to return after prolonged periods of non-weight bearing. The underlying factors that contribute to the development of PF have been debated and include anatomical, biomechanical, and environmental factors [1]. Knowledge of the contributing factors is important in determining the most effective treatment options to alleviate symptoms and prevent recurrence.
Several studies have claimed that mechanical control of the foot provides the best outcomes [1-6]. This would seem to support the theory that biomechanical factors play a significant role in the development of PF. Abnormal biomechanics, especially excessive subtalar joint pronation, places excessive stress and tension on the medial band of the plantar fascia [7-13]. The plantar fascia is a somewhat rigid band that does not stretch therefore, the end result of these abnormal stresses is localized tissue damage near the origin of insertion into the medial tubercle of the calcaneus. Since this occurs with all weight bearing activities, the healing process is prevented due to repetitive weight bearing activities [14]. This might help explain why athletes and runners seem particularly prone to the development of PF [15,16]. It has been suggested that there is a link between the amount of tension placed on the plantar fascia and the development of plantar fasciopathy [14].
The purpose of this retrospective study is to evaluate the possible magnitude of the difference of subtalar joint stability in PF patients with normal and non-normal levels of subtalar joint alignment. The presence of higher than accepted normal relaxed stance weight bearing Talar-second Metatarsal (T2M) and/or Talar Declination (TD) angles in patients diagnosed with PF can be considered an indication of the underlying abnormal subtalar joint biomechanics. Such evaluation would help emphasize the importance of addressing excessive subtalar joint pronation in addition to amelioration of the associated symptoms of PF.
Patients and Methods
A cohort of 108 patients were considered for this study. These patients represented the number of patients that were diagnosed with recalcitrant PF, unresponsive to conservative treatment for 6 months, by the physicians at the Louis Stokes Cleveland VA Medical Center (Cleveland, OH) who ultimately required plantar fasciotomy, partial or full, within a calendar year. The diagnosis of excessive subtalar joint pronation was determined retrospectively through examination of preoperative relaxed stance weight bearing radiographs. No examinations of the postoperative radiographs were performed. This study received institution review board approval.
Patient selection procedures
A diagnosis code search was performed for a calendar year period of all patients who required surgical intervention due to recalcitrant PF was performed. Patients who received a minimum of 6 months of conservative care were considered. Typical symptoms, such as post-static dyskinesia and pain to palpation of the medial band of the PF, were experienced by all patients. Furthermore, all patients had standard weight bearing radiographs performed to rule out fractures, tumors, or other atypical findings rather than PF. Patients were only included if they had not previously undergone any osseous ankle or foot surgery, as this may influence the radiographic measurements. The radiographs for these selected patients were then evaluated to ensure they met the inclusion criteria.
The patient selection criteria did not explore the number of patients with bilateral PF and the radiographs of the contra-lateral limb were not routinely taken, unless the patient also complained of symptomatology of that limb. This study was concerned only with the foot that required surgical transection of the PF. Finally, only the pre-operative radiographs were used for analysis.
Data collection
The data collected from patients was in the form of dorsoplantar (DP) and lateral view Relaxed Stance weight bearing (RSP) radiographs of the foot/feet presenting with medial heel pain. All patients were radiographed using standard angle and base of gait technique.
