Research Article Open Access
Uncemented Arthroplasty for Hip Pain and Fracture after Metastatic Disease and Multiple Myeloma: Case Series, Exploratory Graphical Analysis and Bayesian Network Modeling
Sergio PS Meirelles*, Daniel CS Rebolledo, Luiz FM Correia, Andre M Baptista and Olavo P CamargoUniversity of Sao Paulo, School of Medicine, University of Sao Paulo, Department of Orthopedics and Traumatology, Sao Paulo, SP – Brazil.
- *Corresponding Author:
- Dr. Sergio PS Meirelles
University of Sao Paulo , School of Medicine, University of Sao Paulo
Department of Orthopedics and Traumatology, Rua Alves Guimaraes434
Sao Paulo, SP – Brazil, CEP 05410-000
Tel: 9561765303
E-mail: sergiopsmeirelles@gmail.com
Received Date: November 18, 2015; Accepted Date: December 10, 2015; Published Date: December 17, 2015
Citation: Meirelles SPS, Rebolledo DCS, Correia LFM, Baptista AM, Camargo OP (2015) Uncemented Arthroplasty for Hip Pain and Fracture after Metastatic Disease and Multiple Myeloma: Case Series, Exploratory Graphical Analysis and Bayesian Network Modeling. J Orthop Oncol 1:103. doi:10.4172/2472-016X.1000103
Copyright: © 2015 Meirelles SPS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Orthopedic Oncology
Abstract
We are not aware of previous cases series of uncemented arthroplasty for hip pain or fracture secondary to metastatic disease or multiple myeloma. Objective: To describe a case series using a combination of narrative, graphical exploratory analysis and Bayesian Network modeling. Methods: Case series of 34 patients undergoing uncemented and hybrid arthroplasty procedures secondary to hip pain or fracture secondary to metastatic disease or multiple myeloma. Case series is presented using a narrative following Kempen’s reporting guidelines, exploratory graphical analysis and Bayesian Network modeling with a structure based on expert opinion and parameters inferred from the data. Most common tumors included gastrointestinal, multiple myeloma and breast. A total of 26.3% (n = 5) of all of our procedures were performed secondary to fractures. Most devices were total (n = 16, 84.2%) rather than partial, uncemented (n = 12, 63.2%) rather than hybrid. Average time between surgery and first walk was 20 days, average length of stay of 13 days, with average patient survival of 589 days. Only one infection was reported. Uncemented and hybrid arthroplasty devices did not differ in relation to time to walk as well as length of stay in this sample. Conclusion: Our model should be used as the prior for the addition of subsequent patient samples, thus personalizing its recommendations to other patient populations.
Keywords
Bone tumors; Hip arthroplasty; Metastasis; Musculoskeletal; Bayesian networks
Introduction
The increase in survival among patients with metastatic disease to the bone or multiple myeloma has led to a subsequent increase in the incidence of imminent and pathologic fractures of the proximal femur in this population [1]. As a consequence, prophylactic and therapeutic orthopedic procedures are now performed more frequently [2]. Currently, cemented hip arthroplasty is considered the treatment of choice for such fractures [3,4]. However, such procedures are associated with an increased rate of adverse events [5,6], specially given the common occurrence of comorbid conditions [7]. In face of this high rate of complications it would be plausible to consider the use of uncemented arthroplasty, but to our knowledge there is no adequate evaluation of whether this would be a viable alternative.
Uncemented arthroplasty of the hip is a method widely used for patients with osteoporosis in the hip region, after hip fracture complications as well as in association with osteoarthritis [8]. Despite its higher cost, when compared with traditional cemented arthroplasty this procedure has been associated with lower operating time, more efficient medullary canal preparation and lower cardiopulmonary complication rates than when cement is used [9]. These features would be desirable among patients with metastatic disease, not only since recent series have demonstrated an overall survival improvement [10] but also in face of its safer profile.
In face of the potential advantages in this patient population, our study has two aims. First, to report a case series of uncemented arthroplasty cases for hip pain and fracture after metastatic disease and multiple myeloma, performed at the Cancer Institute of the State of SaoPaulo (Instituto do Câncer do Estado de SaoPaulo, ICESP) between 2010 and 2014. Second, we develop a Bayesian Network model to compare uncemented vs hybrid hip arthroplasty devices in relation to time until first walk and length of stay. We hypothesized that uncemented devices would outperform hybrid devices.
Methods
Our study was approved by the local Institutional Review Board, with participants providing informed consent prior to the initiation of our protocol. We also follow the case series reporting guidelines recommended by [11].
