The Prevalence of Common Infectious Diseases among Nonmedical Prescription Opioid Users: Preliminary Findings from the National Prescription Opioid Misuse, Abuse, and Diversion (NOMAD) Study
Received: 02-Oct-2015 / Accepted Date: 26-Oct-2015 / Published Date: 29-Oct-2015 DOI: 10.4172/2161-1165.1000205
Abstract
Background: Little population data exist on the lifetime prevalence of risk-based infectious diseases, both those that are sexually transmitted and blood-borne via needle sharing among persons using prescription opioids for nonmedical purposes, such as those using for euphoria and/or to self-treat medical conditions. Objective: This study examined the lifetime prevalence and characteristics of persons reporting Common Infectious Diseases (CID) related to sexual risk and drug use in a national study of persons engaging in past-year nonmedical prescription opioid use (NMPOU) in the United States. Methods: The Nonmedical Prescription Opioid Misuse, Abuse, and Diversion (NOMAD) study collected selfreported survey assessments via an online questionnaire (ages 18+). Participants were recruited from online advertisements as well as referrals from ongoing research studies of prescription drug abusers in the United States. Participants were asked to self-report prior medically confirmed diagnoses of blood borne infectious diseases like HIV/AIDS, hepatitis (Hep A, Hep B, Hep C), and sexually transmitted infections like Syphilis. Risk behaviors, such as unprotected sex and needle sharing, were ascertained via standardized survey items drafted from the Composite International Diagnostic Interview. Results: Of the 344 past-year nonmedical prescription opioid users, 72.5% reported at least one lifetime CID. The most common were Hep B (18.8%), Hep A (8.9%), and Hep C (8.4%). Over 5% reported an HIV/AIDS diagnosis. The risk of onset for a CID was between 18 and 35, with 80% of the risk of a first STD in this window. Injection practices were associated with CIDs, and in particular Hep C and Hep A. The characteristics significantly associated with a lifetime CID were having bipolar disorder (O.R.=16.3), an opioid use disorder (O.R.=8.3), and a lifetime mood disorder (O.R.=6.83). Jail/prison and drug treatment were associated with a lower risk of disease risk. Most (95.4%) of the infectious diseases onsets prior to initiation of the NMPOU. Conclusion: This study highlights that common infectious diseases, both STDs and injection-based (e.g., Hep- A,B,C) are very common among NMPOUs, though the risk onset is largely in early adulthood prior to the initiation of NMPOU.
Keywords: Infectious Diseases; National prescription opioid misuse, abuse, and diversion (NOMAD)
163544Introduction
Sexually transmitted diseases (STDs), sometimes referred to as infections, are among the most common physical health conditions in the United States today. According to the United States Centers for Disease Control and Prevention (CDC), about 19 million persons are infected each year [1]. STDs are primarily caused by viruses (e.g., hepatitis virus, human immunodeficiency virus), bacteria (e.g., Chlamydia trachomatis, Treponema pallidum), and fungi/parasites (e.g., Candida albicans). The most common routes of transmission are through sexual contact as well as the exchange of bodily fluids through needles shared among injection drug users [2,3]. STDs are more common among drug users [4,5]. Moreover, HIV/AIDS (1.2 million in 2015) and HCV (3.9 million in 2015) are also more prevalent among drug abusers, particularly persons who inject drugs [6]. Overall, there is little doubt that illicit drug use is associated with several commonly occurring infectious diseases (CIDs).