Determination of radiographic angles
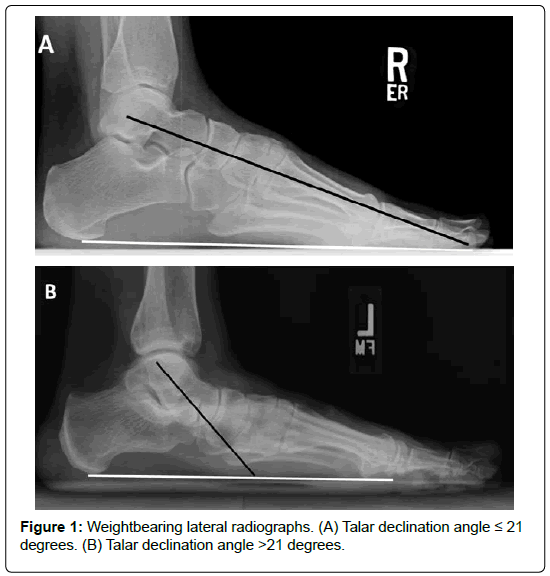
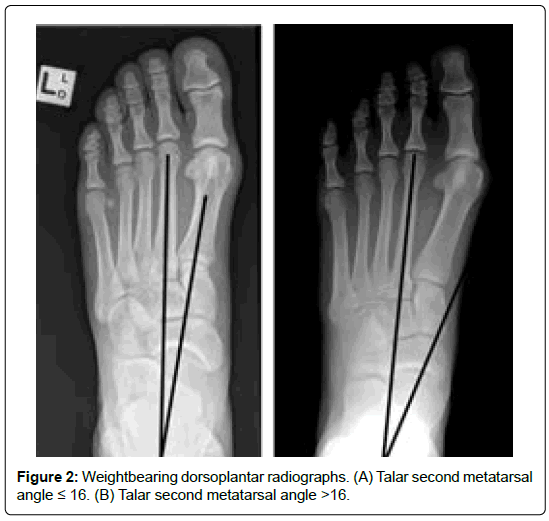
Subtalar joint alignment was objectively assed using the Talar Declination (TD) angle (sagittal plane) and Talar-Second Metatarsal (T2M) angle (transverse plane) [17-22] (Figures 1 and 2). The DP T2M angle has been considered a reliable measurement to evaluate the osseous alignment between the forefoot and the hind foot [17]. The T2M angle is measured between the longitudinal bisection of the second metatarsal and the talus [18]. The second metatarsal is a more reliable reference point over the first metatarsal since many patients can also present with a deviated first metatarsal bone, i.e. increased first intermetatarsal angle. Thomas et al. reported T2M angular values in normal populations as 16° in the bipedal stance position [23].
The TD angle can be used as a direct measure of the inclination of the talus with respect to the ground surface. During pronation, the head and neck of the talus undergo plantar flexion leading to an increase in the TD angle values, while during supination; they undergo dorsiflexion leading to a decrease in the TD values. Thus, pathologic TD values would indicate the occurrence of abnormal subtalar joint alignment. The TD angle can be measured between the longitudinal axis of the talus and the plane of support [23-25]. The accepted normal TD angle is 21° [26,27].
A T2M angle of 16° or less and TD angle of 21° or less were considered normal values and used as the reference to compare the T2M and TD angles measured in the feet of the patients. Both radiographic angles were measured using software that is part of the Vista CPRS system, version 1.0.28.24. These measurements were obtained by a single independent examiner to rule out any bias and to keep a consistency of measurements.
Data analysis
The angles calculated from the radiographs were compared to the normal values (T2M angles higher than 16º and/or TD angles higher than 21º) to determine the existence of excessive subtalar joint pronation.
The percentage of occurrence of values higher than the normal values in at least one view (DP or lateral) was calculated. This result indicates the frequency of presence of subtalar joint instability.
Once a total percentage was calculated, the presence of the deformity was further analyzed with respect to the plane of dominance, if any. Higher values of T2M angles indicate deformity in the transverse plane while higher values of TD angles indicate deformity in the sagittal plane. Transverse plane dominance was identified when the radiographs for a single patient showed a higher than normal T2M angle and a TD angle within the normal range. Alternatively, sagittal plane dominance was identified with only a higher TD angle coupled with a normal T2M angle. Higher T2M and TD angles together indicate deformity in both planes.
