Case Report Open Access
Unilateral Maxillary Lateral Incisor Agenesis with Mini Implant Prostheses: A Case Report
Azzaldeen A, Nikos K, Georgos C and Abu-Hussein M*
Department of Pediatric Dentistry, FICD 123Argus Street, 10441 Athens, Greece
- *Corresponding Author:
- Abu-Hussein M
MDent Sci (PaedDent), FICD 123Argus Street
10441 Athens, Greece
Tel: +65 6324 8802
E-mail: abuhusseinmuhamad@gmail.com
Received: December 18, 2015 Accepted: February 17, 2016 Published:March 15, 2016
Citation:Azzaldeen A, Nikos K, Georgos C, Abu-Hussein M (2016) Unilateral Maxillary Lateral Incisor Agenesis with Mini Implant Prostheses: A Case Report. Dent Implants Dentures 1:106. doi:10.4172/2572-4835.1000106
Copyright: © 2016 Abu-Hussein M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Dental Science and Medicine
Abstract
Orthodontic management for patients with single or bilateral congenitally missing permanent lateral incisors is a challenge to effective treatment planning. Over the last several decades, dentistry has focused on several treatment modalities for replacement of missing teeth. The two major alternative treatment options are orthodontic space closure or space opening forprosthetic replacements. For patients with high aesthetic expectations implants are one of the treatment of choices, especially when it comes to replacement of missing maxillary lateral incisors and mandibular incisors. Edentulous areas where the available bone is compromised to use conventional implants with 2.5 mm or more in diameter, narrow diameter implants with less than 2.5 mm diameter can be successfully used. This case report deals with managing a compromised situation in the region of maxillary lateral incisorusing a narrow diameter implant.
Keywords
Orthodontics; Correction of unilateral missing maxillary lateral incisors; Minimal invasive technique; Narrow diameter implant
Introduction
Many terms can be used to describe missing teeth. Anodontia is the complete absence of teeth; Oligodontia or partial anodontia means absence of six or more teeth; hypodontia denotes missing teeth, but usually less than six and often the size and shape of remaining teeth are altered as well, congenitally missing teeth or agenesis is defined as teeth that failed to develop or are not present at birth. Agenesis of any tooth can cause dental asymmetries, alignment difficulties, and arch length discrepancies but when the missing tooth is in the anterior region of the maxilla, the discrepancies can be quite noticeable [1,2].
The maxillary lateral incisor is the second most frequently missing tooth after the mandibular second premolar even though Muller et al. found that maxillary lateral incisors experience the most agenesis (not including third molars). Agenesis of the maxillary lateral incisor is also linked with anomalies and syndromes such as agenesis of other permanent teeth, microdontia of maxillary lateral incisors (peg laterals), palatally displaced canines and distal angulations of mandibular second premolars [3].
Absence of any tooth can cause treatment difficulties, but agenesis of the maxillary lateral incisor poses a unique set of restorative challenges. Because the maxillary lateral incisor is located in the esthetic zone, it is essential that bone height, papilla height, enamel color, and shape match the surrounding teeth. Clinicians attempt to maintain the proper anterior overbite, overjet and ideal interarch relationships of the canine teeth while creating enough space for a fixed partial denture or more commonly, an implant with a single crown restoration, but few treatment options are available for patients with agenesis of one or both maxillary lateral incisors. One option is to close the space(s) and restore the remaining teeth accordingly and the second is to open the space for a fixed partial denture or implant [4,5].
Kokich believes that canine substitution can be an excellent option for some patients, especially if they are Angle Class II with excessive overjet or are Class I with enough crowding in the mandibular arch to warrant extractions. The profile of the patients is another factor to consider. Protrusive faces are often more esthetically conducive for canine substitution than creating space for an implant by proclining the incisors and potentially making the lips more protrusive. The color and shape of the canines also needs to be taken into account before choosing this as the best option for treatment. If the canines are overly bulky or more yellow in hue than the central incisors, they may need bleaching, enameloplasty or restoration before treatment is complete [6-8].
