The Prevalence of Depression in Patients with Diabetes Mellitus Type II in the Shahid Rahimi Hospital of Khorramabad, Iran
Received: 13-May-2016 / Accepted Date: 03-Jun-2016 / Published Date: 10-Jun-2016 DOI: 10.4172/2161-1165.1000249
Abstract
Background: Diabetes is a chronic illness requiring continuous medical care. Depression is comorbid with diabetes and is associated with poorer glycemic control, and increased complications.
Objectives: The main aim was to assess the prevalence of depression among patients with diabetes mellitus type II to find a correlation between age, gender, HbA1C level, duration of time since the diagnosis of diabetes, number of admissions, methods of controlling diabetes, place of residence, smoking, comorbidities, and educational levels.
Materials and Methods: 169 diabetic patients participated. The methods of data collection included the Beck questionnaire Inventory and an oral interview. Then other data were obtained and were analyzed using SPSS 21.
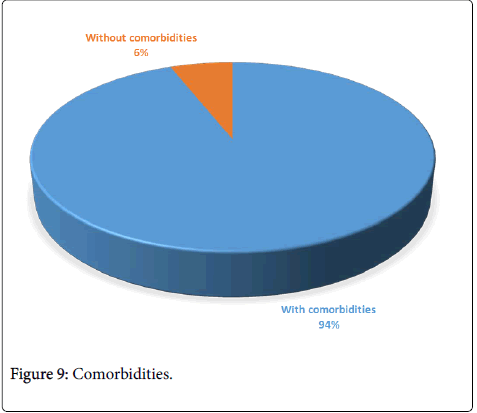
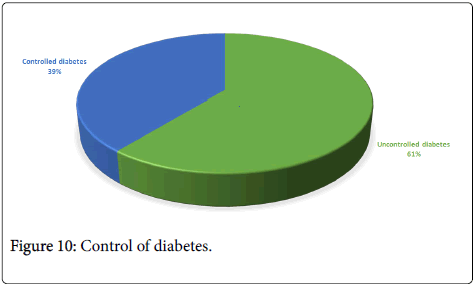
Results: 130 patients (76.9%) were depressed (25.38% mild, 55.38% moderate, 19.23% severe). Only gender had a relationship with depression, and depression was higher in the females (P=0.041). 59.17% of the patients were illiterate and only 5.91% were academically educated, 94% had other comorbidities, and 60.94% had uncontrolled diabetes and HbA1C higher than 8.
Conclusions: Depression has high prevalence among diabetic patients, and it is affected only by gender. The control of diabetes among them is very poor, and most of them have other comorbidities.
Keywords: Depression, Diabetes mellitus Type 2, HbA1c, IGT, IFG
164748Background
Reports from the International Diabetes Federations (IDF) indicate that the prevalence of diabetes mellitus has reached epidemic levels globally [1]. People with diabetes have an increased risk of developing a number of serious health problems, particularly if their diabetes is poorly controlled. Chronically high blood glucose levels can lead to serious diseases affecting the heart and blood vessels, eyes, kidneys and nerves. In addition, people with diabetes have a higher risk of developing infections. In many countries, diabetes is a leading cause of cardiovascular disease, blindness, kidney failure and lower limb amputation [2].
Depression is a common illness worldwide, with an estimated 350 million people affected. Especially when long-lasting and with moderate or severe intensity, depression may become a serious health condition. It can cause the affected person to suffer greatly and function poorly at work, at school and in the family.
Effective treatments for depression, fewer than half of those affected in the world (in many countries, fewer than 10%) receive such treatments [3]. Depression is a common problem among those suffering from diabetes mellitus [4].
Depression and severe psychological distress are frequently comorbid with diabetes and are associated with reduced adherence to medication and healthy lifestyle regimens, poorer glycemic control, and increased complications [5]. Diabetes complications are also greater among individuals with depression [1]. Recent studies have shown that coexisting depression increases the risk of death among people with diabetes [6-8].