Statistical analysis
For each of the angular measurements, TDa and T2Ma, we labeled each angle value as either normal or non-normal, creating two binary variables, TDc and T2Mc. The distributions of angular measurements, TDa and T2Ma, from the 108 radiographs of feet were examined visually and labeled by their normal/non-normal group assignment, TDc and T2Mc. The frequency and relative frequency of patients who had normal and non-normal TD angles were calculated. The frequencies and relative frequencies of patients who had normal TD and T2M angles, only normal TD angles, only normal T2M angles, and both angles non-normal were calculated. Based on the resulting contingency table, a χ2 test of independence between TDc and T2Mc was performed. Summary statistics for the angle measurements in the normal and non-normal TDa and T2Ma groups were calculated. For both the TDa and T2Ma data, the normal and non-normal angle groups were assessed for normality using the Shapiro-Wilk test. Angular measurements between normal and non-normal groups were compared with one- and twosample t-tests and Wilcoxon rank sum tests (equivalent to Mann-Whitney tests) for normally and non-normally distributed data, respectively. For the Wilcoxon rank sum tests, the Hodges-Lehmann estimator and distribution-free confidence interval were found. Statistical analysis was performed in the statistical programming language R v. 3.5.1 [28].
Results
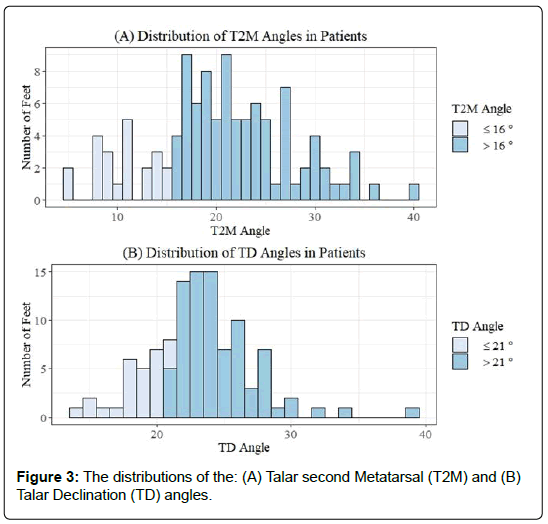
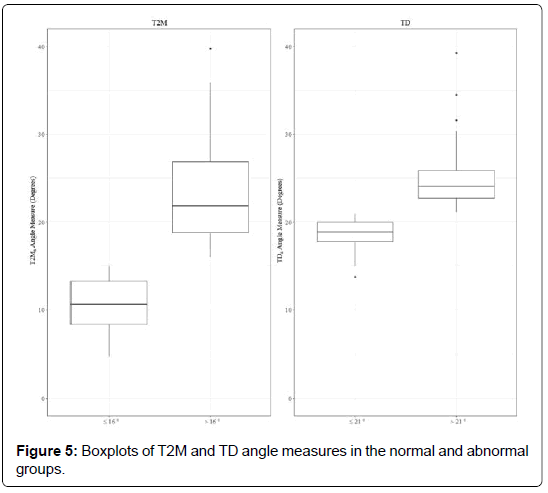
The distributions of the TD and T2M data are provided (Figure 3). Frequencies and relative frequencies are provided (Figure 4). Difference in TD and T2M angles in their respective normal and non-normal groups are summarized (Table 1 and Figure 5). Angle data in the normal (W=0.91, p=0.0325) and non-normal (W=0.84, p<0.001) TD groups were not normally distributed. Angle data in the normal (W=0.95, p=0.36) and non-normal (W=0.93, p=0.0002) T2M groups were normally and non-normally distributed, respectively. Consequently, we used one-and two-sided Wilcoxon rank sum tests (equivalent to Mann-Whitney tests) to evaluate angle differences between groups. The results of the Wilcoxon rank sum, values of the Hodges- Lehmann estimator and corresponding distribution-free confidence interval are provided in Table 2. The categorical variables TD and T2M were independent (χ2=0.91, p=0.34).
