Treatment of Obstructive Sleep Apnea Syndrome through Orthodontics and Orthognathic Surgery: A Case Report with a Five Year Follow-Up
Received: 11-Jul-2016 / Accepted Date: 21-Jul-2016 / Published Date: 28-Jul-2016 DOI: 10.4172/2161-119X.1000250
Abstract
Introduction: Obstructive sleep apnea (OSA) results from the presence of abnormal soft and hard tissues in the upper airway, which cause the collapse of the oropharynx in the deeper stages of sleep. Different treatment modalities have been proposed for OSA, aiming to offer a better quality of life for the patients. Orthognathic surgery via maxillary-mandibular advancement (MMA) decreases the collapse of soft and hard tissue structures during sleep and has a high success rate. The facial and occlusal improvement, the enhancement on respiratory function and the less morbid postoperative period are some advantages responsible for the growing acceptance of this technique. Case report: This case reports a combination of orthodontic treatment and orthognathic surgery via MMA in a 51 year old man with OSA. The initial polysomnography showed an apnea-hypopnea index of 49.2 and arousal index of 21.7. Follow-up polysomnography performed 15 months after surgery revealed significant improvement. The apneahypopnea index decreased to 2.9 and the arousal index to 12.3. The patient reported significant improvements in life quality, sleep quality, and nasal breathing capacity, as well as a decrease in daytime sleepiness and snoring. Thus far, the patient has been under postoperative follow-up for 5 years and 6 months, without any complaints of breathing difficulties during the day or night. Conclusion: The combination of orthodontic and surgical treatment via MMA may be a favorable alternative treatment for improving the respiratory symptoms of patients with OSA and is highly indicated for patients with maxillary-mandibular discrepancies.
Keywords: Obstructive sleep apnea syndrome; Orthognathic surgery; Orthodontics
252264Introduction
Obstructive sleep apnea (OSA) is a disorder resulting from the presence of abnormal soft and hard tissues in the upper airway, which causes the collapse of the oropharynx in the deeper stages of sleep. OSA is also influenced by the body mass index [1]. The incidence of OSA in the general population is approximately 4%; its incidence peaks between the 4th and 5th decades of life and is 8 to 10 times more common in men than in women [2]. The chronicity of the syndrome causes low blood oxygen level, sleep fragmentation, snoring, fatigue, and hypersomnia. These can lead to work disability and behavioral changes, in addition to cardiorespiratory consequences [3]. Sleep disorders also affect public safety by causing an increase in the number of industrial and automobile accidents [4].
Different treatment modalities for OSA, including surgical or conservative treatment, have been proposed in the literature, seeking to offer a better quality of life for the patients. Continuous positive airway pressure (CPAP) is an immediate, fast, and conservative treatment for OSA; however, treatment adherence is low among patients [5]. The use of intraoral devices (IODs) is another conservative treatment option indicated in patients with mild OSA, with surgical contraindication, or refusing CPAP. However, this treatment may cause occlusal changes and temporomandibular disorders (TMDs), and also have lack of adherence [6]. Surgical techniques such as uvulopalatopharyngoplasty (UPP), hyoid suspension, and partial glossectomy yield limited results, and are mainly performed in cases of mild-to-moderate severity; moreover, they have a high rate of intraoperative and recurrent postoperative complications [7,8].
Orthognathic surgery via maxillary-mandibular advancement (MMA) may be indicated for moderate and severe OSA [9,10] and has 65-100% success rate [9]. Once this technique involves the advancement of both the jaws, permeability of the upper airway increases, decreasing the incidence of airway collapse during sleep. This advancement of hard tissues provide greater stability to the soft tissues of the oropharynx and nasopharynx regions, resolving OSA in 95% of the cases [8]. The preoperative orthodontic treatment that the patients with OSA undergo before MMA enables better surgical stability and better occlusal engagement, ensuring a more predictable treatment over time and aesthetic benefits. A meta-analysis performed by Hsieh et al. [10] showed that MMA produced average reduction rates of 61-92% on the apnea-hypopnea index and 82-92% on the respiratory disturbance index.
This case reports a combination of orthodontic treatment and orthognathic surgery via MMA in a 51 year old man with OSA.
Case Report
A 51 year old male patient, with a history of leukoderma and hypertension, sought dental treatment complaining of “poor sleep, snoring, fatigue, and difficulty in nasal breathing and chewing”.
