The Overcoming of Calcaneal Fractures Associated with Skin Problems through a Minimally Invasive Surgery by Closed Reduction and Percutaneous K-wires Fixation
Received: 02-Jan-2018 / Accepted Date: 12-Jan-2018 / Published Date: 25-Jan-2018 DOI: 10.4172/2329-910X.1000254
Abstract
Introduction: Calcaneus injuries account for 2% of all fractures. The surgical treatment of calcaneal fractures with skin problems is a challenge to the surgeon. Many operative techniques described for management of fractures calcaneus, ranging from minimally invasive percutaneous fixation to extensive open techniques.
Material and methods: Between February 2012 and December 2015, this prospective study included forty five patients (38 male and 7 female) presented with 50 displaced calcaneal fractures associated with skin problems underwent a minimally invasive surgery by closed reduction and percutaneous k-wires fixation.
Results: According to American Orthopedics Foot and Ankle Society (AOFAS) ankle hindfoot scale 37 patients had excellent, 9 patients were good and 4 patients had fair results. According to skin, the bad skin condition improved within 2 to 3 weeks postoperatively and there were no serious skin complications.
Conclusion: Calcaneal fractures associated with bad skin conditions are best treated by a minimally invasive surgery by closed reduction and percutaneous k-wires fixation as there is no delay in surgery time like open procedures and there is a marvelous improvement of skin conditions.
Keywords: Skin problems; Closed reduction; Percutaneous k-wires fixation; Calcaneus fracture
Introduction
The calcaneal fractures account for 2% of all fractures seen in adults. The calcaneus is the most frequently fractured tarsal bone, representing more than 60% of tarsal fractures. Recently the focus of bone healing has shifted from anatomical fixation to biological fixation of all fractures. Specific types of calcaneal fractures such as the tongue type pattern of Essex–Lopressti, the closed reduction and percutaneous fixation in its various forms has been recommended [1]. Recently the results of a multi-centered prospective trial suggested that the differences of management between open reduction and internal fixation (ORIF) and the closed procedures might be less than previously thought [2-5].
Many surgical procedures are described in calcaneal fractures, ranging from minimally invasive and percutaneous fixation to extensile open approaches [6]. The surgical approaches of open reduction of the os calcis may be lateral, medial, or combined approaches, depending on the fracture pattern and the extent of injury [7-9]. Possible complications of open procedures are the disturbance of wound healing, skin necrosis and cutaneous flaps. In addition to posttraumatic arthritis in the lower ankle and adjoining joints, there are reports of osteitis of the os calcis. Severe osteitis of the calcaneus can end with a calcanectomy or amputation of the lower leg [10-14]. The decision of treatment depends on many factors like occupation, age, health comorbidity and associated injuries. In the case of open reduction the time is an important factor in determining surgical outcomes. Ideally, if skin condition is bad the time of surgery should be delayed for 10-14 days after trauma. This delay allows for soft tissue oedema and fracture blisters to resolve completely [15].
We aimed at this study to overcome the bad soft tissue conditions associated with fracture calcaneus and evaluate the results of treatment of os calcis fracture by a minimal invasive surgery by closed reduction and percutaneous k-wires fixation. Also, to compare the clinical and radiological results with open and minimally invasive surgical techniques found in the literature.
Patients and Methods
Between February 2012 and December 2015, 45 patients (38 male and 7 female) had undergone this prospective study. The patients presented by fifty calcaneal fractures associated with skin problems in the form of severe oedema, skin blisters, bullae, degloved skin and contaminated open calcaneal fractures All of them were managed by closed reduction and percutaneous k-wires fixation at Mansoura emergency university hospital. The average age at time of calcaneal fracture was 36.5 years (range 21-60 years) of 45 patients, only 5 were bilateral. The mechanism of trauma was a falling from heights in 38 patients and road traffic accidents in seven patients. Patients examined for additional injuries of the musculoskeletal system. There were 8 patients had multiple injuries, 6 patients had fracture spine, 2 cases were fracture femur and 2 cases were fracture tibial plateau. 36 patients had severe edema with skin blisters all over the ankle and foot, 9 cases had degloved skin and open fracture calcaneus (Figure 1).