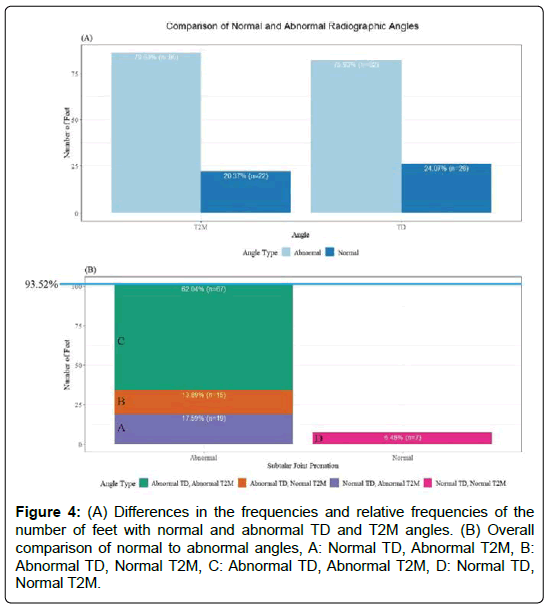
Figure 4: (A) Differences in the frequencies and relative frequencies of the number of feet with normal and abnormal TD and T2M angles. (B) Overall comparison of normal to abnormal angles, A: Normal TD, Abnormal T2M, B: Abnormal TD, Normal T2M, C: Abnormal TD, Abnormal T2M, D: Normal TD, Normal T2M.
| Angle | Type | n | Mean | Median | Standard deviation |
|---|---|---|---|---|---|
| TD | Abnormal | 82 | 24.71 | 24.02 | 3.06 |
| Normal | 26 | 18.54 | 18.84 | 1.91 | |
| T2M | Abnormal | 86 | 23.08 | 21.83 | 5.29 |
| Normal | 22 | 10.52 | 10.57 | 2.97 |
Table 1: Summary statistics for normal and abnormal Talar Declination (TD) and Talar second Metatarsal (T2M) angles.
| Group Comparison | Wilcoxon Rank Sum (Mann-Whitney) Test | W | Difference in location (Hodges-Lehmann estimate) | p-value | 95% Confidence interval |
|---|---|---|---|---|---|
| TD (normal vs. abnormal) | Two-tailed | 0 | -5.55 | 1.91E-14 | (-6.70, -4.53) |
| T2M (normal vs. abnormal) | Two-tailed | 0 | -11.83 | 5.50E-13 | (-13.94, -9.75) |
| TD (normal vs. abnormal) | One-tailed | 0 | -5.55 | 9.54E-15 | (-Inf, -4.68) |
| T2M (normal vs. abnormal) | One-tailed | 0 | -11.83 | 2.75E-13 | (-Inf, -10.08) |
Table 2: Results of the Wilcoxon Rank Sum one- and two-tailed tests.
Planar dominance was analyzed for transverse and sagittal plane. Out of 108 feet, 93.52% (101 feet) had at least one angle (T2M or TD) greater than normal accepted values. T2M angles were greater than the normal values 79.63% (86 feet) of the feet examined. With respect to TD angles, 75.93% (82 feet) showed greater than normal values. 17.59% (19) of the feet showed only higher T2M angles, indicating transverse plane dominance, while 13.89% (15 feet) indicated only higher TD angles, indicating sagittal plane dominance. 62.04% (67 feet) had both higher T2M and TD angles.
Discussion
PF is one of the most common foot and ankle pathologies [29]. It is commonly accepted that repetitive strain on the plantar fascia due to excessive tensile forces at its origin (calcaneal attachment) is the most common cause of this condition [30-32]. Some researchers believe PF is caused by biomechanical overuse from extended standing or running which results in microtears at the calcaneal enthesis [33]. Other research suggests this condition is a result of an underlying mechanical abnormality [8,9,29,34]. However, this is still debated as there has not been any significant evidence to support this conclusion [35].
A normal biomechanical functioning of the foot is dependent on the stability and proper alignment of the talus on the calcaneus and navicular. A loss of talocalcaneal alignment, subtalar joint instability, leads to an excessive amount of foot pronation shown to increase the forces acting onto the medial column of the foot [36,37]. Excessive subtalar joint pronation is characterized by dynamic excessive plantar flexion, eversion and adduction of the talus on the calcaneus when weight bearing. This may lead to excessive eversion of the calcaneus, valgus forefoot and plantar drop of the navicular upon weight bearing [18,27,38]. The clinical result of this partial dislocation of the articular facets during the stance phase of the gait cycle is hyperpronation, which is considered a common foot and ankle disorders [39]. PF is believed to be a common problem associated with excessive hind foot instability [40].