In terms of biological factors, 20% of HIV/AIDS and 75% of HCV are attributable to intravenous drug use [7]. Those with a history of addiction may exhibit diminished psychological capacity to engage in preventive health behaviors, such as condom use during periods of heavy drug use [8]. Further, structural factors, such as the ability to access a steady supply of drugs and sustain financial support for purchasing drugs (e.g., sex-work/trading), may place a drug user at high risk of acquiring a drug-related infectious disease [9]. In particular, abusers of prescription drugs may be a unique risk as well. In 2015, over 150 incident cases of HIV infection occurred among persons reporting injecting the prescription pain reliever-Opana™ [10].Limited access to syringe exchange programs among persons injecting prescription opioids was identified as the primary causal factor in this micro-epidemic [11]. Among the range of prescription drugs that are commonly used nonmedically, opioids are perhaps the most common. Data from the most recent National Survey on Drug Use and Health revealed that in 2013, an estimated 20.3% of respondents reported past-year nonmedical use of prescription pain reliever products, which included opioid-based medications [12]. Injection as a means of administering the drug tends to be more common among opioid users relative to nonmedical use of other types of prescription drugs, such as stimulants or sedatives-hypnotics [13]. Recent increases in heroin initiation also appear to be largely driven by former nonmedical prescription opioid use, highlighting its strong connection to illicit drug use [14].
Population data on the prevalence of the most commonly occurring drug-related infectious diseases (CIDs) in the United States are largely derived from public health surveillance systems involving biological testing through local public health departments. While this system provides credible estimates at the population-level, it leaves gaps in specific subgroups that may be at higher-than-average vulnerability or in need of specialized intervention strategies. To better understand the prevalence of STDs and injection-related diseases, heretofore referred to as Common Infectious Diseases (CID) among nonmedical prescription opioid users (NMPOUs), data were analyzed from an ongoing surveillance study, the National Opioid Misuse, Abuse, and Diversion study (NOMAD).
Methods
The NOMAD study is a national survey of nonmedical prescription opioid users that was administered to 350 English-speaking adults age 18 or older in September of 2015. Recruitment involved a two-stage process. For the first stage, individuals were recruited via online advertisements on Craigslist, drug forums/chat-rooms, and ongoing research studies of prescription drug abusers. The candidate participants were informed that the study was recruiting for a study about prescription pain reliever medications. In the advertisement, they were asked to e-mail a member of our study team with their interest. If they passed the screening questions (i.e., United States citizen, used prescription pain reliever medications non-medically), they were provided a link to the full survey. The candidate was also provided with a unique ID and a link to take an online screening instrument.
The survey was programmed to identify duplicate IP addresses as well as duplicate latitude and longitude coordinates derived from the IP address. For instance, a person may have a dynamic IP address that changes with each session, but the IP address is geocoded to the latitude and longitude coordinates of the active session. Respondents who had privacy filters that hid their IP address and location information were not allowed to take the survey. In addition, the participant was asked to identify the location where they were taking the survey (by state), and to be eligible, the information must have matched the location from their IP address.
Subjects were paid $35 for their participation, and the survey took an average of 35 minutes to complete. Slightly less than 10% of the respondents (n=36 of 390) did not complete the entire survey. Of the complete survey responses, there were 36 fraudulent attempts to the take the survey, accounted for by four unique IP addresses. Approximately 95% of the surveys were completed on desktop machines, with 4% completed via a portable device, most likely iPads. The Human Subjects Committee at RTI International approved these recruitment and consent procedures.
The survey was developed using the Composite International Diagnostic Interview Schedule (CIDI) as a basic starting point. The CIDI is an interviewer-administered instrument, so the questions were modified for self-administration. The final Flesh-Kincaid reading level was 8th grade, or approximately 13 years old. The questions were also drawn from the National Survey on Drug Use and Health, which also uses the CIDI as the basic interview schedule. Additional questions were added to enhance the comprehensiveness of the survey to cover relevant topics such as motivations for using different types of licit and illicit drugs, routes of administration, and knowledge, attitudes, and behaviors involving risky consumption practices. Finally, a sexual risktaking module was adapted from previous RTI International work for online administration [15].
Analyses were conducted on the full sample of respondents that completed the entire survey. Initial demographic comparisons between completers and attriters indicated that the attriters were more likely to be younger, white, and never married. These variables were included as covariates in subsequent analytic models. In terms of statistical analyses, cross-tabulations were used to estimate the prevalence of lifetime STDs. The actuarial method was used to estimate the age-ofonset curves.