Patient information
All patients in our study underwent a total or partial hip arthroplasty with uncemented stems, hybrid procedures having a cemented cup. All procedures were performed and followed up at the Cancer Institute of the State of SaoPaulo (ICESP - Instituto do Cancer do Estado de SaoPaulo). Both orthopedic and clinical oncology group followed each patient in an integrated clinic.
All surgical procedures were indicated for (a) pathological fractures or (b) as a prophylactic treatment for metastatic lesions or multiple myeloma in the periacetabular or femoral regions. Information regarding gender, age, tumor diagnosis, medication history and radiotherapy treatment were all obtained through the electronic health record.
Our final sample was composed by 18 women and 16 men with an average of 67.1 years old (range 42-88). Primary tumors were distributed as: nine breast, one lung, eight prostate, seven gastrointestinal, five multiple myeloma and four of other types. From these patients, only two received preoperative radiotherapy, indicated for pain relief , and two received post-operative radiotherapy. A total of 14 patients undergoing total hip arthroplasty were admitted through the emergency room with a hip fracture. All remaining patients presented with hip pain or significant disability, with an accompanying radiograph and MRI (magnetic resonance imaging).
Diagnostic assessment
All patients were followed with radiographs and magnetic resonance of the corresponding hip to evaluate local progression, using a 3 to 6-month interval depending on patient compliance. Bone scans were used to evaluate new lesions. Based on imaging criteria, physical exam and pain rating scores, we then indicated osteosynthesis or hip arthroplasty on a case by case basis.
Therapeutic intervention
All patients included in this study underwent total or partial hip arthroplasty with a noncemented femoral stem. A total of 17 uncemented total arthroplasties, with 9 of them being indicated after a fracture. In addition, 9 patients received hybrid arthroplasties (cemented acetabulum and uncemented femoral stem), while 8 patients received partial arthroplasties. All procedures were performed through a lateral approach [12], with a 3.2 mm postoperative drain remaining until volume was below 50 ml in the past 24 hours. In all procedures, a cemented arthroplasty was available in the operating room in case of a change in surgical plan .
Preoperative heparin, at a dose of 40 mg subcutaneous injection once/day, was restricted to patients with a pathologic fracture and therefore unable to walk before surgery. All patients received intraoperative elastic band compression on their lower extremity, combined with postoperative enoxaparin, 40 mg subcutaneous once/ day for 3 weeks after the surgical procedure.
Outcome descriptive analysis
Outcomes quantitatively evaluated in this patient sample included length of stay (time between admission and discharge), time until death (time between first surgery and death, with death being identified through contact with family members), time between diagnosis and surgery, time until walking (time between surgery and first walk), postoperative infection, surgical debridement and antibiotic treatment .
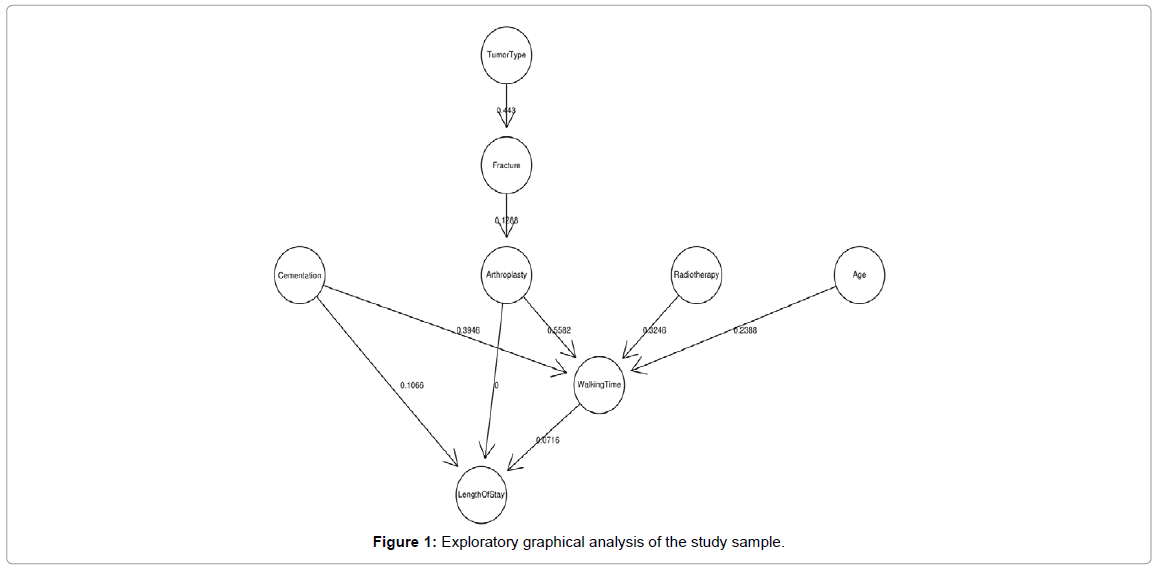
Causal and decision support modeling
We initiated the analysis through a descriptive graphical analysis, with numeric variables evaluated in relation to their statistical distribution and variance. Categorical variables were evaluated for their percentage. Variables with near zero categorical variance [13] either had their low-frequency category merged with other categories or the variable itself was not taken into consideration for further modeling. Causal modeling was conducted using a Bayesian Network [14,15].