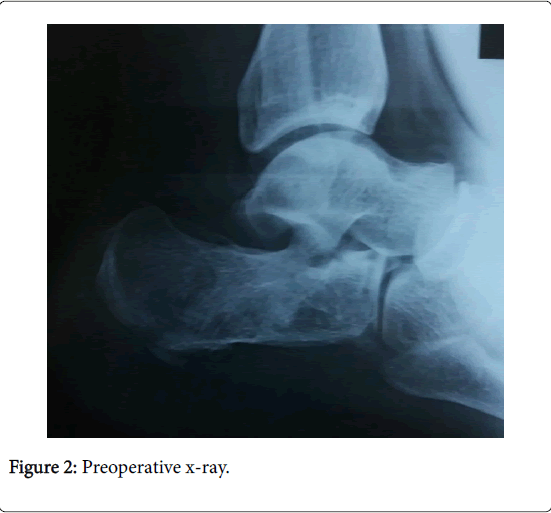
A standard series of plain X-rays of the ankle and foot were taken. The anteroposterior view, the lateral view facilitates the measurement of both Bohler’s and Gissane’s angles and axial view and axial view (Figure 2). CT scanning was performed for all patients for detecting minimally displaced or comminuted fractures. 22 patients had tongue type fracture, 15 cases were joint depression type and 13 patients were comminuted fracture.
Operative Technique
After anesthesia, the patients were positioned in lateral position without a tourniquet. After complete sterilization and draping with the foot and leg left free, the first step was the insertion of a 5-mm Steinmann pin superolateral to the Achilles tendon insertion, the pin was inserted into the articular fragment under image. In the joint depression fracture the pins was placed just posterior to the talus from postero-superior to antero-inferior direction and manipulate the fragment to restore the posterior facet as described by Essex-Lopresti [1].
Another pin inserted into the body of the calcaneus then closed reduction of the fracture was done and the varus or valgus malaligment of the hind foot was corrected. Compression of the heel applied both medially and laterally to reduce the main medial and lateral fragments, this reduces the calcaneal width and prevents lateral impingement. The reduction of the calcaneus was verified by examining the lateral radiographic and axial views. In the case of joint depression fractures, the qualities of joint reduction improved using small stab wound incision and use a blunt which provides a direct elevation and reduction of the articular fragment. The reduction of the posterior facet was secured by two 2 mm k-wires parallel to subarticular joint, then insert 2 k-wires from the body of the calcaneus to the articular fragment from inferior to superior direction. Finally 2 k-wires were inserted parallel to inferior cortex of the calcaneus untill calcaneocuboid joint to keep the length and maintain the varus and vulgus alignment. Another k-wire from lateral to medial if there is fracture sustentaculum talii.