Objective
The main aim of this study is to assess the prevalence of depression among patients with diabetes mellitus type II and to find a correlation between age, gender, HbA1C level, duration of time since the diagnosis of diabetes, number of admissions, methods of controlling diabetes used, place of residence, smoking, comorbidities, and educational attainment levels.
Materials and Methods
This cross-sectional study was done on patients with diabetes mellitus type II, who had been admitted to the Shahid Rahimi Hospital in Khorramabad, west of Iran, from summer 2014 to winter 2015.
Inclusion/exclusion criteria
The aim of admission was not just the control of diabetes or its complications. The patients were admitted with various complaints. The most important inclusion criterion was suffering from type II diabetes. Other criteria were full awareness and ability to talk and respond to questions orally.
Those patients who were unable to respond or had not taken the HbA1C test were eliminated. Eventually 169 patients were selected.The methods of data collection included a questionnaire and an oral interview. After the patients were convinced and consents were obtained, the study started.
Having filled the questionnaire, the patients were interviewed individually. Then based on DSM-V criteria and the results of the questionnaire, the patients were assessed for depression and its severity. The questionnaire used was the Beck Depression Inventory questionnaire, which is a standard one, including 21 sections and each section containing different and separate implications.
We got other data from the patients including age, educational attainment levels, marital state, place of residence (urban or rural areas), duration of time since the diagnosis of diabetes mellitus, the method of controlling diabetes (taking tablets or insulin injection), and comorbidities. Then, the HbA1C test was administered.
According to Beck depression inventory questionnaire, we have asked about 21 part of this questionnaire (including Sadness, pessimism, past failure, loss of pleasure, guilty feelings, punishment feelings, self-dislike, self-criticalness, suicidal thoughts or wishes, crying, agitation, loss of interest, indecisiveness, worthlessness, loss of energy, changes in sleeping pattern, irritability, changes in appetite, concentration difficulty, tiredness or fatigue, loss of interest in sex) [9].
Then we have given score to each section. After that we have calculated the final score for each patient. According to the final score, we could be able to classify the depression to mild (score 5 to 9), moderate (score 10 to 18) and severe depression (more than 19) [10].
According to the formula “n=Z2p(1-p)/d2” we estimated 170 patients as the sample size. The collected data were analyzed using SPSS 21 software.