Logistic regression was used to estimate the correlates of comorbidity between NMPOU and commonly occurring infectious diseases. The lifetime patterns of mental health and drug history characteristics were added to a model that controlled for age, sex, and race. Each characteristic was entered separately. The risky sexual behavior and needle sharing characteristics were asked in reference to engagement of those activities in the past year. The logits and their 95% confidence intervals were converted into odds ratios by exponentiation for ease of interpretation. Statistical significance was estimated using 2- tailed 0.05-level tests. Because of the small number of a-priori comparisons, no corrections for multiple comparisons were deemed necessary.
Results
Sample characteristics
The sample was composed of persons who consumed at least one prescription opioid non-medically in the past year (Table 1). Similar to studies of illicit drug users, the sample was composed of mostly males (75%), young adults aged 25-34 (66%), and non-Hispanic whites (70%). Respondents from 42 different states completed the survey and they were mostly single/never married (49%) or divorced (45%). Most of the respondents had a high school education or higher (95%). In terms of background risk factors for CIDs, about 1 in 5 (20%) reported initiation of prescription opioids prior to age 18, whereas most (58%) initiated their use between the ages of 18 to 24. Most (70%) identified themselves as heterosexual. The remaining 30% were distributed between those identifying as exclusively lesbian/gay (13%) or bisexual (16%). The sample was also very diverse in terms of risk behaviors, with over one-fifth (20%) reporting at least 3 or more lifetime symptoms of opioid dependence. Slightly less than half had engaged in intravenous drug use in their lifetime.
| Characteristic | Percentage | Sample n |
|---|---|---|
| Sex | ||
| Male | 75.2 | 251 |
| Female | 24.8 | 83 |
| Age | ||
| 18-24 | 6 | 20 |
| 25-34 | 66.5 | 222 |
| 35 or older | 27.5 | 92 |
| Race | ||
| White | 70.6 | 236 |
| Black | 12.9 | 43 |
| Hispanic | 14.1 | 47 |
| Other | 2.4 | 8 |
| Marital | ||
| Single, never married | 49.7 | 166 |
| Married | 5.1 | 17 |
| Divorced | 45.2 | 151 |
| Education | ||
| High school grad or less | 14.9 | 50 |
| Some college/technical school | 44.6 | 199 |
| College grad or more | 40.4 | 135 |
| Age of first prescription pain reliever use | ||
| <18 | 20.6 | 69 |
| 18-24 | 57.5 | 192 |
| 25 or older | 21.9 | 73 |
| Sexual orientation | ||
| Straight | 70 | 224 |
| Lesbian/gay | 13.4 | 43 |
| Bisexual | 16.6 | 53 |
| Any STD | 72.5 | 242 |
| Nonmedical prescription opioid use before STD | 4.6 | 11 |
| Lifetime opioid disorder symptoms | 20.9 | 70 |
| Lifetime injection drug use | 45.5 | 152 |
Table 1: Characteristics of NOMAD Study, 2015.
Lifetime prevalence of common infectious diseases (CIDs)
As shown in Table 2, slightly more than 72% of respondents reported a diagnosis of at least one of the commonly occurring infectious diseases investigated in this study. The breakdown was such that 5.9% reported a diagnosis of HIV/AIDS, 8.9% reported Hep A, 18.8% reported Hep B, 8.4% reported Hep C, and 31.7% reported other infections, such as STDs. Overall, lifetime intravenous drug use was highly associated with the presence of an infectious disease (Chi- Square 28.9, 1df, P<0.001).
| Non-Inject | Inject | Total | Test | ||||
|---|---|---|---|---|---|---|---|
| % | N | % | N | % | N | Chi-Sq (df) P-value | |
| HIV/AIDS | 4.9 | 9 | 5.9 | 9 | 5.4 | 18 | 0.68 (1)P=0.694 |
| Hep A | 1.7 | 3 | 17.7 | 27 | 8.9 | 30 | 26.8 (1)P<0.001 |
| Hep B | 17 | 31 | 21.5 | 32 | 18.8 | 63 | 0.87 (1)P=0.354 |
| Hep C | 4.4 | 8 | 13.6 | 20 | 8.4 | 28 | 8.27 (1)P<0.004 |
| Other STD | 32.9 | 60 | 30.3 | 46 | 31.7 | 106 | 0.58 (1)P=0.587 |
| Any STD | 60.4 | 110 | 86.8 | 132 | 72.5 | 242 | 28.9 (1)P<0.001 |
Note: Abbreviations: %: Percent, df: Degrees of Freedom, N: Sample Size
Table 2: Lifetime prevalence estimates of common infectious disease (CIDs) by injection status.