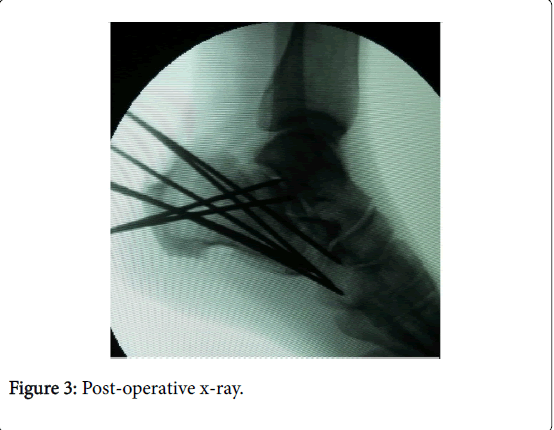
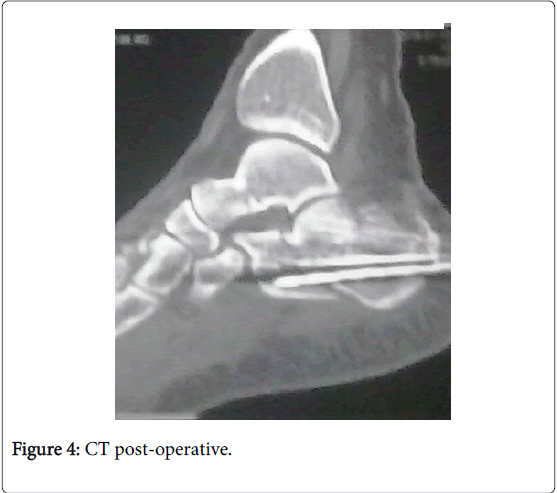
The number of k-wires is usually 6 k-wires but may vary according to the type of fracture and the degree of comminution. k-wires should secure both the reduced articular surface and the overall alignment and should be arranged perpendicular to fracture lines as possible. After introducing the k-wires, the wires were cut and bent outside the skin level and the Steinmann pins were removed. A bulky sterile dressing was applied. Anti oedematous measures were prescribed and elevation of the limp. Active range of motions exercises encouraged. The patients underwent closed follow up for care and evaluation of the skin condition and post-operative plain x-rays and CT scan were done (Figures 3 and 4).
Follow-up every 2 weeks for 2 months a maximum follow-up was one year to evaluate the skin condition, pain, oedema and the joints function. The k-wires were removed after radiological union. Patients started partial weight bearing after fracture healing about 10-12 weeks postoperative depending on the original degree of comminution and the fracture healing then full weight bearing as pain tolerated. In the cases of poly trauma patients and according to other fracture fixation the weight bearing is customized. Follow-up monthly up to 1 year. Physiotherapy started both active and passive motions of the ankle, subtalar and midtarsal joints.
Results
The follow-up ranged from 8 to 12 months to have adequate time to assess the subtalar joint. Patients were generally operated within 48 h after admission even in the presence of bad skin conditions like open fractures, severe oedema and skin blisters unless if the patient is unfit for surgery. The operative time ranged from 30 to 40 minutes. There were no intraoperative complications. The postoperative x-ray revealed that Bohler’s angle was restored in 42 out of 50 fractures. The mean was 35 degrees (range 27 to 38 degrees). Also, the Gissane angle was restored in 45 fractures and the mean was 120 degrees (range 115 to 135 degrees). The calcaneal width was measured and compared with the normal side and 4 fractures had more than 12 mm of heel broadening. The width of calcaneus was restored in 44 out of 50 fractures. Also, the height of os calcis was corrected in 47 fractures. There were 3 patients having more than 10 mm discrepancy in heel height.
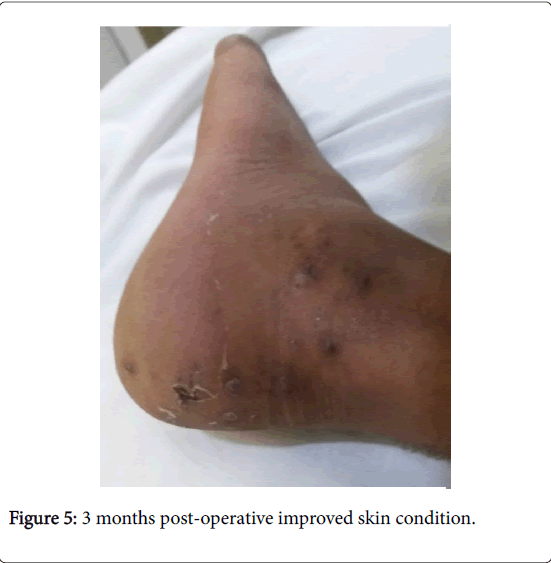
No patients complained of ankle dysfunction. 3 patients complained of peroneal tendon impingement. Subtalar movements were evaluated using the McMaster technique with comparison to the other side and there were 4 patients had comminuted fractures complained from restricted movements and pain. According to skin, the bad skin condition improved within 2 to 3 weeks postoperatively and there were no serious skin complications reported during follow-up. There was no deep infection of the bone (Figure 5).