Results
There were 169 cases (69 females and 73 males). One patient was omitted, because of the lack of HbA1C test. 130 patients (76.9%) were depressed. Among the depressed patients, 25.38% had mild, 55.38% had moderate, and 19.23% had severe depression.
The results were segregated according to these items: age, sex, educational attainment levels, smoking, the number of admissions, the method of controlling diabetes (taking tablets, insulin injection), the place of residence (urban or rural areas), duration of time since the diagnosis of diabetes mellitus, comorbidities and the HbA1C test.
The distribution and severity of depression for age, HbA1C level, duration of time since the diagnosis of diabetes, educational attainment levels, smoking, number of admissions, place of residence (urban or rural areas), method of controlling diabetes and comorbidities:
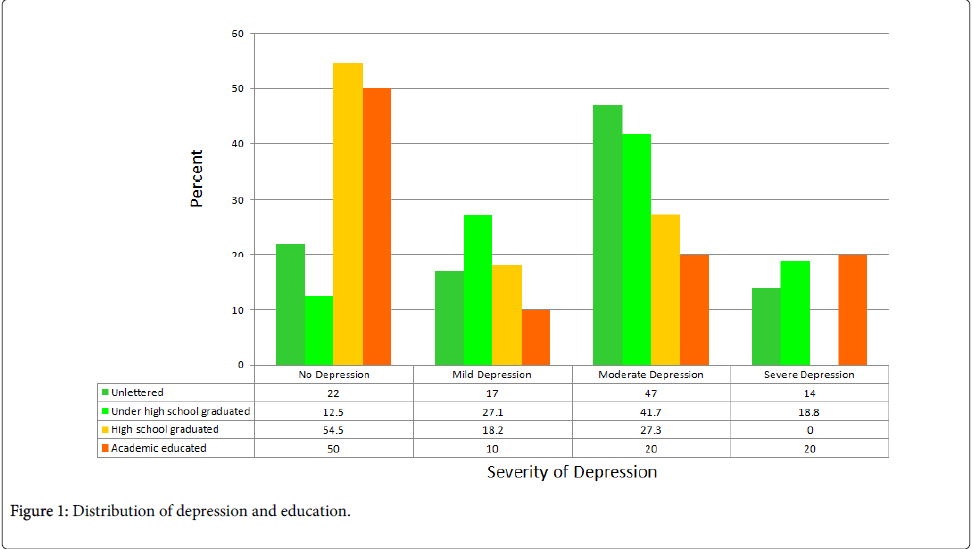
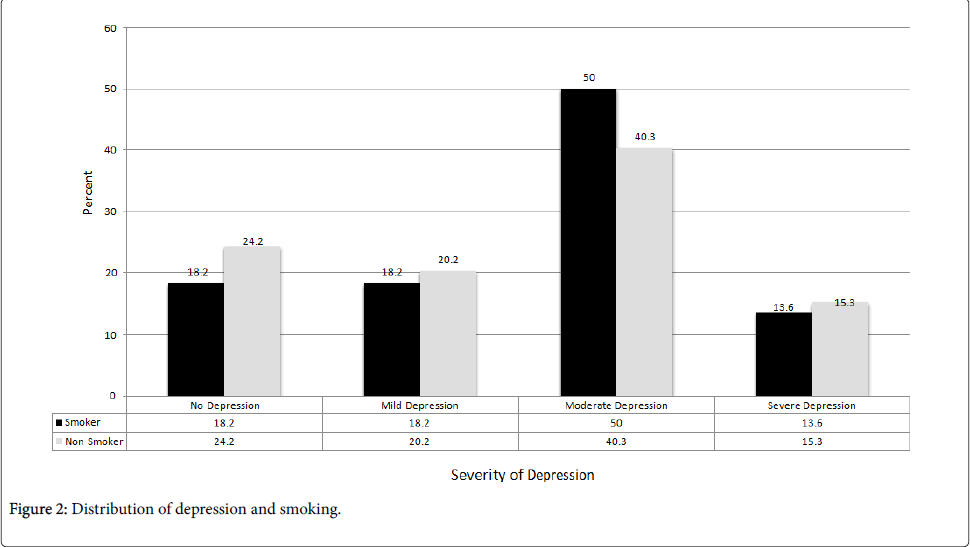
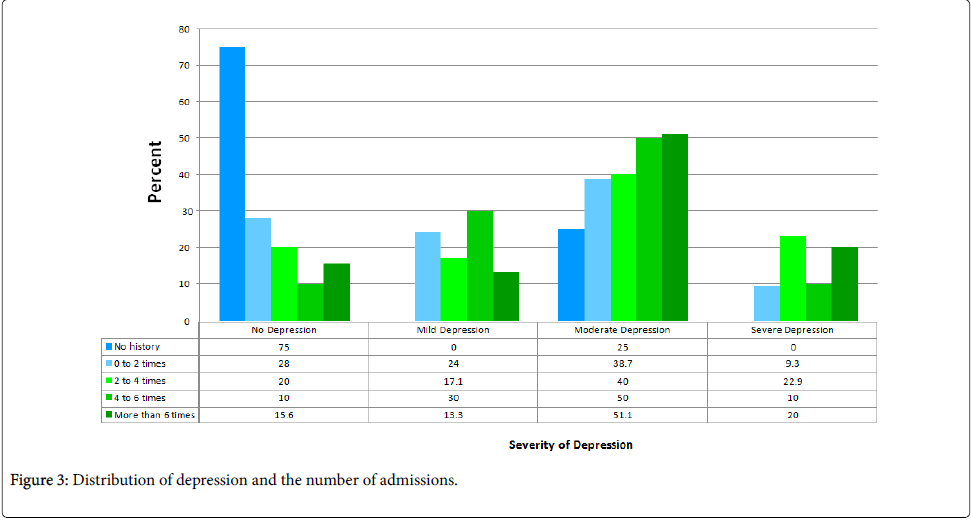
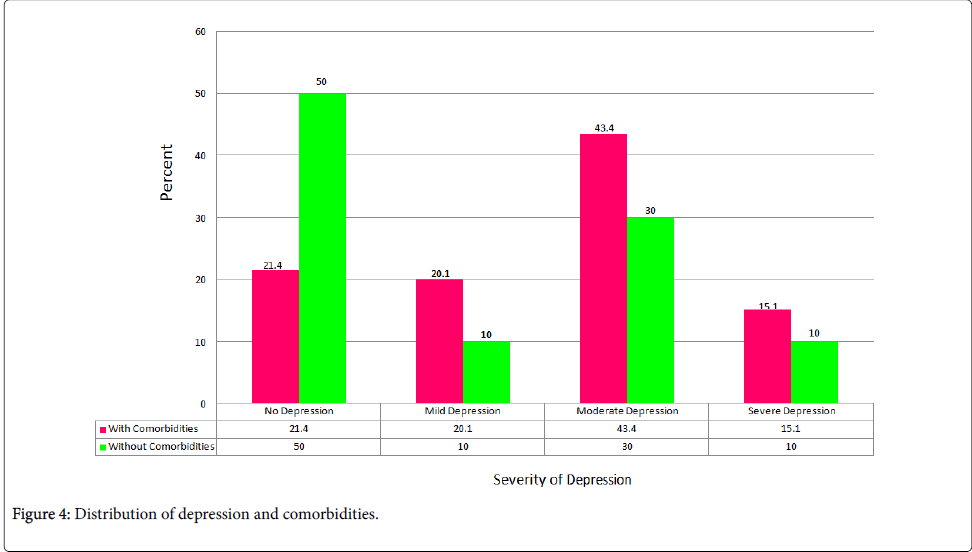
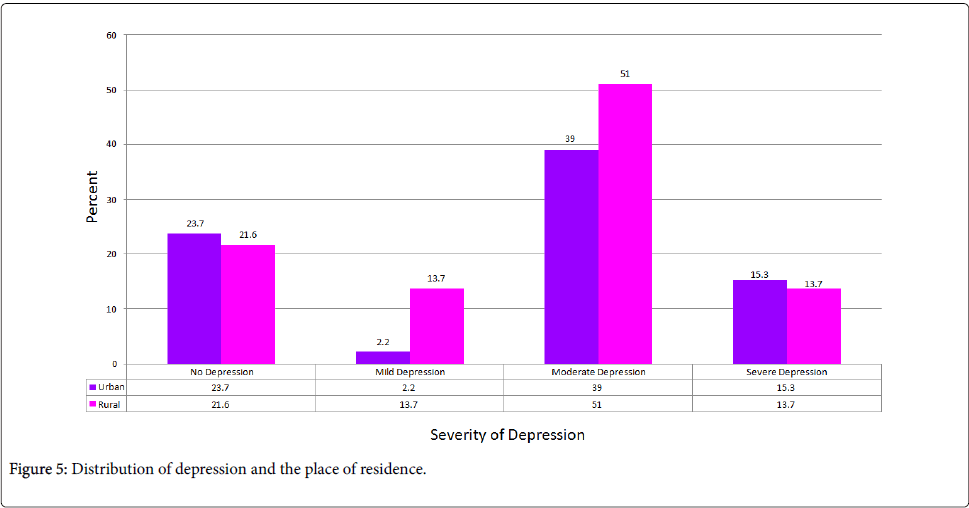
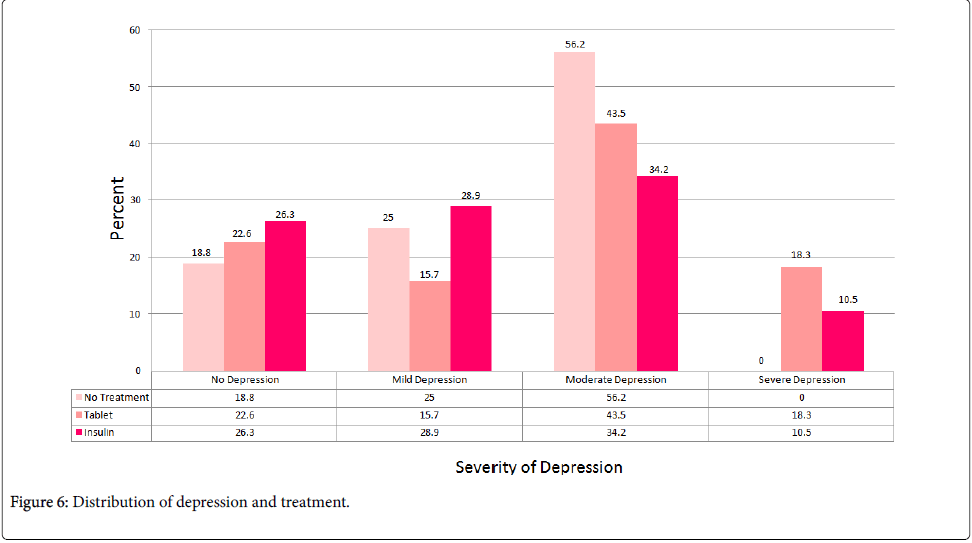
We could not find any significant correlations between depression and the age of the patients (p=0.385), HbA1C levels (p=0.58), duration of time since the diagnosis of diabetes mellitus (p=0.248), educational attainment levels (p=0.095), smoking (p=0.582), number of admissions (p=0.162), the method of controlling diabetes (p=0.218), the place of residence (p=0.459) and comorbidities (p=0.222) (Tables 1-3 and Figures 1-6).