One prosthetic option for replacing the missing lateral incisor is a resin bonded (Maryland) bridge, cantilevered bridge, or full-coverage bridge. Some benefits to these restorations include being less invasive than an implant, they can be completed in a growing individual, and there is more freedom with the space requirements when compared to the minimum of 6 mm required for an implant. Kokich reports that the resin bonded bridge is especially conservative since the preparations are only on the lingual of the incisors when compared to the full coverage abutments of a traditional bridge. A cantilevered bridge is the second most conservative option, followed by the fullcoverage bridge. Mobility of the abutment teeth, angulations of the incisors, gingival contours and occlusion are all factors to take into account before choosing one of these treatments for a patient [3,4,7,8].
Replacing the missing lateral incisor with an implant is another prosthetic alternative to closing the space. Kokich states that the smallest implant for this site is about 3.2 mm in diameter and recommends having at least 1 mm of bone between the implant and adjacent tooth. Therefore, the implant alone requires at least 5.2 mm of space and with the restoration of the crown at least 6 mm of space in required. Frequently, clinicians cannot maintain the proper occlusion and create a minimum of 6 mm of space for an implant. Kokich [7] advises the interproximal reduction of the central incisors, canines, or premolars to create enough space for an implant when this situation arises. More recently, he recommended only slenderizing teeth distal to the canines so as not to adversely affect anterior papillae in the esthetic zone [6-8].
Brook et al. have shown that some genes are implicated in the agenesis of teeth, including PAX9, MSX1 and AXIN2. The PAX9 gene is on chromosome with a controlling factor for dental development and mutations related to missing teeth. Brook et al. [9] measured the tooth sizes on maxillary and mandibular dental casts in the test group, 10 people with a known PAX9 mutation in one family and 10 people in a control group matched for sex, age and ethnicity, who were not related to the test group and did not have the PAX9 mutation. Differences in the test group with the mutation and hyperdontia were found; these teeth were significantly smaller than controls. Canines and first molars were least affected in the test group [10,11]. This contradicts Bailit’s theory that genetics mostly affects the first tooth in each group: the central incisor, canine, first premolar and molar [10,11]. Brook et al. [12] found that the second tooth in each group was more affected by the PAX9 mutation. The study concluded that the PAX9 mutation not only decreased tooth number, but also tooth’s size throughout the dentition. Large role in tooth size and agenesis with the PAX9 and MSX1 mutations; however some authors suspect that the local environment is important factor. EGF, EGFR, FGF-3 and FGF-4 are not shown to be linked to incisor-premolar agenesis, but it is possible that signaling factors early in embryologic development may contribute to agenesis [10]. Through the work of Pirinen et al. and Arte et al. it is evident that incisor premolar hypodontia is genetically inherited, with strong links to other dental anomalies such as palatally impacted canines. Incisor-premolar hypodontia is an autosomal dominant gene inheritance with incomplete penetrance [9,12].
The incidence of congenitally missing maxillary lateral incisors has been reported to range from between 1% and 2% 1 to as high as 5%. Maxillary lateral incisors are the most common congenitally missing teeth after upper and lower second premolars. Sex differences have been found to be negligible, with slightly more females affected as compared with males. Treatment options include orthodontic movement of cuspids into lateral incisor sites, prosthodontics restorations including fixed and removable prostheses and resinbonded retainers, and single tooth implants [10].
Implants do not require preparation of natural teeth and thus can be considered the most conservative approach. Orthodontic space opening may be necessary but on occasion can compromise esthetics, periodontal health, and function [1,2,4,5]. Parents and professionals must often decide at a child’s early age on how to cope with congenitally missing maxillary lateral incisors. Orthodontic treatment to create space for implants should not be initiated before the age of 13. This will avoid the potential for alveolar bone atrophy and the risk of relapse and subsequent retreatment [4,5].