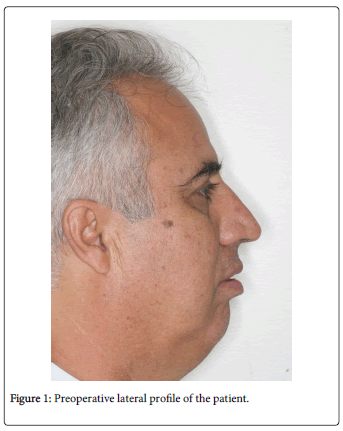
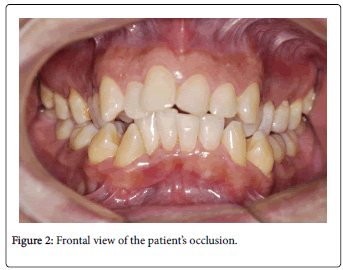
On facial analysis, dolichofacial pattern, non-passive lip seal, increased facial convexity, short chin-neck line, mandibular asymmetry, and nasal apex offset (Figure 1). On intraoral examination, Angle’s Class II malocclusion, overjet, severe upper and lower crowding, crossbite maxillary atresia, and deviation from the mean mandibular line (Figure 2).
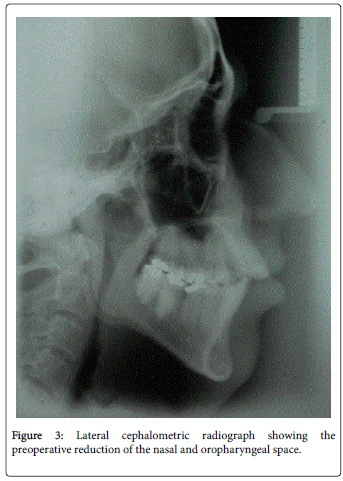
Radiographic examination revealed skeletal changes matching the patient’s facial deformity and severe posterior air space decrease in the nasal and oropharyngeal regions (Figure 3). The initial polysomnographic examination showed an apnea-hypopnea index of 49.2 and arousal index of 21.7. The outlined treatment plan included a combination of an orthodontic approach together with orthognathic surgery.
Alignment and leveling of the upper arch was performed using surgically assisted maxillary expansion, without the involvement of the nasal septum. After 5 days, maxillary expansion was initiated using a Haas-type dental-mucus-supported expander appliance. Maxillary expansion was carried out for 40 days postoperatively, until a magnitude of 10.5 mm was achieved. The expander was retained in the upper arch for 6 months and was removed after radiographic confirmation of bone formation in the intermaxillary suture region. After the removal of the expander, an acrylic containment apparatus was placed on the palatal concavity throughout the alignment and leveling process of the upper teeth.
The alignment and leveling of the lower arch was performed by extracting a lower first premolar on each side (elements 34 and 44) because of severe crowding in the arch and excessive labial inclination of the lower anterior teeth. Fifteen months after the removal of the expander, we started planning for the bimaxillary orthognathic surgery.
The orthognathic surgery was initiated by performing bilateral sagittal mandibular osteotomies, followed by mandibular advancement of 12 mm on the right side and 14 mm on the left. After surgically guided maxillary-mandibular fixation (MMF) with steel wires, a sagittal internal fixation plate of 2.0 mm thickness with 6 holes was placed on each side of the jaw for clamping and fixation of jaw segments.
Then, a 6 mm advancement mentoplasty was carried out with a decreased vertical height of 1 mm. Subsequently, total bilateral Le Fort I osteotomy (after the mobilization of the maxillary arch), a 10 mm advancement, and 3 mm superior repositioning were performed. During the surgical procedure, the intranasal region was accessed and removed 2/3 of the bilateral inferior turbinates. During the same procedure, a septoplasty in the palatal region of the nasal septum was performed.
The upper osteosynthesis used two 2.0 mm L mini-plates system for canine pillar region and two 1.5 mm L micro-plates system for zygomatic pillar region. Autogenous bone grafts were positioned in the space between the jaw segments. The MMF was removed when the patient was awake and repositioned 12 h after surgery by using intermaxillary elastic bands. The patient remained hospitalized for 36 h after the surgery.
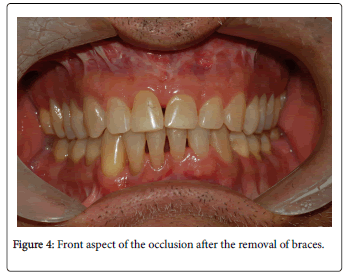
Semi-rigid MMF was used for 24 h in the first 21 days, and the elastic bands were removed 3 times a day only for the main meals. After this period, the patient started postoperative physiotherapy and concluded orthodontic treatment. The orthodontic procedure, including postoperative intercuspation, was completed in 10 months, and the patient reported respiratory and sleep improvements since the early postoperative period (Figure 4).
A follow-up polysomnography performed after 15 months showed significant improvement in OSA. The apnea-hypopnea index had decreased to 2.9 and the arousal index to 12.3. The patient reported a significant improvement in life quality, sleep quality, and nasal breathing capacity, as well as decreased daytime sleepiness and snoring. At 5 years and 6 months after surgery, the patient has no complaints of breathing difficulties at day or night (Figure 5).