| P value | F | Standard Deviation | Mean | Number | Severity of Depression |
|---|---|---|---|---|---|
| 0.385 | 1.02 | 11.48495 | 61.8718 | 39 | No depression |
| 11.36365 | 64.1515 | 33 | Mild Depression | ||
| 10.89514 | 62.2639 | 72 | Moderate Depression | ||
| 11.90056 | 58.96 | 25 | Severe Depression | ||
| 11.2759 | 62.0533 | 169 | Total |
Table 1: The distribution and severity of depression and age.
| P value | F | Standard Deviation | Mean | Number | Severity of Depression |
|---|---|---|---|---|---|
| 0.6 | 0.66 | 3.2859 | 8.781 | 39 | No Depression |
| 3.2122 | 9.574 | 33 | Mild Depression | ||
| 2.6905 | 8.745 | 72 | Moderate Depression | ||
| 2.8024 | 8.841 | 25 | Severe Depression | ||
| 8.929 | 169 | Total |
Table 2: The distribution and severity of depression and HbA1C.
| P value | F | Standard Deviation | Mean | Number | Severity of Depression |
|---|---|---|---|---|---|
| 0.25 | 1.39 | 1.4667 | 3.821 | 39 | No Depression |
| 1.7763 | 3.697 | 33 | Mild Depression | ||
| 1.5423 | 3.958 | 72 | Moderate Depression | ||
| 1.2288 | 4.48 | 25 | Severe Depression | ||
| 1.5384 | 3.953 | 169 | Total |
Table 3: The distribution and severity of depression and duration of time since the diagnosis of diabetes.