The management of small restorative areas in the esthetic zone has posed significant problems for the implant and restorative team. The lack of bone available for the surgeon as well as the lack of restorative space available between the adjacent teeth makes tooth replacement with implants challenging for both the restorative dentist and the laboratory technician. In the past, patients with congenitally missing teeth or microdontia have been treated with resin-bonded bridges, removable retainers, or cantilever crowns to avoid the use of standarddiameter implants and prosthetics in this area [1,5].
The two common treatment options include orthodontic space opening for future restorations or orthodontic space closure utilizing the adjacent permanent canine teeth. With a paradigm shift in the patient expectations towards functional as well as esthetically appealing replacements for edentulous, the implant based oral rehabilitation has emerged as a sole winner in fulfilling all aspects of patient needs [1,2,4,5].
The orthodontist plays a key role in determining and establishing space requirements for patients with congenitally missing maxillary lateral incisors .However, the implant based treatment option in such patients requires an interactive and interdisciplinary management approach. This interdisciplinary approach may involve preprosthetic orthodontic treatment following consultations with an oral surgeon or periodontist and restorative dentist to ensure orthodontic alignment will facilitate the surgical, implant and restorative treatment.
Too often, surgeons attempting to place standard-diameter implants have forced the restorative team to manage these small dimensions with a lack of adequate prosthetics because of the size and diameter of the fixture head. In addition, surgical complications, such as contact with the adjacent roots, dehiscences of the labial plate, or the “show through” of the titanium through thin soft tissues, has posed a significant complication risk when attempting to use implants for tooth replacement in these situations.
Recently, manufacturers in the implant industry have offered a 3- mm diameter implant design to address these challenges. Most of the implants available in the 3-mm size have been one-piece or unibody implants, which often necessitate conventional tooth-preparation techniques by the restorative team as well as standard cord-impression techniques for indexing the restorative margins. With some systems, there is no need for preparation due to a cervical marginal collar that can be captured utilizing a snap-in impression transfer. This case report deals with managing a compromised situation in the region of maxillary lateral incisor using a narrow diameter implant.
Methods and Materials
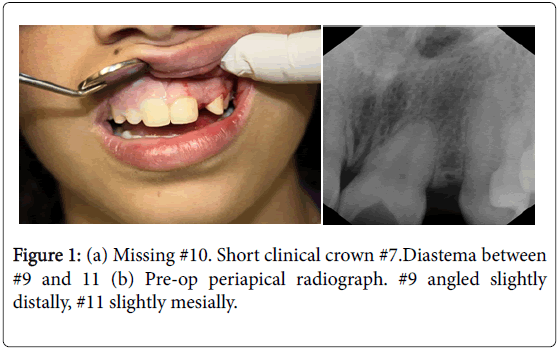
A 15 years old Arab girl was seen in private orthodontic clinic in Israel. She was an intelligent, college student, co-operative, and conscientious about her oral health and aesthetics. The patient was undergoing an active treatment of orthodontic treatment for past years, the aim of which was to close the residual space between her upper anterior teeth. Examination revealed good facial symmetry profile complicated by the presence of class I malocclusion. The patient was in permanent dentition with unilateral congenitally missing maxillary lateral incisors and retained deciduous lateral incisors. The maxillary arch presented with spacing between anterior teeth and in addition there was minor crowding of lower arch (Figure 1).
Objectives of the orthodontic treatment were:
• To provide adequate space for restoration of missing lateral incisors.
• Closure of residual spaces in the upper jaw.
• Correction of the crowding of lower anterior using edge wise brackets (non-extraction)
A multidisciplinary approach was discussed which included the patient, orthodontist, oral surgeon, restorative dentist and dental technician and following treatment plan was agreed upon as a team:
• To wait for a year to have complete bone healing prior to placement an implant.
• To restore the maxillary with lateral incisor implant supported crown.
The patient is a 17 yrs. old female with congenitally missing left lateral incisor. She just recently completed 2 years of orthodontic therapy. She was fitted with a retainer with 22 teeth on the retainer. Orthodontic treatment was only able to provide for 4 mm between the upper left central incisor and the upper left cuspid. The patient was referred to my office for consultation for implant therapy (Figure 2).