Discussion
OSA is characterized by the total cessation of airflow for a period greater than or equal to 10 s [2], and the treatment goal is to reduce the frequency of occurrence of this obstruction. Several clinical symptoms allow the diagnosis of OSA and many of these symptoms could be observed in the current patient. Despite the typical clinical signs, polysomnography is considered the most reliable diagnostic technique to assess the achievement of OSA treatment goals [6].
Although various treatment modalities are available for OSA, some have disadvantages. Techniques such as CPAP and IOD depend on patient compliance and their efficacy might be compromised. CPAP has a precise indication and should be used by patients with moderate and severe OSA, as well as those who have no other immediate alternative treatment [5]. The long-term use of IODs has been associated with the appearance of malocclusions and TMDs [6].
Surgical techniques initially proposed for the treatment of OSA, such as UPP, hyoid suspension, and partial glossectomy, aim to manipulate soft tissues. These techniques are associated with postoperative morbidity, which discourages patients from opting these treatments. Postoperative complications and poor long-term effectiveness have sharply reduced the number of such surgical treatments for OSA [5-8].
Orthognathic surgery via MMA was initially first indicated for patients with clinical and cephalometric patter of maxillarymandibular retrusion. Secondly, after nasal or palatine surgery without significant improvement in OSA [8,10]. In some cases, MMA can provide up to 80% improvement in OSA, as indicated by the apneahypopnea post-treatment index (AHI)/disordered breathing index (DBI) [10]. The facial and occlusal improvement, the enhancement on respiratory function and the less morbid postoperative period are some advantages responsible for the growing acceptance of this technique by surgeons and patients.
On this case report, the patient achieved a significant improvement in OSA after surgical treatment, with a decreased apnea-hypopnea index (from 49.2 to 2.9) and arousal index (from 21.7 to 12.3), 15 months after surgery. At 5 years and 6 months after the surgery, the patient is very satisfied with the treatment outcomes and presents a stable occlusion, while reporting aesthetic satisfaction and the absence of any snoring and daytime sleepiness.
Conclusion
The combination of orthodontic and surgical treatment via MMA may be a favorable alternative treatment for improving the respiratory symptoms of patients with OSA and is highly indicated for patients with maxillary-mandibular discrepancies.
References
- Schendel SA, Broujerdi JA, Jacobson RL (2014) Three-dimensional upper-airwaychanges with maxillomandibular advancement for obstructive sleepapnea treatment. Am J OrthodDentofacialOrthop 146: 385-393.
- Wiegand L, Zwilich CW (1994) Obstructive Sleep Apnea. St. Louis, Mosby.
- Eckert DJ, Malhotra A, Jordan AS (2009) Mechanisms of apnea. ProgCardiovasc Dis 51: 313.
- Ferrara M, De Gennaro L (2001) How much sleep do we need? Sleep Med 5: 155-179.
- Weaver TE, Grunstein RR (2008) Adherence to continuous positive airway pressure therapy: The challenge to effective treatment. Proc Am ThoracSoc 5: 173.
- Dal-Fabbro C, Chaves CM Jr., Bittencourt LRA, Tufik S (2010) AvaliaçãoclÃnica e polissonográfica do aparelho BRD no tratamento da SÃndrome da ApneiaObstrutiva doSono. Dental Press J Orthod 15: 107-117.
- Riley RW, Powell NB, Guillelminault C (1993) Obstructive sleep apnea syndrome: a review of 306 consecutively treated surgical patients. Otolaryngol Head Neck Surg 108:117-125.
- Ronchi P, Novelli G, Colombo L, Valsecchi S, Oldani A, et al. (2010) Effectiveness of maxillo-mandibular advancement in obstructive sleep apnea patients with and withoutskeletal anomalies. Int J Oral MaxillofacSurg 39: 541–547.
- Waite PD, Wooten V, Lachner J, Guyette RF (1989) Maxillomandibular advancement surgery in 23 patients with obstructive sleep apnea syndrome. J Oral MaxillofacSurg 47:1256–1261.
- Hsieh YJ, Liao YF (2013) Effects of maxillomandibular advancement on the upper airway and surrounding structures in patients with obstructive sleep apnoea: a systematic review. Br J Oral MaxillofacSurg 51: 834-840.
Citation: Ayub OS, Ayub B, Ayub PV, Ravelli DB, Ribeiro PD, et al. (2016) Treatment of Obstructive Sleep Apnea Syndrome through Orthodontics and Orthognathic Surgery: A Case Report with a Five Year Follow-Up. Otolaryngol (Sunnyvale) 6:250. DOI: 10.4172/2161-119X.1000250
Copyright: © 2016 Ayub OS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 13676
- [From(publication date): 8-2016 - Jul 06, 2025]
- Breakdown by view type
- HTML page views: 12662
- PDF downloads: 1014