Patterns of onset for a common infectious diseases (CID)
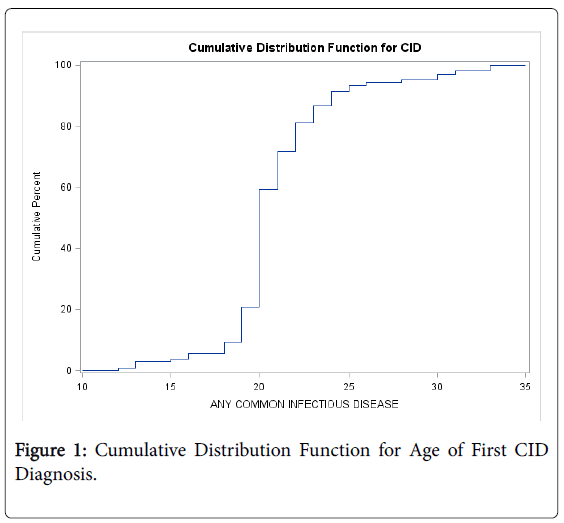
As shown in Figure 1, the cumulative distribution function (CDF) describes the unadjusted probability of onset for an STD. In the NOMAD study, the CDF reveals that the risk of onset for the first CID was between the ages of 20 and 25, where there was an increase of nearly 60 percentage points. Put another way, about 20% of those with an STD reported receiving their diagnosis by the time they were 20 years old. By age 25, approximately 80% of those with a CID had received a diagnosis. The risk of a first CID diagnosis was less than 1% after age 35.
A limitation of the CDF is that it calculates the risk of an event only on those with the event. It does not account for censoring, which occurs when the risk of an event may persist after the study ends. With regard to the present investigation, the risk of a first CID for those who have not yet received a diagnosis may occur well beyond after the survey was completed. To illustrate, persons who completed the survey at age 18 may still be at risk for a CID after age 18. The survey counts these individuals as non-cases, but if the survey had tracked them longer, these non-cases could be converted to a case.
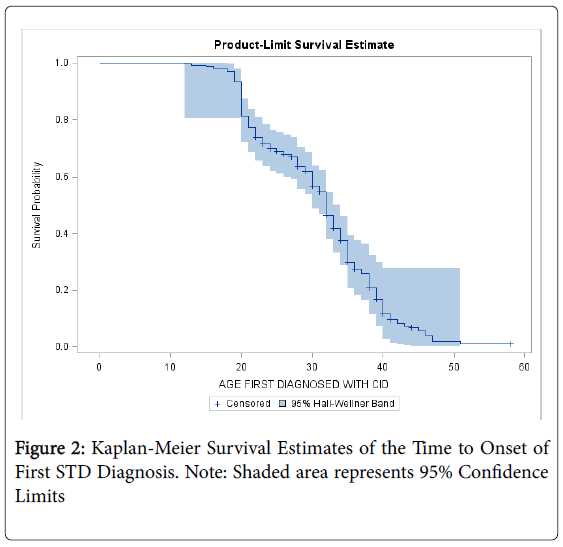
To account for right-censoring, survival analytic techniques (e.g., Kaplan-Meier Curves) compute the hazard of onset at time T, conditional on the sample of persons who have not yet experienced the outcome by time T-1. As shown in Figure 2, the risk of onset is shifted past age 35 when censoring is taken into account. This finding indicates that the projected lifetime risk of a first CID reaches 20% of the entire population of NMPOUs at age 35, about 10 years later than the CDF. According to the Kaplan-Meier estimate, the risk of initiation is greatest between ages 18 to 35. Only 10% of the population is expected to receive their first CID diagnosis after age 40.
