Unusual Cases of Abscess Involving Head and Neck Region Caused by Burkholdreria Species
Received: 19-Nov-2019 / Accepted Date: 10-Dec-2019 / Published Date: 17-Dec-2019 DOI: 10.4172/2161-119X.1000389
Abstract
Burkholdreria cepacia complex refers to a group of aerobic, gram negative, non-fermenting bacilli that commonly causes opportunistic infections in patients with cystic fibrosis and chronic granulomatous disease. They thrive well in commonly used disinfectants, intra venous fluids and anti-septic solutions, thus have a tendency to cause outbreak in intensive care units and haematology wards. Sporadic cases occur very rarely and may manifest as skin & soft tissue infections, lung infections, urinary infections, peritonitis etc. Infections usually spreads very fast and it shows resistance to most of the commonly used antibiotics. Laboratory isolations is at times delayed and they are wrongly labelled as Pseudomonas species. All these factors make treatment more challenging. Here we present two cases of pyogenic infections involving head & neck region caused by Burkholderia species with two different clinical presentation in diabetic patients treated in our tertiary care institute in India.
Keywords: Burkholderia; Head & neck infections; Antibiotic resistance
Introduction
Burkholderia cepacia complex (Bcc) refers to a group of gram negative, lactose non-fermenting bacilli which are abundant in soil. They act as plant pathogens and also have anti-fungal, plant growth promoting and bio-remediation properties [1]. Human infection with Burkholderia species is very rare and is quite difficult to treat. They cause opportunistic infection in immune compromised patients, hospitalized patients and in patients with cystic fibrosis. They thrive well in commonly used intra venous fluids, disinfectants, ventilators, mattresses [2], etc. and hence have the tendency to cause hospital outbreaks in intensive care units or specialized wards. In the laboratory settings, many a times they are wrongly labelled as Pseudomonas species, which alters the treatment plan completely [3]. Here we present two cases of Burkholdreria infection with two different presentations, treated successfully in our tertiary care set up.
Case Reports
Case 1
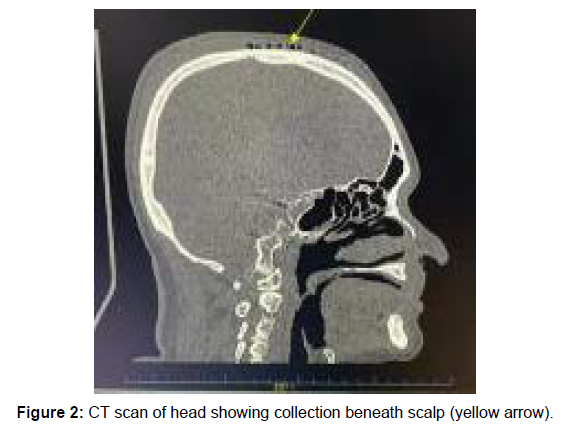
69 year old gentleman presented to our emergency department with complaints of pain and swelling in right side of cheek for 1 week duration. On eliciting further history, it was noted that patient developed pain and swelling in the cheek region around one week back. It was associated with fever. He consulted his physician and was diagnosed to have facial cellulitis with abscess formation. Incision and drainage (I&D) was done for the same. Even after I&D, he continued to have pain, and the swelling progressed to involve temporal region also. He has been taking medications for diabetes mellitus for the past 10 years. In view of rapid disease progression, he was referred to our tertiary care centre for further management. At presentation, he was febrile with elevated blood sugar levels. Detailed clinical examination revealed the presence of a large linear wound at the site of incision and drainage in right side cheek and there was copious pus discharge from the wound. It was associated with a large fluctuant, warm and tender swelling in temporal and zygomatic region. Rest of the head & neck examination was unremarkable. Imaging revealed the presence of inflammation with pus collection in facial soft tissue over right maxillary, zygomatic region extending up to temporal fossa (Figure 1). He was taken up for drainage of pus collection under general anaesthesia. Thorough wound wash and debridement was done through previous I&D site. Regular wound care was continued in the post-operative period. Culture & sensitivity of the pus revealed the presence Burkholdreria cepacia and it was resistant to most of the commonly used penicillin’s and cephalosporin. He was started on intra venous ceftazidime. Despite receiving regular wound care, with culture sensitive antibiotics and strict glycaemic control he did not show any significant improvement. Patient continued to have persistent pain, copious pus discharge, progressive swelling and inflammation. Inflammation extended further in the scalp region up to vertex in midline (Figure 2).