Given the small sample for this study, we did not infer the structure from the data, but instead used a standardize protocol to extract the structure from clinical experts [16]. This structure was then followed by parameter estimation for each node connection. Expert elicitation was approached by first having the lead author (SM) generate a causal graph based on existing variables. This graph was later brought to discussion with co-authors using a variant of the Delphi method [17]. Although the final graph structure of choice was the one elicited from experts, we did attempt to infer the structure directly from the data using the following algorithms: grow-shrink, incremental association and its variants, hill-climbing, tabu search and restricted maximization, hill-climbing, tabu search and restricted maximization algorithms. For the score computation we used the following algorithms: Gaussian log-likelihood, Akaike Information Criterion, Bayesian Information Criterion, Bayesian Dirichlet equivalent and K2. An initial attempt to estimate structure using a hybrid model containing Gaussian and discrete variables, resulting in poor fit. This was therefore followed by a second model with discrete variables. All analyses were conducted using the blearn package [18] and the R statistical language [19]. Additional packages included the ggplot2 [20], tabplot [21], knitr [22], moonBook [23] and survival [24].
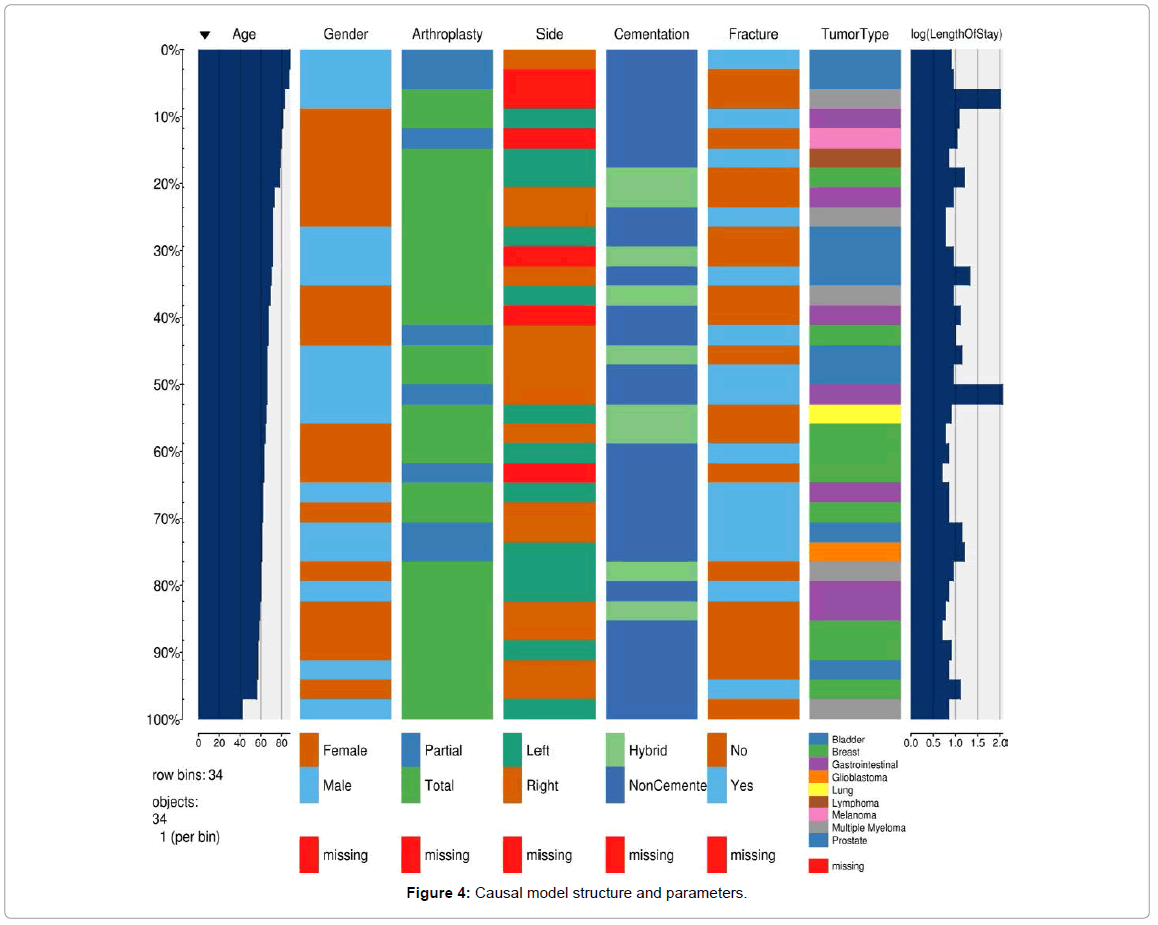
Descriptive statistics and graphical exploratory analysis