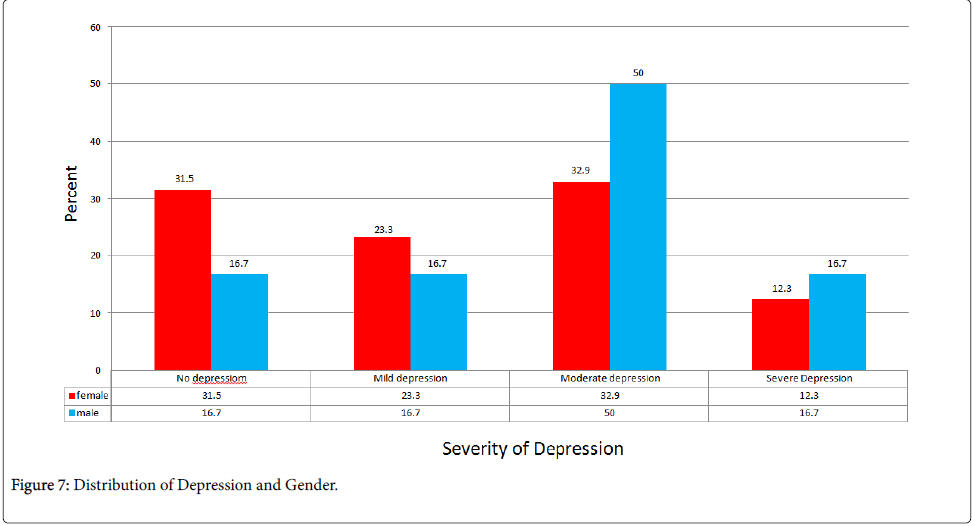
The distribution and severity of depression for gender: The prevalence of depression in diabetic women was significantly higher than in diabetic men. (83% vs. 67%) (p=0.041) (Figure 7).
Discussion
This study showed that depression is very common among patients who were admitted to the Shahid Rahimi Hospital of Khorramabad, Iran and the prevalence was 76.9%.
Most of the patients were not aware of their disease and had not consulted any doctors, and also during their admission, they had not consulted any psychiatrics. So we were facing many depressed diabetic patients, who had not received any treatments.
In other studies from other countries, the prevalence of depression in diabetic patients in Spain was 5.8% [11], Taiwan 10.6% [12], Malaysia 11.5% [13], Addis Ababa 13% [14], London 22% female and 13% male [15], Pakistan 14.7% [16], Brazil 18.6% [17], Jordan 19.7% [18], Bangladesh 30.5% female and 29% male [19], the Netherlands 38% female and 35% male [20], India 38.8% and 46.15% in two studies [21,22], and in Mexico 48.27% [23].
The prevalence of depression in diabetic patients in Iran was noticeably more than other countries. This prevalence in Rasht was 37.8% [24], Dr Shariaty Hospital clinic in Tehran and Iranian Diabetes Society 41.9% [25], Bandar Abbas 50% [26], Yazd 64% [27], Imam Khomeini Hospital in Tehran 70.7% [28], Semnan 71.6% [29], Firouzgar Hospital in Tehran 71.8% [30] and Uroumieh 77% [31].
The high prevalence of depression in this study may seem incredible, but unfortunately it is real and the factors like being admitted in the hospital didn’t have significant effects in this high prevalence.
In this study, we interviewed the patients face to face, and we made sure that the symptoms are reliable and had started at least 2 weeks earlier before admitting to the hospital. We ignored the symptoms that were started in the hospital.
Also, the results gained from other similar studies in Iran, confirmed our results, that was 64% in Yazd [27], 70.7% in Imam Khomeini Hospital in Tehran [28], 71.6% in Semnan [29], 71.8% in Firouzgar Hospital in Tehran [30] and 77% in Urmiah [31].
In Khoram abad, there isn’t any center to educate diabetic patients how care about themselves. Most of the patients were illiterate and they didn’t know how to get aware about diabetes, so most of them were complicated or had other comorbidities and also depression.
On the other hand, there were not any psychological consult about diabetic patients who were admitted to the hospital and many of them became missed, so they were not referred to the psychiatrist after discharge.
Because of all reasons above, the high prevalence of depression in diabetic patients in Shahid Rahimi hospital, is true and real.0
In this study, among all the factors mentioned above, only gender had a significant relationship with depression, and depression was higher in females.
The prevalence of depression in diabetic patients in this study was independent from many factors. Therefore, the control of depression will be very important and difficult and will need fundamental planning.