Characteristics of lifetime CIDs
The logistic regression models showing the characteristics of those with a CID are located in Table 3. Raising the risk by nearly 16 times, a diagnosis of bipolar disorder was the strongest predictor of an STD diagnosis (O.R=16.3, 95% C.I=2.1-125.5, P<0.001). Having an opioid disorder was also highly correlated with one of the CID diagnoses (O.R=8.27, 95% C.I=2.41-28.33, P<0.003). Of interest was that persons reporting lifetime drug treatment (O.R=0.25, 95% C.I=0.11-0.58, P<0.001) or jail/prison (O.R=0.04, 95% C.I=0.0.1-0.19, P<0.001) were less likely to have a CID diagnosis. The presence of an anxiety disorder was unrelated to a CID diagnosis. Trading sex for drugs (O.R=10.6, 95% C.I=4.87-23.1, P<0.001) and re-using needles (O.R=18.7, 95% C.I=1.9-100.1, P<0.001) was highly correlated with having received a diagnosis of at least one CID in one’s lifetime. Having sex while under the influence of drugs in the past year was not statistically correlated with a CID diagnosis.
| % | O.R. | 95% C.I. | P-Value | |
|---|---|---|---|---|
| Opioid Disorder, LF | 95.7 | 8.27 | 2.41-28.33 | <0.001 |
| Injection Drug Use, LF | 86.8 | 4.57 | 2.31-9.04 | <0.001 |
| Mood Disorder, LF | 90.6 | 6.83 | 3.24-14.32 | <0.001 |
| Anxiety Disorder, LF | 50 | 0.34 | 0.79-1.59 | 0.153 |
| Bipolar Disorder, LF | 97.1 | 16.3 | 2.1-125.5 | <0.001 |
| Drug treatment, LF | 67.7 | 0.25 | 0.11-0.58 | <0.001 |
| Jail or prison, LF | 64.4 | 0.04 | 0.01-0.19 | <0.001 |
| Sex while under influence of drugs, PY | 77.8 | 1.65 | 0.87-3.12 | 0.118 |
| Traded sex for drugs, PY | 91.5 | 10.6 | 4.87-23.1 | <0.001 |
| Re-used needles for others, PY | 97.8 | 18.7 | 1.9-100.1 | <0.001 |
Note: Abbreviations: O.R: Odds Ratio, C.I: Confidence Interval, %: percent, LF: lifetime, PY: Past Year.Each variable entered separately; all models control for age, race, sex, education
Table 3: Lifetime comorbidity of common infectious disease (CIDs) with behavioral and structural characteristics.
Table 4 presents the bivariable associations between the two major categories that comprise CIDs---sexually transmitted diseases and drug use transmitted diseases (e.g., hepatitis). HIV was excluded from this analysis due to small sample size. We also excluded those who reported both an STD and hepatitis (n=226). Therefore, this analyses examined the differences between those with only an STD or hepatitis (n=221). Persons with an opioid use disorder (62% versus 30%), bipolar disorder (59% versus 31%), sex under the influence (80% versus 42%), and trading sex (77% versus 31%) were more likely to have an STD relative to hepatitis. Conversely, those who were injection drug users (63% versus 41%), in drug treatment (62% versus 32%), and reusing needles (90% versus 45%) were more likely to have hepatitis than an STD.
| Hepatitis (A,B,C) | STD | Chi-sq | df | P-value | |||
|---|---|---|---|---|---|---|---|
| % | N | % | N | ||||
| Opioid disorder | 30.7 | 20 | 62.7 | 101 | 19 | 1 | <0.001 |
| Injection drug use | 63.7 | 79 | 41.1 | 42 | 11.4 | 1 | <0.001 |
| Mood disorder | 47.9 | 47 | 57.8 | 74 | 2.16 | 1 | 0.141 |
| Bipolar disorder | 31.9 | 15 | 59.2 | 106 | 11.2 | 1 | 0.008 |
| Drug treatment | 62.1 | 100 | 32.3 | 21 | 16.5 | 1 | <0.001 |
| Jail or prison | 54.7 | 80 | 51.2 | 41 | 0.26 | 1 | 0.609 |
| Sex under influence | 42.5 | 68 | 80.3 | 53 | 26.8 | 1 | <0.001 |
| Traded sex for drugs | 31.3 | 37 | 77.8 | 84 | 48.8 | 1 | <0.001 |
| Re-used needles for others | 90 | 36 | 45.7 | 85 | 29.5 | 1 | <0.001 |
Note: Abbreviations: STD: Sexually Transmitted Disease, %: Percent, df: Degrees of Freedom. Anxiety dropped because of skewed distribution.Individuals with both diseases (n=226) were excluded
Table 4: Lifetime comorbidity of hepatitis and STDs by behavioral and structural characteristics.