Our sample (Table 1) is composed by a slightly greater number of males, with an average age around 67 years of age. Diagnoses were highly heterogeneous, with the most prevalent tumor being breast cancer. The majority of patients underwent total and uncemented arthroplasty procedures, most not undergoing radiotherapy for pain control. Only one patient evolved with infection followed by debridement in this series. Given the sparcity of our data, we represent it through a single plot so that information on individual patients can be fully visualized (Figure 1).
| Particulars | Total (N=34) | p Value |
|---|---|---|
| Age | 67.1 A± 9.8 (42 - 88) | 0.466 |
| Female | 18 (52.9%) | 0.809 |
| Arthroplasty | 0.488 | |
| - Partial | 8 (23.5%) | |
| - Total | 26 (76.5%) | |
| Right Side | 15 (53.6%) | 0.030 |
| Cementation | 0.304 | |
| - Hybrid | 9 (26.5%) | |
| - NonCemented | 25 (73.5%) | |
| Fracture | 15 (44.1%) | 0.063 |
| TumorType | 0.903 | |
| - Bladder | 1 (2.9%) | |
| - Breast | 9 (26.5%) | |
| - Gastrointestinal | 7 (20.6%) | |
| - Glioblastoma | 1 (2.9%) | |
| - Lung | 1 (2.9%) | |
| - Lymphoma | 1 (2.9%) | |
| - Melanoma | 1 (2.9%) | |
| - Multiple Myeloma | 5 (14.7%) | |
| - Prostate | 8 (23.5%) | |
| Length ofStay | 14.3 ± 24.2 (42 - 114) | 0.954 |
| Death | 15 (44.1%) | 0.809 |
| TimeUntilDeath | 425.8 ± 388.5 (6 - 1419) | 0.019 |
| Radiotherapy | 1.000 | |
| - No | 30 (88.2%) | |
| - Post | 2 (5.9%) | |
| - Pre | 2 (5.9%) | |
| WalkingTime | 12.6 ± 19.1 (0 - 82) | 0.030 |
| Infection | 1 (2.9%) | 0.560 |
| SurgicalDebridement | 1 (2.9%) | 0.560 |
| AntibioticTreatment (Ciprofloxacin/Pseudomonas) | (2.9%) | 0.560 |
Table 1: Descriptive statistics for study sample.