In addition to the conclusion above, this study had more conclusions, too:
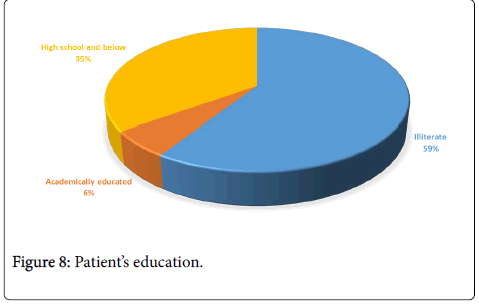
59.17% of the patients were illiterate and only 5.91% were academically educated.
So they are not able to study about diabetes, its treatment, control or its complications (Figure 8).
94% of the patients had other comorbidities (e.g. hypertension, hyperlipidemia, ischemic heart disease, diabetes complications, etc.), so they need serious medical care in contrast with patients who have no comorbidities (Figure 9).
60.94% of the patients had uncontrolled diabetes and HbA1C higher than 8 (Figure 10).
At the end of the study, we have recommended our suggestions to the internal medicine group of Shahid Rahimy Hospital and we have referred the depressed patients to the psychiatrist.
We make the following suggestions according to the conclusions above:
1. Psychiatric consultations for all diabetic patients who are admitted to hospitals.
2. Improvement of diabetic clinics in Khorramabad and other cities of Iran and the creation of diabetic files for each patient, and encouraging the patients for follow-up and regular visits with their doctors.
3. Development of training programs about diabetes for the diabetics.
4. Improving public knowledge.
References
- Egede LE, Ellis C (2010) Diabetes and depression: Global perspectives. Diabetes Research and Clinical Practice 87: 302-312.
- (2013) Diabetes and disability: impairments, activity limitations, participation restrictions and comorbidities. Australian Institute of Health and Welfare
- Frederick FT, Maharajh HD (2013) Prevalence of depression in type 2 diabetic patients in Trinidad and Tobago. West Indian Medical Journal 62: 7.
- Friis AM, Consedine NS, Johnson MH (2015) Does Kindness Matter? Diabetes, Depression, and Self-Compassion: A Selective Review and Research Agenda. Diabetes Spectrum 28: 252-257.
- Zhang X, Norris SL, Gregg EW, Cheng YJ, Beckles et al. (2005) Depressive symptoms and mortality among persons with and without diabetes.Am J Epidemiol 161: 652-660.
- Katon W, Fan MY, Unutzer J (2008) Depression and diabetes: a potentially lethal combination. J Gen InternMed 23: 1571-1575.
- Egede LE, Nietert PJ, Zheng D (2005) Depression and all-cause and coronary heart disease mortality among adults with and without diabetes. Diabetes Care 28: 1339-1345.
- (2002) Beck Depression Inventory and Mood/Depression Assessment Questionnaire.
- Ganji H (2015) the Beck depression inventory questionnaire. Ravansanji publish center.
- Lopez-de-AndrésA, Isabel Jiménez-Trujillo M, Hernández-Barrera V, de Miguel-Yanes JM, Méndez-Bailón M, et al. (2015) Trends in the Prevalence of Depression in Hospitalized Patients with Type 2 Diabetes in Spain: Analysis of Hospital Discharge Data from 2001 to 2011. PLoS One 10: e0117346.
- WuSF, Huang YC, Liang SY, Wang TJ, Lee MC, et al. (2011) Relationships among depression, anxiety, self-care behaviour and diabetes education difficulties in patients with type-2 diabetes: A cross-sectional questionnaire survey. Int J Nurs Stud48: 1376-1383.
- KaurG, Tee GH, Ariaratnam S, Krishnapillai AS, China K (2013) Depression, anxiety and stress symptoms among diabetics in Malaysia: a cross sectional study in an urban primary care setting. BMC FamPract14:69.
- Habtewold TD, Radie YT, Sharew NT (2015) Prevalence of Depression among Type 2 Diabetic Outpatients in Black Lion General Specialized Hospital, Addis Ababa, Ethiopia. Depression Research and Treatment.