Conclusion
This is one of the first national studies investigating the prevalence of STDs among nonmedical prescription opioid users (NMPOUs) in the United States. There have been numerous studies investigating the linkages between drug use and STDs [16], but few that have specifically examined STDs among NMPOUs. We found very high numbers of STDs among this population (72.5%), including Hepatitis (A, B, and C), HIV/AIDS, and bacterial STDs. The period of greatest risk for first diagnosis appears to be between the ages of 18 to 35. Moreover, STDs were more common among those with an opioid use disorder, as well as mental health illnesses such as mood and bipolar disorders. Interestingly, respondents noting a history of being in the criminal justice or drug treatment systems were less likely to report an STD compared to those without these characteristics. There were significant differences in the characteristics of those with either disorder on the lengthy list of structural and behavioral characteristics.
The mechanisms underlying the associations between STDs and NMPOUs have yet to be investigated. One finding that was somewhat unexpected was the negative association between structural characteristics (e.g., community services) and STDs. More specifically, jail/prison and drug treatment were associated with a lower likelihood of STDs. There are two plausible explanations. The first is that these organizations instill, either directly or indirectly, motivation to engage in safe behaviors. The second is that opportunities to engage in risky behaviors are limited in such a highly structured environment. These data are unable to resolve either pathway, so future longitudinal studies are needed to test how structural characteristic and STDs are causally related.
A second important finding is the degree to which personal characteristics were associated with STDs. Persons with mood and bipolar disorders had higher proportions of STDs compared to individuals without these disorders. This finding is consistent with other studies investigating drug use and risky sexual behaviors in a wide range of population sub-groups, such as sexual and racial minority groups [17-19]. In terms of bipolar disorder, one of the symptoms is extreme mania. Hyper-sexuality is part of a constellation of adverse health behaviors during manic episodes [20,21]. Instead of a causal pathway whereby bipolar disorder affects the likelihood of an STD, it is possible that both STDs and NMPOU may be linked to a common fundamental causal factor, such as impulsivity [22]. Longitudinal studies are best equipped to address this very important point.
There are numerous limitations to this study that should be noted. Perhaps the most significant limitation of this work is that the diagnosis of a specific STDs is based on self-reported diagnoses of a condition that had been previously diagnosed by a medical physician. This method is must more limited employing a biological confirmation on each research participant. Because we were interested in diagnoses, the prevalence estimates cited here likely underestimate the true population prevalence. Depending upon the symptom severity, it could be months or perhaps even years before symptoms reach the point in which the person seeks any sort of treatment. Rates of detection are difficult to precisely estimate. The reason is that some tests have low rates of detection among infected persons. For example, most tests are about 90% to 95% accurate [23], meaning that up to 10% of positive individuals may receive incorrect diagnoses. The prospect of re-testing to confirm the diagnosis notwithstanding, the biggest reason for lack of detection is that persons with STDs can remain relatively symptomfree for several years [24-26]. While studies based on self-reported STD status are likely to yield estimates toward the lower bound of the true population prevalence, it is important to note that such studies add value to the scientific literature. Screening for STDs in a population-based study is exceptionally cost-prohibitive and is often not feasible. This is especially true in studies where the sexual history data are a second tier research priority. The data presented herein are to be regarded as preliminary and in need of replication.