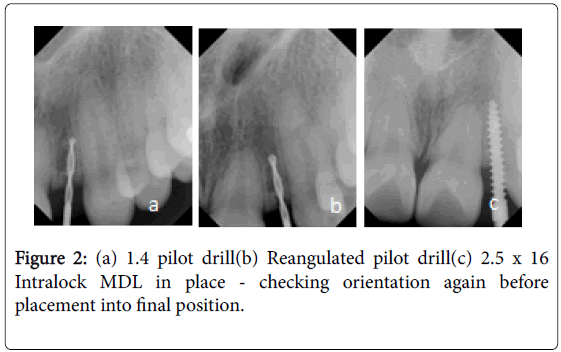
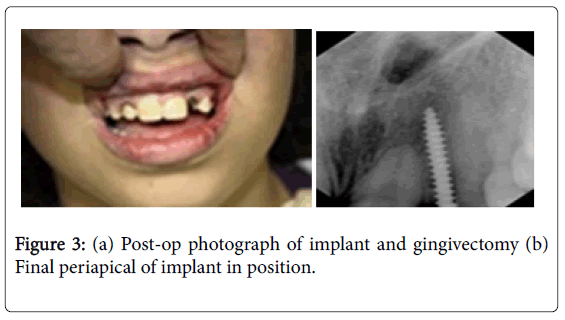
After preliminary investigations and thorough medical history patient was selected suitable for implant placement. The mesio-distal width of available alveolar bone between the maxillary right central incisor and maxillary right canine was 4 mm through the radiographic analysis. Single piece 2.5 × 16 mm implant was selected according to the bone width available. Prophylactic antibiotic regimen was started one day prior to the implant placement. After following the disinfection protocol, an infiltration of local anesthesia (Xylocaine 2% Adrenalin 1:200000) was administered in the labial vestibular region, in the region of missing tooth and a full thickness flap was raised. The labio-palatal alveolar bone diameter was confirmed as 4 mm using Osseo meter. Then pilot drill was made at implant site using 2 mm pilot drill to the required full depth and no sequential drill was used as the proposed implant diameter was 2.5 mm. By maintaining torque at 35N, using motor driven implant hand piece, implant was inserted into the prepared site. The flap was sutured back and hemostasis was achieved. The implant abutment was checked for any interference and is five day antibiotic protocol was followed. After the primary soft tissue closure around the implant impressions was recorded, temporary crown was fabricated and luted using non-eugenol cement. Nonfunctional immediate loading protocol was followed and all the contacts and interferences were removed (Figure 3).
Results
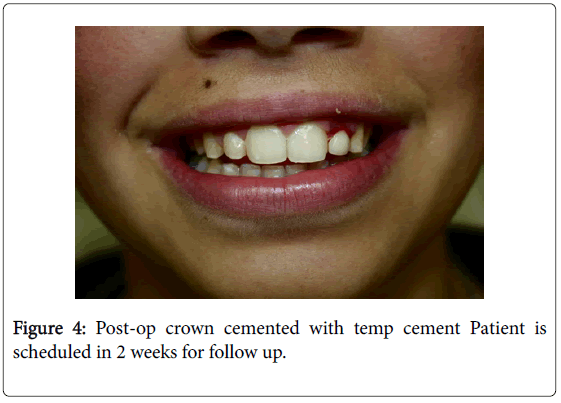
The implant was allowed to Osseo integrate for a period of 6 months, and a final impression was made using putty wash technique and a final prosthesis was fabricated. Prosthesis was tried in patient mouth and after checking the esthetics, the prosthesis was luted with GIC type 1 luting cement. Excellent esthetics and emergence profile were obtained through this technique (Figure 4).
Discussion
Small diameter implants provides advantages for the patients those normally would have preceded with a fixed or resin-bonded prosthesis with preparation and/or reduction of the adjacent natural dentition. Implants help in preserving the leftover alveolar ridge in the area of missing tooth and reduction of natural tooth structure as in the case of tooth supported fixed dentures can be avoided. In our case the mesiodistal diameter of alveolar bone is around 4 mm which is a difficult situation for placing the conventional implant [13].