The plantar fascia provides support and stability to the medial longitudinal arch/medial column and assists in the weight bearing activities of the foot [41,42]. During pronation, the weight of the body is transmitted onto the weight bearing surface. This causes the medial longitudinal arch to lower which in turn results in tensile forces acting on the plantar fascia as it resists the lowering of the arch [43-46]. More force will act on the larger medial band that is supporting the dynamic medial column over the smaller lateral band of the plantar fascia that supports the more static lateral column.
Diagnosis of subtalar joint pronation can be accomplished by evaluation of the position of foot components and their motion, i.e. range of motion testing. Unfortunately, this type of measurements is purely subjective and is not very reproducible from one examiner to another. There are several arthrometric measurement techniques accepted for evaluation of foot and ankle pathologies. Radiographic measurement techniques are commonly used in the assessment and diagnosis of osseous foot deformities. The authors selected weight bearing radiographic measures because of the objective findings that are highly reproducible and are backed via validated studies.
In this study, 93.52% of patients with PF had higher than the normal values for the T2M, TD or both angles. Since it has been established that higher than normal weight bearing T2M and TD angles can be used to diagnose excessive talotarsal joint pronation and the patient population in this study showed a predominance of patients with pathologic radiographic measurements, it stands to reason that excessive talotarsal joint pronation may be a contributing factor in the majority of cases of recalcitrant PF.
In this study, 93.52% of patients with PF had higher than the normal values for the T2M, TD or both angles. Since it has been established that higher than normal weight bearing T2M and TD angles can be used to diagnose excessive talotarsal joint pronation and the patient population in this study showed a predominance of patients with pathologic radiographic measurements, it stands to reason that excessive talotarsal joint pronation may be a contributing factor in the majority of cases of recalcitrant PF.
Unfortunately, the use of the term plantar fasciitis has become commonly associated with disease of the origin of the medial band of the plantar fascia. This is a misnomer as the use of “iitis” is an indication of an inflammatory process. This inflammatory origin has been shown not to exist in all patients with recalcitrant PF [47,48]. The focus of PF treatment is aimed at the reduction of the inflammatory process by the use of non-steroid anti-inflammatory medications, ice, shock-wave, and the use of steroid injections into the medial band of the plantar fascia is advocated. Meanwhile, little to no measures are taken to effectively resolve the underlying mechanical over-loading of forces acting on the plantar fascia while the patient is standing, walking, or running caused by subtalar joint instability.
Many practitioners advocate the use of a pre-fabricated arch supports or custom-made orthoses as a conservative non-surgical option. The effectiveness of an arch support, whether it is off-the-self or custom- made, will have a positive influence to decrease the mechanical overloading/strain of the plantar fascia has been examined and shown to have little to no effect [49]. Furthermore, there is no data to suggest an arch support can realign and/or stabilize the subtalar joint. A recent published multi-centered study showed that there was no radiographic realignment of the subtalar joint [50].
When conservative measures have failed to bring relief, the patient is given the option to have a plantar fasciotomy. There are many associated risks and complications with this procedure that are well documented [51-53]. The release of the fascia may pose a risk to arch stability and could lead to further foot pain. Tweed et. al. reported that a total plantar fasciotomy may lead to further loss of stability of medial longitudinal arch and abnormalities in gait, in particular an excessively pronated foot [54]. Gefen found that tension on the arch may exceed the normal average stress by more than 200% after the transection of the plantar fascia [55]. A recent long-term outcome study over a 10-year period led the authors to believe the partial plantar fascia release leads to a “prolonged recovery period and generally poor outcomes…” [56]. Only 60% of patients reported satisfactory results after a plantar fasciotomy in another study by Monteagudo et al. and only 20 of 41 patients (48.8%) were totally satisfied [57]. For these reasons preservation of the plantar fascia should be advocated and methods to realign and stabilize the subtalar joint, while still allowing a normal range of motion, should be considered.