Other limitations of the study are as follows. The study did not collect detailed information on sexually transmitted infections, particularly those that are treatable with antibiotics. While those types of sexually transmitted infections are contagious and impairing, they do not have the same level of impact as diseases such as HIV/AIDS and Hep C. Another limitation is that the study was also based on reactive recruitment strategies, such as responses to advertisements. There are many unknown factors that are difficult to adjust for in terms of statistical models. Some studies use propensity weighting post-hoc to balance the study using known characteristics that discriminate between those in the sample from those not in the sample but sharing the same population characteristics [27,28]. The current study recruited from a diverse range of geographic areas in an attempt to broaden the sample and reduce the likelihood of selection biases. However, we cannot be entirely confident that all selection biases have been removed.
In conclusion, the lifetime prevalence of STDs in the sample of NMPOUs calls attention to the importance of prevention of STDs. In terms of public health initiatives, such as Seek, Test, Treat for STDs like HIV, a question remains regarding the role of primary prevention of drug use as a means of preventing STDs as secondary prevention. That is, preventing drug use should reduce the likelihood of STDs. These findings suggest that most participants had been diagnosed with an STD prior to onset of NMPOU. Therefore, prevention among NMPOUs would seem fruitless, given that they had been previously infected with an STD. Prevention of a first STD should occur much earlier in life, and perhaps there is an opportunity to discuss the prevention of NMPOU during STD interventions as well. Nonmedical prescription drug use is a “hidden epidemic” because many users have high levels of social functioning and can maintain their consumption for months to years without detection [13]. Lately, many young users are transitioning to heroin with the decrease in availability of potent prescription pain relievers, particularly in the suburbs [29,30]. HIV and drug use have been referred to as the twin epidemics that have plagued the United States. Of late, prescription drug use and STDs also appear to be concomitant public health issues in desperate need of further inquiry.
Acknowledgments
This study was supported by institutional funds from RTI International, the National Institute on Drug Abuse (PI Novak, DA030427), and the Pfizer Foundation. We gratefully acknowledge the participants for taking the time to share their data. We also acknowledge the assistance of Claire Dean at the Global Drug Survey for her assistance with the survey and ongoing field management of the study.
References
- Boily MC, Baggaley RF, Wang L, Masse B, White RG, et al. (2009) Heterosexual risk of HIV-1 infection per sexual act: systematic review and meta-analysis of observational studies.Lancet Infect Dis 9: 118-129.
- Fleming DT, Wasserheit JN (1999) From epidemiological synergy to public health policy and practice: the contribution of other sexually transmitted diseases to sexual transmission of HIV infection. Sexually Transmitted Infections 75: 3-17.
- DiClemente RJ, HansenWB, Ponton LE(2013) Handbook of adolescent health risk behavior. Springer Science & Business Media.
- Wechsberg WM, Golin C, El-Bassel N, Hopkins J, Zule W (2012) Current interventions to reduce sexual risk behaviors and crack cocaine use among HIV-infected individuals.Curr HIV/AIDS Rep 9: 385-393.
- Baggaley RF, Boily MC, White RG, Alary M (2006) Risk of HIV-1 transmission for parenteral exposure and blood transfusion: a systematic review and meta-analysis.AIDS 20: 805-812.
- de Graaf R, Vanwesenbeeck I, van Zessen G, Straver CJ, Visser JH (1995) Alcohol and drug use in heterosexual and homosexual prostitution, and its relation to protection behaviour.AIDS Care 7: 35-47.
- Strathdee SA, Lozada R, Martinez G, Vera A, Rusch M, et al. (2011) Social and structural factors associated with HIV infection among female sex workers who inject drugs in the Mexico-US border region.PLoS One 6: e19048.
- Strathdee SA, Beyrer C (2015) Threading the Needle--How to Stop the HIV Outbreak in Rural Indiana.N Engl J Med 373: 397-399.
- Merikangas KR, McClair VL (2012) Epidemiology of substance use disorders.Hum Genet 131: 779-789.
- Novak SP. (2011) The epidemiology of prescription drug disorders in the United States Intech 2011, New York InTech
- Kolodny A, Courtwright DT, Hwang CS, Kreiner P, Eadie JL, et al. (2015) The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction.Annu Rev Public Health 36: 559-574.