Regular implant systems usually have 3.0 mm as their starting diameter. But 3.0 mm implant can't be placed in this situation due to lack of alveolar bone width. According to Carl E Mish, after placing the implant minimum of 1.0 mm bone should be present around the implant. As the available bone is only 4 mm, in this compromised mm situation, a 2.5 mm diameter implant is selected and successfully placed. So by placing narrow diameter implants we preserve not only the remaining alveolar bone from resorptions but also help in achieving optimal esthetics [14].
One of the most difficult areas for implant reconstruction has been the anterior maxilla, or what is known as the “esthetic zone”. Improved technology involving the surface of the implant body, abutment connection and prosthetic reconstruction of implants provided successful Osseo integration with raised possibility of totally mimicking the esthetics and function of natural teeth at this area [15].
In the early implantation the treatment protocol was to follow a two stage implantation to secure full Osseo integration before loading machined surfaced implants, where it achieved over 81% success rate in 15 years [5]. To advocating Load free Osseo integration, transitional implantation had been developed. Transitional implants were designed with smaller diameter of near 2 mm at various lengths. Mainly as abutments for interim over denture and loading were placed immediately after implantation until the definitive prosthesis were delivered. On histological and clinical evaluation have revealed that successful Osseo integration was observed in immediately loaded transitional implants [16].
Degidi et al. [17] did a 3 year randomized clinical trial on immediate versus one stage restoration of small diameter implants for a single missing maxillary lateral incisor and concluded that in the rehabilitation of a single missing maxillary lateral incisor, no statistically significant difference was assessed between immediately and one-stage restored small-diameter implants with regard to implant survival, mean marginal bone loss and probing depth. 3.0 mm diameter implants proved to be a predictable treatment option in their test and control groups when strict clinical protocol was followed.
Dong-Seok et al. [18] did a retrospective multicenter analysis of immediate provisionalization using one-piece narrow-diameter (3.0 mm) implants and concluded that for missing maxillary lateral incisors and mandibular incisors with compromised labio-lingual and mesiodistal available bone, one piece narrow diameter implants could be used successfully.
Anitha et al. [19] did a pilot study of mini implants as a treatment option for prosthetic rehabilitation of ridges with sub-optimal bone volume and concluded that failure rate of mini implants placed to replace single missing tooth was low and narrow diameter implants could be used in clinical situations in which available bone volumes did not permit placement of conventional implants.
Azfar et al. [20] used mini implants for replacement and immediate loading of two single-tooth restorations and concluded that mini implants were indicated for areas where the use of narrow diameter implants (3.0 mm) were contraindicated. Until long-term longitudinal clinical data on mini dental implants are available, their use should be limited to areas with potentially less occlusal load.
Reddy et al. [21] studied initial clinical efficacy of 3 mm implants immediately placed into function in conditions of limited spacing and concluded that in the areas of compromised bone spaces single piece immediately loaded narrow diameter implants could be used for predictable success.
Selection of the patients, correct surgical techniques, suitable implant design, complete understanding of the concepts of occlusion and the correct timing of implant placement are mandatory for optimum outcomes Bone growth with complete dent alveolar and facial growth should be completed before implant insertion. It takes place in males around the age of 21 while in females it occurs at age of 16 years. This coincides with the selected age range of the subjects included in this study. The females selected were older than 16 years while the males were between 21 and 23 years [22,23].
Another study using four to six Midi one-piece implants in the maxilla to support maxillary over dentures proved that it was ideal for most types of bone qualities, quantities and for atrophic ridges. The study reported that it is a reliable and cost effective treatment option that brings secure dentures within the reach of many patients, who are medically or financially compromised contributing to a higher degree of implant treatment acceptance due to less discomfort and generally shorter treatment times [24].
Different studies recommended that placement of the implants should be done after completing the orthodontic treatment and ending the retention period in order to achieve soft and hard tissue stabilization [25].