A limitation of this study is the lack of hands-on clinical biomechanical range of motion examination. This data is observational and lacks subjective findings. Radiographic evidence provides better objective data than subjective visual observation of range-of motion testing or a visualization of the gait cycle. Radiographic measurements continue to be the gold standard for the osseous relationship of the complex foot structure. A limitation of weight bearing radiographs is that they do not provide “worse case subtalar joint displacement” that could occur during the gait cycle. This could also be a reason why a subset of patients had normal radiographic values.
This study did not evaluate the calcaneal inclination angle to determine if the patient had a lower, normal, or high arched foot. This was not the intent of this study. It is possible to have a subtalar joint instability in both low and high arched feet, depending calcaneal inclination angle. Finally, this study does not provide any evidence as to how many patients had a co-existing equinus component. Again, that was not the aim of this research; further studies are needed to determine the role of equinus in the formation of recalcitrant PF.
Conclusion
It is clear from our results that, more often than not, recalcitrant PF patients will have non-normal TD and T2M angles, signaling the presence of subtalar joint instability. For this reason, PF treatment coupled with treatments shown to realign and stabilize the subtalar joint could be more successful than PF treatment alone. The reduction of the mechanical overloading of the plantar fascia should assist in the effectiveness of treatment options aimed at “healing” the diseased portion of the fascial tissue. Every effort should be attempted to stabilize the hind foot and preserve the integrity of the plantar fascia, prior to surgical release of the diseased fascial tissue.
Acknowledgments
The authors would like to acknowledge Maria Wojakowski for her assistance with the statically analysis
Availability of Data and Materials
The data that supports the findings of this study is included in the article.
Author Contributions
Conception: MEG; Design of the study: MEG, LK, HK; Analysis and interpretation of data: LK; Literature search: MEG, LK; All authors contributed to the drafting the article and revising it critically for important intellectual content.
Ethics Approval and Consent to Participate
Not applicable.
Consent for Publication
The participants consented to the utilization of their data for the purposes of this scientific study.
Role of the Funding Source
There was no funding for this manuscript.
Competing Interests
The authors declare that they have no competing interests.
References
- Martin J, Hosch JC, Goforth WP, Murff RT, Lynch DM, et al. (2001) Mechanical treatment of plantar fasciitis: A prospective study. J Am Podiatr Med Assoc 91: 55-62.
- Pfeffer G, Bacchetti P, Deland J, Lewis A, Anderson R, et al. (1999) Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot Ankle Int 20: 214-221.
- Campbell J, Inman VT (1974) Treatment of plantar fasciitis and calcaneal spurs with the UC-BL shoe insert. Clin Orthop 103: 57-62.
- Scherer PR (1991) Biomechanics graduate research group for 1988: Heel spur syndrome: Pathomechanics and nonsurgical treatment. J Am Podiatr Med Assoc 81: 68-72.
- O’brien D, Martin W (1985) A retrospective analysis of heel pain. J Am Podiatr Med Assoc 75: 416-418.
- Lynch DM, Goforth WP, Martin JE, Odom RD, Preece CK, et al. (1998) Conservative treatment of plantar fasciitis: A prospective study. J Am Podiatr Med Assoc 88: 375-380.
- Hintermann B, Nigg BM (1998) Pronation biomechanics in runners. Sports Med 26: 169-176.
- Waller J (1978) Physiology of the foot and the biomechanics of the flexible flat foot. Ona J 5: 101-103.
- Warren BL (1984) Anatomical factors associated with predicting plantar fasciitis in long-distance runners. Med Sci Sports Exerc 16: 60-63.
- Kosmahl EM, Kosmahl HE (1987) Painful plantar heel, plantar fasciitis, and calcaneal spur: Etiology and treatment. J Orthop Sports Phys Ther 9: 17-24.