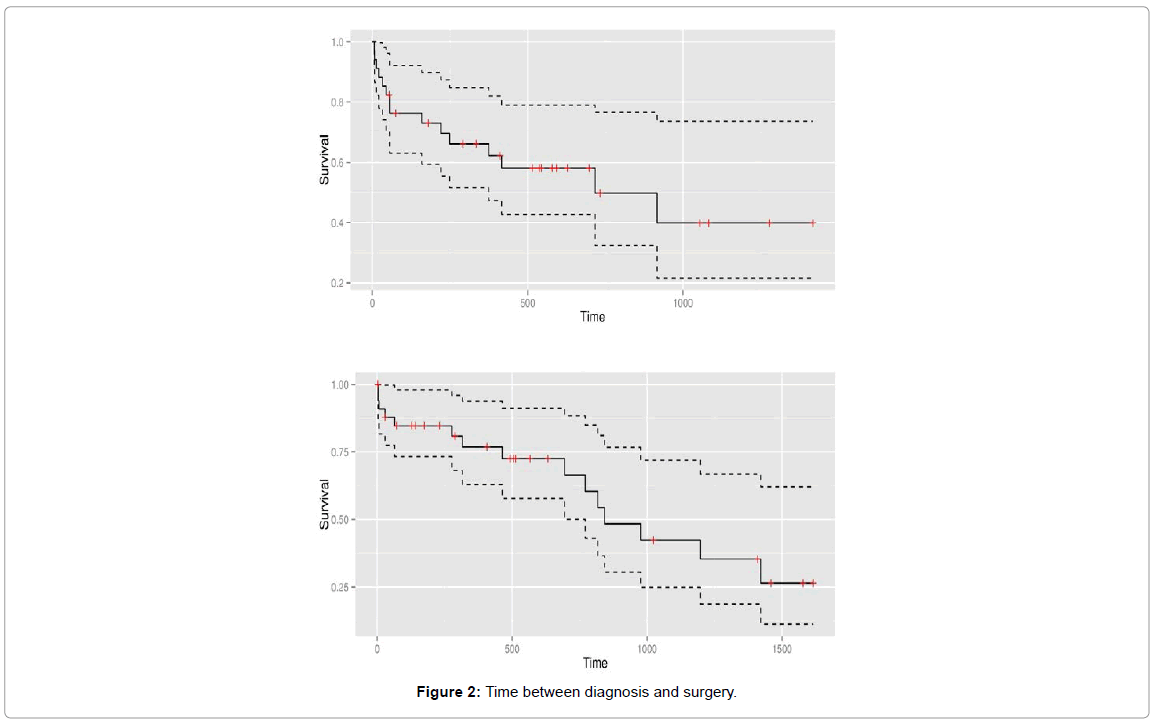
Surgical procedures largely occurred during the first two years after diagnosis, with only 4 patients operated on the first week after diagnosis and with surgeries being performed up to 4.4 years after diagnosis (Figure 2).
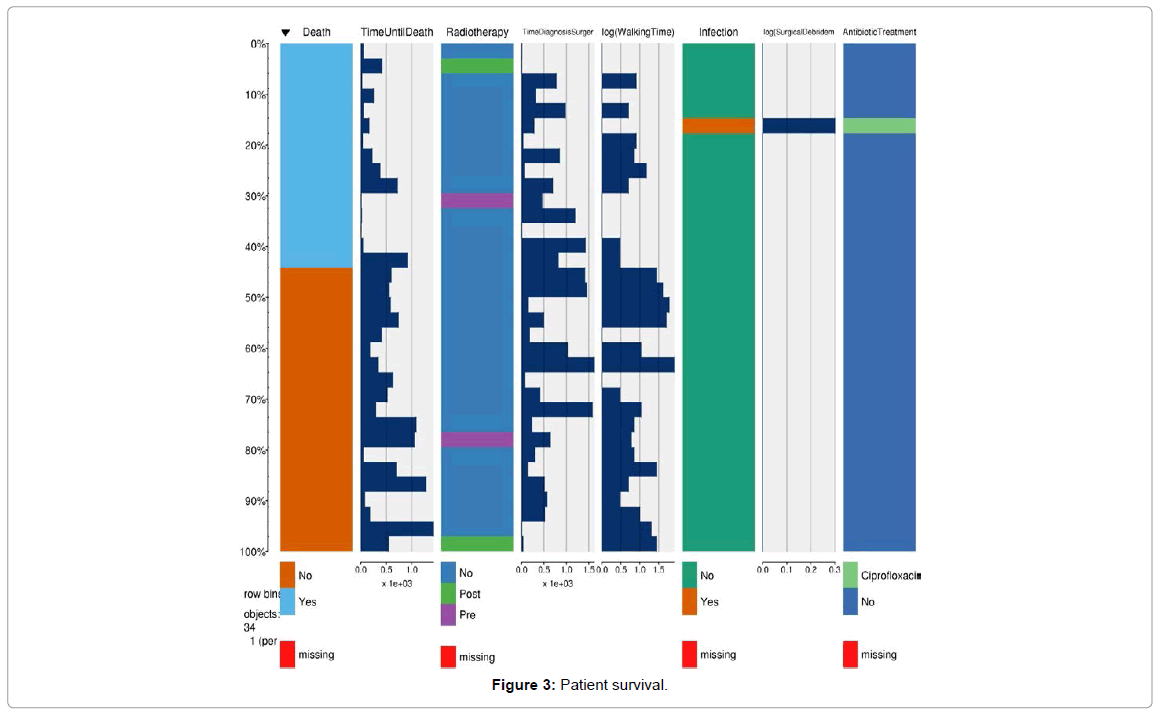
A total of 15 patients died during the course of the study, their mortality being distributed as displayed under (Figure 3).