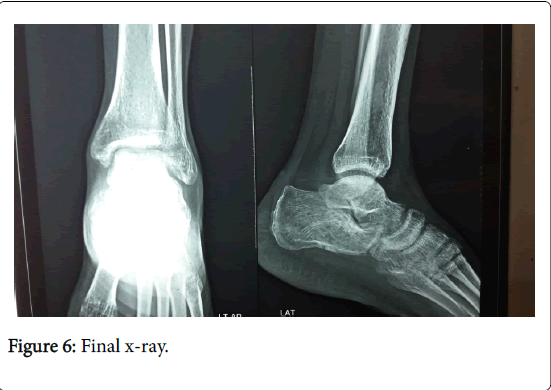
Out of all patients there were 3 diabetic patients reported with superficial pin tract infection at follow up which resolved with appropriate antibiotics and frequent dressing. Radiographic evaluation revealed, bony union was achieved in all patients ranged from 8 to 12 weeks (Figure 6). 4 patients had loss of reduction at final follow-up as compared to the immediate postoperative x-rays due to early removal of k-wires and early weight bearing by the patients. Patients were assessed by the American Orthopaedic Foot and Ankle Society (AOFAS) ankle hindfoot scale to assess functional outcome. 37 fractures were rated as excellent (74%), 9 patients rated as good (18%) and 4 patients had fair results (8%).
Discussion
There is a controversy between non-operatives versus operative treatment in calcaneal fractures. The aim of operative management is to achieve realignment of the posterior facet of the subtalar joint, restoration of bone morphology [16,17]. The decision of treatment depends on many factors like occupation, age, health comorbidity and associated injuries. In the case of open reduction the time is an important factor in determining surgical outcomes. Ideally, if skin condition is bad the time of surgery should be delayed for 10-14 days after trauma. This delay allows for soft tissue oedema and fracture blisters to resolve completely [15].
Open reduction and internal fixation of calcaneal fractures through extensile approaches have many complications like delayed wound healing, skin necrosis, deep infection, pain, chronic oedema, and damage to the sural nerve. Occasionally further plastic surgical treatment may be required. Also, the development of a deep wound infection often requires surgical interference [18-20].
This study included the patients with fracture calcaneus presented with soft tissues problems like severe edema, skin blisters, skin abrasions, and open fractures. According to skin condition, by this minimal invasive technique the bad skin condition improved within 2 weeks to 3 weeks postoperatively and there were no skin scar, infection, or other complications reported during follow-up. Also, there was no deep infection of the bone in the open calcaneal fractures which are obscure fractures. These injuries result from highenergy, polytraumatized patients. The management consists of irrigation and debridement then reduction of the fractures and k–wires fixation.
In this technique all patients treated by a minimal invasive technique by closed reduction and k-wires fixation. The displaced fragment reduced by schanz technique then the fragments stabilized by multiple k-wires. There were no the traditional wound for open reduction. The displaced tongue shaped fracture which was relatively simple and easy in manipulation with good results obtained. The joint depression fracture was more difficult than the tongue type in manipulation. In severely comminuted fracture the aim of surgery was restoration of the bone morphology as much as possible for subtalar fusion later on.
In this study there were many advantages. First of all the patients had undergone the operation within 48 h after the injury. The bad soft tissue conditions were not a contraindication and did not delay the time of surgery and did not wait for soft tissue improvement like formal open reduction and internal fixation. The early interference improved the skin conditions like blisters, severe oedema and open wounds. Also, early interference made the manipulation and reduction of displaced fragments easier than after delay. There were no traditional skin complications of formal open surgery like wound dehiscence, deep infection, ugly scar, bone infection damage to the sural nerve. There was no need for a second operation for implant removal. The advantages of this technique were decreasing the hospital stay, cost, hastening the recovery of the injured limb, early motion. Also, there were no postoperative scar formation and a less incidence of peroneal tendon dysfunction and subtalar joint arthritis.