In a study by Van de et al. [26] on immediately loaded one-piece implants, only three of 12 implants were considered successful, showing a bone loss of 1.7 mm after two years of function.
The mean peri-implant marginal bone loss was 2.1 mm after one year. A mean bone loss of 1.6 mm after 12 months of loading of MDIs (3 mm) placed in the maxillary lateral and mandibular incisor area was observed, while 18% of the implants showed more than 3 mm of bone loss [27].
Sohn et al. [18] reported that mean marginal bone loss after 12 months of loading was 0.53 ± 0.37 mm [18]. In a study involving 115 one-piece implants, a failure rate of 5.2% due to excessive marginal bone loss was observed [28].
Proussaefs and Lozada [29] reported that the mean marginal bone loss of immediately loaded two-piece single-tooth implants was 1.05 mm after 12 months of loading.
In mesio-distal bone width compromised cases when all the factors are favorable, narrow diameter implant is the ideal choice for replacement of maxillary lateral incisor for achieving better esthetics as shown in our case. The long term success rate of these implants with various loading protocols has been assessed and the success rates of these implants were encouraging.
Conclusion
Planning for space management is best carried out before initiating orthodontic treatment. The time of implantation should be close to the end of orthodontic treatment. As opposed to starting orthodontic space closure early, orthodontic space opening before implantation should be started late. Finally, the importance of interdisciplinary team treatment planning is emphasized as a requirement for achieving optimal final esthetics.
References
- Abu-Hussein M, Abdulgani A, Watted N, Zahalka M (2015) Congenitally Missing Lateral Incisor with Orthodontics, Bone Grafting and Single-Tooth Implant: A Case Report. Journal of Dental and Medical Sciences 14: 124-130.
- Abu-Hussein M, Watted N, Abdulgani A, Bajali M (2014) Treatment of Patients With Congenitally Missing Lateral Incisors: Is an Interdisciplinary Task. 2: 53-68.
- Muller TP, Hill IN, Peterson AC, Blayney JR (1970) A survey of congenitally missing permanent teeth. J Am Dent Assoc 81:101-107.
- Abu-Hussein M, Abdulgani A, Watted N, Zahalka M (2015) Management of Congenitally Missing Lateral Incisors with Orthodontics and Single-Tooth Implants (A Case Report: After One Year Clinical Follow-Up) JMSCR 3: 5011-5019.
- Abu-Hussein M, Watted N,AbdulganiA, BorbélyB(2015) Modern Treatment for Congenitally Missing Teeth : A Multidisciplinary Approach. International Journal of Maxillofacial Research 1: 179-190.
- Kokich VO Jr, Kinzer GA (2005) Managing congenitally missing lateral incisors PartII: Tooth-supported restorations. J. EsthetRestor Dent 17:76-84.
- Kokich VG (2004) Maxillary lateral incisor implants: planning with the aid of orthodontics. J Oral Maxillofac Surg 62: 48-56.
- Kokich VO Jr, Kinzer GA (2005) Managing congenitally missing lateral incisors Part III: Single-tooth implants. J EsthetRestor Dent 17: 202-210.
- Brook AH, Elcock C, Aggarwal M, Lath DL, Russell JM, et al. (2008) Tooth dimensions in hypodontia with a known PAX9 mutation. Archives of Oral Biol 54: S57-62.
- Abu-Hussein M, Watted N, YehiaM, ProffP, Iraqi F, et al. (2015) Clinical Genetic Basis of Tooth Agenesis. Journal of Dental and Medical Sciences 14: 68-77.
- Vastardis H (2000) The genetics of human tooth agenesis: new discoveries for understanding dental anomalies. Am J OrthodDentofacialOrthop 117: 650-656.
- Brook AH, Elcock C, al-Sharood MH, McKeown HF, Khalaf K, et al. (2002) Further studies of a model of the etiology of anomalies of tooth number and size in humans. Connective Tissue Res 43: 289-295.
- Zinsli B, Sagesser T, Mericske E, Mericske- Stern R (2004) Clinical evaluation of small-diameter ITI implants: a prospective study. Int J Oral Maxillofac Implants. 19: 92-99.