Causal model
(Figure 4) represents our causal model where its structure was based on expert opinion and where parameters connecting different variables were inferred directly from the data. The causal model with probability parameters inferred from our data is displayed under (Figure 4). Of all associations, tumor type’s effect on the probability of fracture accounted for the largest conditional probability.
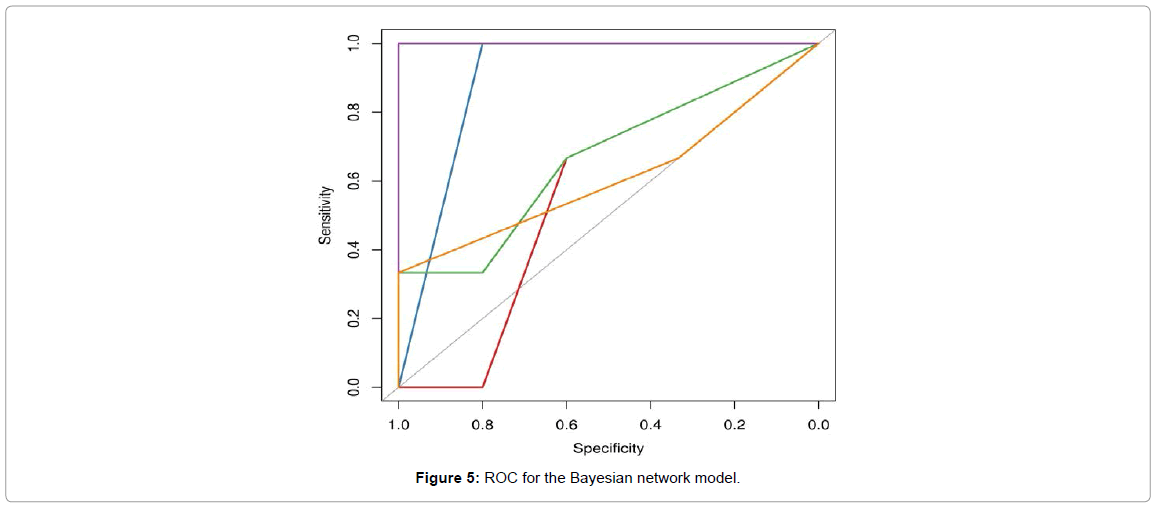
Predictive performance for our model achieved an area under the curve of 0.74, which can be considered as fair [25] (Figure 5).
Of central importance to our study, uncemented and hybrid arthroplasty devices did not differ in relation to time to walk as well as length of stay in this sample (Table 2).
| Sample | Total | Hybrid | Uncemented |
|---|---|---|---|
| [11.8,114] | 0.2454978 | 0.2787378 | 0.2330328 |
| [6,8] | 0.2530978 | 0.4870868 | 0.1653519 |
| [8,11.8] | 0.1196554 | 0.0568182 | 0.1432194 |
| [4,6] | 0.381749 | 0.1773573 | 0.4583959 |
a) Impact of Cementation on Length of Stay
| Sample | Total | Hybrid | Uncemented |
|---|---|---|---|
| [0,0.5] | 0.2283314 | 0.2787378 | 0.209429 |
| [0.5,5.5] | 0.1906461 | 0.2116829 | 0.1827573 |
| [5.5,13] | 0.2279387 | 0.2116829 | 0.2340346 |
| [13,82] | 0.3530838 | 0.2978963 | 0.3737791 |
b) Impact of Cementation on Time Until Walking
Table 2: Experiments comparing uncemented versus hybrid arthroplasty in relation to probability of walking and length of stay.
Discussion
To our knowledge, this is the first comprehensive case report, graphical exploratory analysis and causal modeling related to the use of uncemented arthroplasty for metastatic disease and multiple myeloma of the hip. We have both described our case series in relation to its clinical outcomes, as well as described a Bayesian Network model connecting several clinical factors to walking time and length of stay. Specifically, an experiment conducted within this model demonstrated that uncemented and hybrid arthroplasty devices did not differ in relation to time to walk as well as length of stay in this sample.
Date, cemented components are the traditional surgical technique when a hip arthroplasty is indicated for pain or fracture after metastatic or multiple myeloma in the hip area [26-28,3,4]. Previous studies have described the use of composite allograft with uncemented arthroplasty in the treatment of primary bone tumors [29], arguing that the cardiovascular risks associated with the use of cement could be avoided. This is also a strong argument in relation to patients with metastatic disease and multiple myeloma, as their overall health status is frequently compromised. An additional argument includes the increase in complexity of revision procedures if they might ever be needed. While in the past one could simply dismiss this point as survival tended to be poor, recent improvements in therapeutic management [10,30] now warrant reconstruction procedures where revision should be considered. Besides these former arguments, uncemented procedures use an interference or press fit mechanism, allowing for bone ingrowth and revascularization once weight bearing is initiated [31-33].