- Mann R, Inman V (1964) Phasic activity of intrinsic muscles of the foot. J Bone Joint Surg Am 46: 469-81.
- Shama SS, Kominsky SJ, Lemont H (1983) Prevalence of non-painful heel spur and its relation to postural foot position. J Am Podiatry Assoc 73: 122-123.
- Schroeder BM (2002) American college of foot and ankle surgeons: Diagnosis and treatment of heel pain. Am Fam Physician 65: 1686-2002.
- Fuller EA (2000) The windlass mechanism of the foot: A mechanical model to explain pathology. J Am Podiatr Med Assoc 90: 35-46.
- Kibler W, Goldberg C, Chandler TJ (1991) Functional biomechanical deficits in running athletes with plantar fasciitis. Am J Sports Med 19: 6671.
- Kwong P, Kay D, Voner RT, White MW (1988) Plantar fasciitis: Mechanics and pathomechanics of treatment. Clin Sports Med 7: 119-126.
- Murley GS, Menz HB, Landorf KB (2009) A protocol for classifying normal- and flat-arched foot posture for research studies using clinical and radiographic measurements. J Foot Ankle Res 2: 22.
- Graham ME, Chikka A, Jones PC (2011) Validation of the talar-second metatarsal angle as a standard measurement for radiographic evaluation. J Am Podiatr Med Assoc 101: 475-483.
- Gould N (1983) Evaluation of hyperpronation and pes planus in adults. Clin Orthop Relat Res 181: 37-45.
- Mosca V (1995) Calcaneal lengthening for valgus deformity of the hind foot results in children who had severe, symptomatic flatfoot and skewfoot J Bone Joint Surg 77: 500-512.
- Myerson MS, Corrigan J, Thompson F, Schon LC (1995) Tendon transfer combined with calcaneal osteotomy for treatment of posterior tibial tendon insufficiency: A radiological investigation. Foot Ankle Int 16: 712-718.
- Sangeorzan BJ, Mosca V, Hansen ST (1993) Effect of calcaneal lengthening on relationships among the hindfoot, midfoot, and forefoot. Foot Ankle 14: 136-141.
- Thomas JL, Kunkel MW, Lopez R, Sparks D (2006) Radiographic values of the adult foot in a standardized population. J Foot Ankle Surg 45: 3-12.
- Gentili A, Masih S, Yao L, Seeger LL (1996) Pictorial review: Foot axes and angles. Br J Radiol 69: 968-974.
- Steel MW, Johnson KA, Dewitz MA, Ilstrup DM (1980) Radiographic measurements of the 526 normal adult foot. Foot And Ankle Int 1: 151-155.
- Digiovanni JE, Smith SD (1976) Normal biomechanics of the adult rearfoot: A radiographic analysis. J Am Podiatry Assoc. 66: 812-824.
- Forg P, Feldman K, Flake E, Green DR (2001) Flake-austin modification of the sta-peg arthroereisis: A retrospective study. J Am Podiatr Med Assoc 91: 394-405.
- Kogler G, Solomonidis SE, Paul JP (1995) In vitro method for quantifying the effectiveness of the longitudinal arch support mechanism of a foot orthosis. Clin Biomech (Bristol, Avon) 10: 245-252.
- Cornwall MW, Mcpoil TG (1999) Plantar fasciitis: Etiology and treatment. J Orthop Sports Phys Ther 29: 756-760.
- Chandler TJ, Kibler WB (1993) A biomechanical approach to the prevention, treatment and rehabilitation of plantar fasciitis. Sports Med 15: 344-352.
- League AC (2008) Current concepts review: Plantar fasciitis. Foot Ankle Int 29: 358-66.
- Goff J, Crawford R (2011) Diagnosis and treatment of plantar fasciitis. Am Fam Physician 84: 676-682.
- Tanner S, Harvey J (1988) How we manage plantar fasciitis. Physician Sportsmed 16: 39.
- Wearing SC, Smeathers JE, Urry SR, Hennig EM, Hills AP (2006) The pathomechanics of plantar fasciitis. Sports Med 36: 585-611.