- Bhattarai N,Charlton J, Rudisill C, Gulliford MC (2013) Prevalence of depression and utilization of health care in single and multiple morbidity: a population-based cohort study. Psychol Med43: 1423-1431.
- Zahid N, Asghar S, Claussen B, Hussain A (2008) Depression and diabetes in a rural community in Pakistan. Diabetes Res ClinPract79: 124-1 27.
- PapelbaumM, O Moreira R, Coutinho W, Kupfer R, Zagury L, et al. (2011) Depression, glycemic control and type 2 diabetes. DiabetoloMetabSyndr 3:2 6
- Al-Amer R, Sobeh M, Zayed A, Al-domi H (2011) Depression among adults with diabetes in Jordan: risk factors and relationship to blood sugar control. J Diabetes Complications 25: 247-252.
- Asghar S, Hussain A, Ali SMK, Khan AKA, Magnusson A (2007) Prevalence of depression and diabetes: a population-based study from rural Bangladesh. Diabet Med 24: 872-877.
- Pouwer F, Geelhoed-Duijvestijn PH, Tack CJ, Bazelmans E, Beekman AJ, et al. (2010) Prevalence of comorbid depression is high in out-patients with type 1 or type 2 diabetes mellitus. Results from three out-patients clinics in the Netherlands. DiabetMed 27: 217-224.
- Mathew CS,Dominic M,Isaac R,Jacob J (2012) Prevalence of depression in consecutive patients with type 2 diabetes mellitus of 5-year duration and its impact on glycemic control. Indian J Endocrinol Metab 16: 764-768.
- DasR, Singh O, Thakurta RG, Khandakar MR, Ali SN, et al. (2013) Prevalence of Depression in Patients with Type II Diabetes Mellitus and its Impact on Quality of Life. Indian J Psychol Med 35: 284-289.
- Tovilla-ZárateC, Juárez-Rojop I, Jimenez YP, Jiménez MA, Vázquez S, et al. (2012) Prevalence of Anxiety and Depression among Outpatients with Type 2 Diabetes in the Mexican Population. PLoS One7:e36887.
- KalantariS, Jafarinezhad A, Zohrevand B (2014) Association of depression with type 2 diabetes and relevant factors. Adv Biomed Res 3: 244.
- Larijani B (2004) Association of depression and diabetes in the doctor Shariati diabetes clinic and Iranian diabetes association.Journal of Diabetes and Metabolic Disorders 3: 62.
- Moaedi F (2015) Anxiety and depression in diabetic patient referred to Bandarabbas. diabetes clinic 18:65-71.
- Mazloumi S (2008) The prevalence of depression in patients with diabetes mellitus type 2 who referred to research center of Diabetes in Yazd (Iran) in 2008. Research Quarterly of hygienecollege of Yazd.
- Palizgir M, Bakhtiari M, Esteghamati A (2013) Association of Depression and Anxiety With Diabetes Mellitus Type 2 Concerning Some Sociological Factors. Iran Red Crescent Med J 15: 644-648.
- Behnam B (2005) Epidemiological features of depression in diabetic patients Insulin-independent group in Semnan Iran. Research in medicine 29: 45-49.
- Khamesh M (2007) Depression and Diabetes in Iranian Patients: A Comparative Study. Int J Psychiatry Med 37:81-86.
- Mahmoudi A (2008) A comparison between the Prevalence of depression and its associated factors in diabetic and nondiabetic people. Nursing and Midwifery training college magazine 6: 88-93.
Citation: Norouzi Z, Kaviani M, Tarrahi M, Jariani M, Abdollahian M, et al. (2016) The Prevalence of Depression in Patients with Diabetes Mellitus Type II in the Shahid Rahimi Hospital of Khorramabad, Iran. Epidemiology (Sunnyvale) 6:249. DOI: 10.4172/2161-1165.1000249
Copyright: © 2016 Norouzi Z, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 14509
- [From(publication date): 6-2016 - Aug 19, 2025]
- Breakdown by view type
- HTML page views: 13458
- PDF downloads: 1051