The closed reduction and percutaneous k-wire fixation of displaced fractures in this study improved the radiological and clinical results and gave good mechanical stability, biological environment for bone healing and early motion. According to radiological results, the Bohler and Gissane angles were corrected to near normal 84% and 90% respectively indicating restoration of subtalar joint congruity and the normal calcaneal anatomy. According to the American Orthopaedic Foot and Ankle Society (AOFAS) ankle hindfoot scale to assess functional outcome. The mean score was 88 with a range from (73-98).
The complications reported in this study includes 3 diabetic patients with superficial pin tract infection at follow up which resolved with appropriate antibiotics and dressing. Also, four patients with comminuted fractures complained at last follow-up from subtalar arthritis and chronic subtalar pain and needed subtalar fusion. Four patients had loss of reduction at final follow-up as compared to the immediate postoperative x-rays due to loosening and early removal of k-wires and early weight bearing by the patients.
Zhang et al. reported in their study of comparing operative management of displaced intra-articular fractures with conservative treatment. Although the gait patterns and shoe wear improved these benefits were concealed by increases in wound complications [21]. Buckley et al. reported in a study, that the functional outcomes after open surgery of displaced intra-articular calcaneus fractures were better than those undergoing nonoperative treatment [22]. Dhillon et al. reported in a comparative study that minimally invasive surgery (MIS) can achieve a reasonable fracture reduction and that it can consider as the definitive treatment option for open fractures of the calcaneus [23]. Schuberth et al. concluded that a minimally invasive surgery in displaced intra-articular calcaneal fractures can restore the articular surface, calcaneal height with minimal risk of wound complications. They noticed significant improvements in soft tissue healing, articular step-off of the posterior facet, varus displacement, and the Boehler angle. No patients progressed to subtalar fusion [6].
Conclusion
Calcaneal fractures associated with bad skin conditions are best treated by a minimally invasive surgery by closed reduction and percutaneous k-wires fixation as there is no delay in surgery time like open procedures and there is a marvelous improvement of skin conditions. Also this technique improved the radiological and clinical results. The clinical and radiological results compared favorably with other reported minimal invasive and more invasive and high cost techniques.
Open calcaneal fractures are obscure fractures. Typically, these injuries result in a high-energy, polytraumatized patient population. Initial management consists of irrigation and debridement. Secondary forms of management continue to evolve. High-energy fracture subtypes and severe soft tissue injuries portend an unsatisfactory outcome, despite appropriate management. Standards for the type and timing of treatment have not been established.
Conflict of Interest
There are no conflicts of interest.
Funding
Nil.
Ethical Approval
The study was done under the local ethical committee of our institution.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
References
- Essex-Lopresti P (1952) The mechanism, reduction technique and results in fractures of the os calcis. Br J Surg 39: 395-419.
- Rammelt S, Grass R, Schikore H, Zwipp H (2002) Injuries of the chopart joint. Unfallchirurg 105: 371-383.
- Rammelt S, Gavlik JM, Barthel S, Zwipp H (2002) The value of subtalar arthroscopy in the management of intraarticular calcaneus fractures. Foot Ankle Int 23: 906-916.
- Rammelt S, Barthel S, Biewener A, Gavlik JM, Zuipp H (2003) Calcaneus fractures: Open reduction and internal fixation. Zentralbl Chir 128: 517-528.
- Gavlik JM, Rammelt S, Zwipp H (2002) Percutaneus arthroscopically assisted osteosynthesis of calcaneus fractures. Arch Orthop Trauma Surg 33: 63-71.
- Schuberth JM, Cobb MD, Talarico RH (2009) Minimally invasive arthroscopic-assisted reduction with percutaneous fixation in the management of intra-articular calcaneal fractures: A review of 24 cases. J Foot Ankle Surg 48: 315-322.