While our case series made use of a reporting guideline [11] to ensure that patient information can be more reliably interpreted by research and clinical peers, the narrative nature of case series does not allow for substantive evidence accumulation [34]. To decrease this limitation, we used a Bayesian Network model that combines expert knowledge in the form of its structure, while the relationship among different clinical factors is directly inferred from data [15]. Bayesian networks allow for a number of advantages while being used in the context of case series, namely, the ability to develop formal models with small sample sizes, good predictive performance, the possibility of adding data from other case series as well as the literature to generate cumulative evidence and, finally, the possibility of creating decision support tools such as Web applications so that model results can be accessed at the bedside [35,36].
Despite its novelty and significance, our study does have limitations.
First, our sample is acknowledged small. Despite its size, our models using Bayesian networks can be expanded through the addition of other case series, thus allowing for cumulative evidence rather remaining as an isolated narrative. Second, our model might not have accounted for all possible confounding factors affecting the association between uncemented arthroplasty and time to walk as well as length of stay, ultimately not substituting a randomized experiment [15]. While this is certainly a limitation, our model allowed us to establish an experiment comparing uncemented vs. hybrid arthroplasty procedures while having this experiment taking into account the values of all parent nodes, which assists in the decrease of confounding [37]. Last, given our limitations in terms of sample size, all of our model variables had to be categorized in order to have an acceptable predictive performance [15]. Although maintaining some of the clinical variables in its original numeric values would have provided a higher degree of information, future models with larger patient samples might use our estimates as Bayesian priors.
In sum, based on this case series with an accompanying Bayesian Network model, we have found that uncemented arthroplasty devices increase the conditional probability of both earlier time to walk as well as decreased length of stay among patients with metastatic disease or multiple myeloma in the hip area. Given the small sample in our study, we encourage other researchers to update our model results through their local data, thus not only increasing the body of evidence-based knowledge for this procedure but by also localizing its results to their population of interest.
References
- Chow E, Harris K, Fan G, Tsao M, Sze WM (2007) Palliative radiotherapy trials for bone metastases: a systematic review. J ClinOncol 25: 1423-1436.
- Swanson KC, Pritchard DJ, Sim FH (2000) Surgical treatment of metastatic disease of the femur. J Am AcadOrthopSurg 8: 56-65.
- Kiatisevi P, Sukunthanak B, Pakpianpairoj C, Liupolvanish P (2015) Functional outcome and complications following reconstruction for harrington class iI and iIIperiacetabular metastasis. World Journal of Surgical Oncology 13:4.
- Selek H, Baayarir K, Yildiz Y, Saaylik Y (2008) Cemented endoprosthetic replacement for metastatic bone disease in the proximal femur. J Arthroplasty 23: 112-117.
- Price SL, Farukhi MA, Jones KB, Aoki SK, Randall RL (2013) Complications of cemented long-stem hip arthroplasty in metastatic bone disease revisited. ClinOrthopRelat Res 471: 3303-3307.
- Thein R, Herman A, Chechik A, Liberman B (2012) Uncementedarthroplasty for metastatic disease of the hip: preliminary clinical experience. J Arthroplasty 27: 1658-1662.
- Li Shoumin, Hole wing, Rui Xia (2009) In the same line of hip and knee replacement mechanism is filled with bone cement 157Analysis of blood pressure and heart rate effects on tissue engineering of Clinical Rehabilitation China 13: 8381-8384.
- Post ZD (2013) Cemented versus cement less total hip arthroplasty: Is a hybrid the most cost effective? Journal of Comparative Effectiveness Research 2: 375-377.
- Yli-Kyyny T, Ojanperä J, Venesmaa P, Kettunen J, Miettinen H, et al. (2013) Perioperative complications after cemented or uncementedhemiarthroplasty in hip fracture patients. Scand J Surg 102: 124-128.
- Clément-Demange L, Clézardin P (2015) Emerging therapies in bone metastasis. CurrOpinPharmacol 22: 79-86.
- Kempen JH (2011) Appropriate use and reporting of uncontrolled case series in the medical literature. Am J Ophthalmol 151: 7-10.
- Hardinge K (1982) The direct lateral approach to the hip. J Bone Joint Surg Br 64: 17-19.