- Misch CE, Perel ML, Wang HL, Sammartino G, Galindo-Moreno P, et al. (2008) Implant success, survival, and failure: the International Congress of Oral Implantologists (ICOI) Pisa Consensus Conference. Implant Dent 17: 5-15.
- Wheeler SL (2007) Implant complications in the esthetic zone. J Oral Maxillofac. Surg Suppl 1 65: 93-102.
- Proussaefs P (2003) Histologic evaluation of an immediately loaded titanium provisional implant retrieved after functioning for 18 months: A clinical report. J Prosthet Dent 89: 331-334.
- Degidi M, Nardi D, Piattelli A (2009). Immediate versus one-stage restoration of small-diameter implants for a single missing maxillary lateral incisor: a 3-year randomized clinical trial. Journal of Periodontology 80: 1393-1398.
- Sohn DS, Bae MS, Heo JU, Park JS, Yea SH, et al. (2011) Retrospective Multicenter Analysis of Immediate Provisionalization Using One-Piece Narrow- Diameter (3.0-mm) Implants. Int J Oral Maxillofac Implants 26: 163-168.
- Anitha B, Jumshad BM, Kathiresan R (2010) A Pilot Study of Mini Implants as a Treatment Option for Prosthetic Rehabilitation of Ridges with Sub-Optimal Bone Volume. J. Maxillofac. Oral Surg 9: 334-338.
- Azfar AS, Mark S, Mark G (2006) Use of mini implants for replacement and immediate loading of 2 single-tooth restorations: A Clinical Case Report. Journal of Oral Implantology 32: 82-86.
- Reddy MS, O'Neal SJ, Haigh S, Aponte-Wesson R, Geurs NC, et al. (2008) Initial clinical efficacy of 3-mm implants immediately placed into function in conditions of limited spacing. Int J Oral Maxillofac Implants 23: 281-288.
- Kokich, OV, Kinzer GA, Janakievski J (2011) Congenitally missing maxillary lateral incisors: Restorative replacement. American Journal of Orthodontics and Dentofacial Orthopedics 139: 435-445.
- Gumus HO, Hersek NI, Tuluoglu, Tasar F (2008) Management of Congenitally Missing Lateral Incisors with Orthodontics and Single-Tooth Implants: Two case Reports. Dental Research Journal 5: 37-40
- Zahran A, Darhous M, Sherien M, El-Nimr T, Mostafa B, et al. (2010) Evaluation of Conical Selftapping One-piece Implants for Immediate Loading of Maxillary Overdentures. Journal of American Science 6: 1774-1781.
- Krassnig M, Fickl S (2011) Congenitally missing lateral incisors- A comparison between restorative, implant, and orthodontic approaches. Dent Clin N Am 55: 283-299.
- Van de VT, Thevissen E, Persson GR, Johansson C, De Bruyn H, et al. (2009) Two-year outcome with Nobel Direct implants: a retrospective radiographic and microbiologic study in 10 patients. Clin Implant Dent Relat Res 11:183-193.
- Zembic A, Johannesen LH, Schou S, Malo P, Reichert T, et al. (2012) Immediately restored one-piece single-tooth implants with reduced diameter: one-year results of a multi-center study. Clin Oral Implants Res 23: 49-54.
- Ostman PO, Hellman M, Albrektsson T, Sennerby L (2007) Direct loading of Nobel Direct and Nobel Perfect one-piece implants: a 1-year prospective clinical and radiographic study. Clin Oral Implants Res 18: 409-418.
- Proussaefs P, Lozada J (2004) Immediate loading of hydroxyapatite-coated implants in the maxillary premolar area: three-year results of a pilot study. J Prosthet Dent 91: 228-233.
Relevant Topics
Recommended Journals
Article Tools
Article Usage
- Total views: 13913
- [From(publication date):
December-2016 - Aug 28, 2025] - Breakdown by view type
- HTML page views : 12698
- PDF downloads : 1215