- Tomaro JE, Burdett RG, Chadran AM (1996) Subtalar joint motion and the relationship to lower extremity overuse injuries. J Am Podiatr Med Assoc 86: 427-432.
- Inman VT (1969) The influence of the foot-ankle complex on the proximal skeletal structures. Artif Limbs 13: 59-65.
- Menz HB (1998) Alternative techniques for the clinical assessment of foot pronation. J Am Podiatr Med Assoc 88: 119-129.
- Vogler H (1981) Arthroereisis principles and concepts. In Clark T (ed.), Year book of podiatric medicine and surgery Mt Kisco, NY pp: 448.
- Stovitz SD, Coetzee JC (2004) Hyperpronation and foot pain: Steps towards pain-free feet. Phys Sports Med 32: 19-26.
- Huang CK, Kitaoka HB, An KN, Chao EY (1993) Biomechanical evaluation of longitudinal arch stability. Foot Ankle 14: 353-357.
- Hicks JH (1954) The mechanics of the foot. The plantar aponeurosis and the arch. J Anat 88: 25-30.
- Wright DG, Rennels DC (1964) A study of the elastic properties of plantar fascia. J Bone Joint Surg Am 46: 482-492.
- Sarrafian SK (1987) Functional characteristics of the foot and plantar aponeurosis under tibiotalar loading. Foot Ankle 8: 4-18.
- Lemont H, Ammirti KM, Usen N (2003) Plantar fasciitis: A degenerative process (fasciosis) without inflammation. J Am Podiatr Med Assoc 93: 234-237.
- Snider MP, Clancy WG, McBeath AA (1983) Plantar fascia release for chronic plantar fasciitis in runners. Am J Sports Med 11: 215-219.
- Sinclair J, Isherwood J, Taylor PJ (2015) The effects of orthotic intervention on multisegment foot kinematics and plantar fascia strain in recreational runners. J Appl Biomech 31: 28-34.
- Steber S, Kolodziej L (2015) Analysis of radiographic outcomes comparing foot orthosis to extra-osseous talotarsal stabilization in the treatment of recurrent talotarsal joint dislocation. J Min Inv Orthop. 1: 1-11.
- Ward ED, Smith KM, Cocheba JR, Patterson PE, Phillips RD (2003) In vivo forces in the plantar fascia during the stance phase of gait. J Am Podiatr Med Assoc 93: 429-442.
- Arangio GA, Chen C, Salathe EP (1998) Effect of varying arch height with and without the plantar fascia on the mechanical properties of the foot. Foot Ankle Int 19: 705-709.
- Cheung JT, An KN, Zhang M (2006) Consequences of partial and total plantar fascia release: A finite element study. Foot Ankle Int 27: 125-132.
- Tweed JL, Barnes MR, Allen MJ, Campbell JA (2009) Biomechanical Consequences of Total Plantar Fasciotomy. J Am Podiatr Med Assoc 99: 422-430.
- Gefen A (2002) Stress analysis of the standing foot following surgical plantar fascia release. J Biomech 35: 629-637.
- Macinnes A, Roberts SC, Kimpton J, Pillai A (2016) Long-term outcome of open plantar fascia release. Foot Ankle Int 37: 17-23.
- Monteagudo M, Maceira E, Garcia-Virto V, Canosra R (2013) Chronic plantar fasciitis: Plantar fasciotomy versus gastrocnemius recession. Int Orthop 37: 1845-1850.
Citation: Graham ME, Kolodziej L, Kimmel HM (2019) The Frequency of Association between Pathologic Subtalar Joint Alignment in Patients with Recalcitrant Plantar Fasciopathy-A Retrospective Radiographic Evaluation. Clin Res Foot Ankle 7: 288.
Copyright: © 2019 Graham ME, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Usage
- Total views: 4081
- [From(publication date): 0-2019 - Dec 18, 2025]
- Breakdown by view type
- HTML page views: 3186
- PDF downloads: 895