- Kuhn M, Johnson K (2013) Applied predictive modeling. Springer
- Pearl J (2014) Probabilistic reasoning in intelligent systems: Networks of plausible inference. Morgan Kaufmann
- Scutari M (2009) Learning bayesian networks with the bnlearn r package.
- Daly R, Shen Q, Aitken S (2011) Learningbayesian networks: Approaches and issues. The knowledge engineering review 26: 99-157.
- Creswell JW, Clark VLP (2007) Designing and conducting mixed methods research.
- Nagarajan R, Scutari M, Labre S (2013) Bayesian networks in r. Springer
- Dean CB, Nielsen JD (2007) Generalized linear mixed models: a review and some extensions. Lifetime Data Anal 13: 497-512.
- Wickham H (2009) Ggplot2: Elegant graphics for data analysis. Springer New York
- Tennekes M, de Jonge E (2014) Tree Colors: Color Schemes for Tree-Structured Data. IEEE Trans Vis Comput Graph 20: 2072-2081.
- Xie Y (2013) Knitr: A general-purpose package for dynamic report generation in r.
- Moon K-W (2015) MoonBook: Functions and datasets for the book by keon-woong moon.
- Therneau TM, Grambsch PM (2000) Modeling survival data: Extending the cox model. Springer Science & Business Media
- Krzanowski WJ, Hand DJ (2009) ROC curves for continuous data. CRC Press
- Felden A, Vaz G, Kreps Set al (2015) A Cemented acetabular component with a reinforcement cross provides excellent medium-term fixation in total hip arthroplasty after pelvic irradiation. Bone & Joint Journal 97-B: 177-184.
- Guo W, Sun X, Ji T, Tang XD (2009) [The surgical treatment of metastatic periacetabular tumors]. ZhonghuaWaiKeZaZhi 47: 1718-1721.
- Hertlein H, Schürmann M, Piltz S, Kauschke T, Lob G (1993) [Surgical treatment strategies in femoral metastases]. ZentralblChir 118: 532-538.
- Min L, Peng J, Duan H, Zhang W, Zhou Y, et al. (2014) Uncemented allograft-prosthetic composite reconstruction of the proximal femur. Indian J Orthop 48: 289-295.
- Gartrell BA, Saad F (2014) Managing bone metastases and reducing skeletal related events in prostate cancer. Nat Rev ClinOncol 11: 335-345.
- Wyatt M, Hooper G, Frampton C, Rothwell A (2014) Survival outcomes of cemented compared to uncemented stems in primary total hip replacement. World J Orthop 5: 591-596.
- Nieuwenhuijse MJ, Nelissen RG, Schoones JW, Sedrakyan A (2014) Appraisal of evidence base for introduction of new implants in hip and knee replacement: a systematic review of five widely used device technologies. BMJ 349: g5133.
- Kynaston-Pearson F, Ashmore A, Malak T (2014) Primary hip replacement prostheses and their evidence base: Systematic review of literature. British Journal of Sports Medicine 48:1198-1198.
- Rosner AL (2012) Evidence-based medicine: revisiting the pyramid of priorities. J BodywMovTher 16: 42-49.
- Friedman N, Nachman I, Pear D (1999) Learning bayesian network structure from massive datasets: The sparse candidate algorithm. In: Proceedings of the fifteenth conference on uncertainty in artificial intelligence. Morgan Kaufmann Publishers Inc20: 206-215
- Jensen FV (1996) An introduction to bayesian networks. UCL press London
- Fenton N, Neil M (2012) Risk assessment and decision analysis with bayesian networks. CRC Press
Relevant Topics
- 3D Printing in Limb-Sparing Surgery
- Adamantinoma
- Aneurysmal Bone Cysts
- Chondrosarcoma
- Chordomas
- Cryosurgery
- Enchondroma
- Ewing’s Sarcoma
- Fibrous Dysplasia
- Giant Cell Tumor of Bone
- Immunotherapy for Osteosarcoma
- Liquid Biopsy in Orthopedic Oncology
- Malignant Osteoid
- Metastatic Bone Cancer
- Molecular Profiling of Bone Tumors
- Multilobular Tumour of Bone
- Orthopaedic Oncology
- Osteocartilaginous Exostosis
- Osteochondrodysplasia
- Osteoma
- Osteonecrosis
- Osteosarcoma
- Primary Bone Tumors
- Sarcoma
- Secondary Bone Tumours
- Targeted Therapy in Bone Sarcomas
- Tumours of Bone
Recommended Journals
Article Tools
Article Usage
- Total views: 10925
- [From(publication date):
December-2015 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 9954
- PDF downloads : 971