- Benirschke SK, Sangeorzan BJ (1993) Extensive intraarticular fractures of the foot. Surgical management of calcaneal fractures. Clin Orthop 128-134.
- Burdeaux BD (1997) Fractures of the calcaneus: Open reduction and internal fixation from the medial side a 21-year prospective study. Foot Ankle Int 18: 685-692.
- Grala P, Twardosz W, Tondel W, Olewicz-Gawlik A, Hrycaj P (2009) Large bone distractor for open reconstruction of articular fractures of the calcaneus. Int Orthop 33: 1283-1288.
- Boack DH, Wichelhaus A, Mittlmeier T, HoVmann R, Haas NP (1998) Therapy of dislocated calcaneus joint fracture with the AO calcaneus plate. Chirurg 69: 1214–1223.
- Brunner UH, Betz A, Halama R (1991) The surgical treatment of calcaneus fractures. Orthopade 20: 55–66.
- Cavadas PC, Landin L (2007) Management of soft-tissue complications of the lateral approach for calcaneal fractures. Plast Reconstr Surg 120: 459–466.
- Folk JW, Starr AJ, Early JS (1999) Early wound complications of operative treatment of calcaneus fractures: analysis of 190 fractures. J Orthop Trauma 13: 369–372.
- Sanders R, Fortin P, Di-Pasquale T, Walling A (1993) Operative treatment in 120 displaced intraarticular calcaneal fractures. Clin Orthop 290: 87–95.
- Varela CD, Vaughan TK, Carr JB, Slemmons BK (1993) Fracture blisters: Clinical and pathological aspects. J Orthop Trauma 7: 417-427.
- Sanders R (1992) Intra-articular fractures of the calcaneus: Present state of the art. J Orthop Trauma 6: 252-265.
- Thermann H, Krettek C, Hüfner T, Schratt HE, Albrecht K, et al. (1998) Management of calcaneal fractures in adults: Conservative versus operative treatment. Clin Orthop Relat Res 353: 107-24.
- Schepers T, Vogels LM, Schipper IB, Patka P (2008) Percutaneous reduction and fixation of intraarticular calcaneal fractures. Oper Orthop Traumatol 20: 168-175.
- Walde TA, Sauer B, Degreif J, Walde HJ (2008) Closed reduction and percutaneous Kirschner wire fixation for the treatment of dislocated calcaneal fractures: surgical technique, complications, clinical and radiological results after 2-10 years. Arch Orthop Trauma Surg 128: 585-591.
- DeWall M, Henderson CE, McKinley TO, Phelps T, Dolan L, et al. (2010) Percutaneous reduction and fixation of displaced intra-articular calcaneus fractures. J Orthop Trauma 24: 466-472.
- Zhang W, Lin F, Chen E, Xue D, Pan Z (2016) Operative versus nonoperative treatment of displaced intra-articular calcaneal fractures: A meta-analysis of randomized controlled trials. J Orthop Trauma 30: 75-81.
- Buckley R, Tough S, McCormack R (2002) Operative compared with nonoperative treatment of displaced intra-articular calcaneal fractures: A prospective, randomized, controlled multicenter trial. J Bone Joint Surg Am 84: 1733-1744.
- Dhillon MS, Gahlot N, Satyaprakash S, Kanojia RK (2015) Effectiveness of MIS technique as a treatment modality for open intra-articular calcaneal fractures: A prospective evaluation with matched closed fractures treated by conventional technique. Foot 25: 134-140.
Citation: Maaty MT, Khalek MA (2018) The Overcoming of Calcaneal Fractures Associated with Skin Problems through a Minimally Invasive Surgery by Closed Reduction and Percutaneous K-wires Fixation. Clin Res Foot Ankle 6: 254. DOI: 10.4172/2329-910X.1000254
Copyright: ©2018 Maaty MT, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4781
- [From(publication date): 0-2018 - Jun 11, 2025]
- Breakdown by view type
- HTML page views: 3914
- PDF downloads: 867