- Wechsberg WM, Novak SP, Zule WA, Browne FA, Kral AH, et al. (2010) Sustainability of intervention effects of an evidence-based HIV prevention intervention for African American women who smoke crack cocaine.Drug Alcohol Depend 109: 205-212.
- Klitzman RL, Pope HG Jr, Hudson JI (2000) MDMA ("Ecstasy") abuse and high-risk sexual behaviors among 169 gay and bisexual men.Am J Psychiatry 157: 1162-1164.
- Crosby RA, DiClemente RJ, Wingood GM, Rose E, Lang D (2003) Correlates of continued risky sex among pregnant African American teens: implications for STD prevention.Sex Transm Dis 30: 57-63.
- Seth P, Sales JM, DiClemente RJ, Wingood GM, Rose E, et al. (2011) Longitudinal Examination of Alcohol Use: A Predictor of Risky Sexual Behavior and Trichomonas vaginalis Among African-American Female Adolescents. Sexually Transmitted Diseases 38: 96-101.
- Wingood GM, DiClemente RJ (1998) The influence of psychosocial factors, alcohol, drug use on African-American women's high-risk sexual behavior.Am J Prev Med 15: 54-59.
- Basco MR, Celis-de Hoyos CE (2012) Biopsychosocial Model of Hypersexuality in Adolescent Girls With Bipolar Disorder: Strategies for Intervention. J Child Adolesc Psychiatr Nurs. 25:42-50.
- Perugi G (2012) Clinically relevant subtypes of mania. International Clinical Psychopharmacology 28: e15-e16.
- Dvorak RD, Wray TB, Kuvaas NJ, Kilwein TM (2013) Mania and sexual risk: associations with behavioral self-regulation.J Affect Disord 150: 1076-1081.
- Hecht FM, Busch MP, Rawal B, Webb M, Rosenberg E, et al. (2002) Use of laboratory tests and clinical symptoms for identification of primary HIV infection.AIDS 16: 1119-1129.
- Ashley-Morrow R Krantz E, Wald A (2003) Time course of seroconversion by HerpeSelect ELISA after acquisition of genital herpes simplex virus type 1 (HSV-1) or HSV-2.Sex Transm Dis 30: 310-314.
- Fortenberry JD (1997) Health care seeking behaviors related to sexually transmitted diseases among adolescents.Am J Public Health 87: 417-420.
- Hook EW 3rd, Richey CM, Leone P, Bolan G, Spalding C, et al. (1997) Delayed Presentation to Clinics for Sexually Transmitted Diseases by Symptomatic Patients: A Potential Contributor to Continuing STD Morbidity. Sexually Transmitted Diseases 24: 443-448.
- Novak SP, Kroutil LA, Williams RL, Van Brunt DL (2007) The nonmedical use of prescription ADHD medications: results from a national Internet panel.Subst Abuse Treat Prev Policy 2: 32.
- Spijkerman R, Knibbe R, Knoops K, Van De Mheen D, Van Den Eijnden R (2009) The utility of online panel surveys versus computer-assisted interviews in obtaining substance-use prevalence estimates in the Netherlands.Addiction 104: 1641-1645.
- Cicero TJ, Ellis MS, Surratt HL, Kurtz SP (2014) The changing face of heroin use in the United States: a retrospective analysis of the past 50 years.JAMA Psychiatry 71: 821-826.
- Ciccarone D, Bourgois P (2003) Explaining the geographical variation of HIV among injection drug users in the United States.Subst Use Misuse 38: 2049-2063.
Citation: Novak SP, Ball EL, Winstock AR, Peiper N (2015) The Prevalence of Common Infectious Diseases among Nonmedical Prescription Opioid Users: Preliminary Findings from the National Prescription Opioid Misuse, Abuse, and Diversion (NOMAD) Study. Epidemiology (sunnyvale) 5:205. DOI: 10.4172/2161-1165.1000205
Copyright: © 2015 Novak SP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 11674
- [From(publication date): 12-2015 - Aug 30, 2025]
- Breakdown by view type
- HTML page views: 10768
- PDF downloads: 906