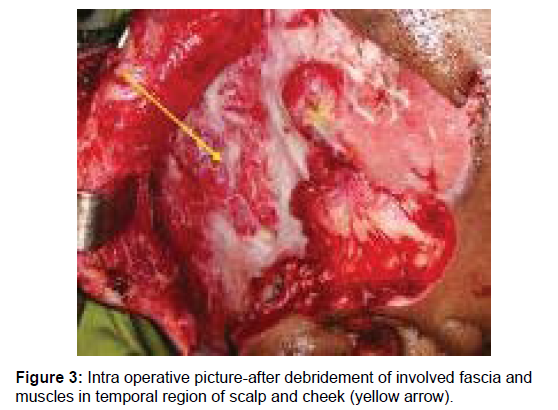
In view of disease progression, he was taken up for wound exploration and debridement again for the third time. To gain access to collection in scalp region, previous incision was extended up to temporal fossa. There was presence of copious pus discharge with diffuse inflammation eating away most of the fascia and fibres of temporalis, masseter, pterygoid and scalp muscles. Complete wound debridement was done after removing the diseased fascia and muscle fibre till bleeding margins (Figure 3). Wound was partially closed after a thorough wound wash with antibiotics. In the post-operative period, he continued to receive intra venous antibiotics with regular wound care. Now the antibiotic has been changed to a combination of intravenous meropenem and oral doxycycline. He started showing signs of recovery in the form of improved pain score with a well granulating wound. He was discharged with oral antibiotics. Secondary suturing of the wound was done four weeks after last surgery. He was kept on oral antibiotics (Trimethoprim-Sulfamethoxazole) for another 12 weeks. He did not develop any signs of recurrent infection during the follow up period.
Case 2
53 year old gentleman presented with complaints of pain and swelling over right side of neck for one month duration. It was associated with fever for the last one week. He has taken few courses of antibiotics for the problem. At presentation, he had tender and fluctuant swelling in the neck and imaging was suggestive of lymphadenitis with abscess formation. Pus collection was let out after doing incision and drainage at the abscess site. Pus and the lymph nodal tissue was sent for gram`s stain, ziehl neelsen stain, KOH mount, culture & sensitivity and histopathological analysis. Initial report did not reveal presence of any type of bacteria, Tuberculous bacilli or fungal hyphae. Culture report was initially negative and at 1 week later, it revealed growth of Burkholdreria pseudomallei. He was started on injection ceftazidime based on sensitivity pattern. Surgical wound healed completely with proper wound care, better glycaemic control and adequate antibiotic cover. Intravenous ceftazidime was continued for 2 weeks and later antibiotic was switched over to oral co-trimoxazole. He has been advised to continue oral antibiotics for 20 weeks period. Patient did not develop any recurrent infection or swelling during the follow up period.
Discussion
Burkholdreria cepacia complex refers to a group of aerobic, gram negative, non-fermenting bacilli that shows resistance to most of the commonly available antibiotics. It shows intrinsic resistance to many disinfectants, antiseptic solutions and antibiotics, which makes infection control particularly problematic [4]. In 1980`s they emerged as dreadful pathogen causing life threatening lung infections in patients with cystic fibrosis [5]. They commonly cause opportunistic infection in immunocompromised patients, hospitalized patients and in patients with cystic fibrosis. However, both the cases discussed here did not fit into this category. Incidences of isolated head & neck infection caused by Burkholdreria species in otherwise healthy patients is sparsely reported in literature [6].
They are facultative intra cellular pathogens capable of invading and replicating within both epithelial cells and macrophages. The virulence factors of Burkholdreria species includes; three type III secretion systems (T3SS), six type VI secretion systems (T6SS), multiple polysaccharide loci, and a number of secreted effectors. Poly saccharide capsule and lipopolysaccharides help them evade defence mechanism [7]. They are highly virulent, have tendency to spread very fast and becomes lethal at times. In both of our cases, Burkholdreria infection caused extensive tissue destruction involving skin, fascia, muscles and lymphnodes. There was rapid local spread despite under culture directed antibiotic cover, requiring repeated wound debridement.
B. cepacia complex isolates are frequently misidentified in the clinical laboratory by conventional manual biochemical or automated testing methods. Sometimes they are wrongly labelled as Pseudomonas species [3]. In our second case, it took us a week time to diagnose Bukholdreria species from the pus culture and sensitivity. Initially we suspected it to be a tuberculous lymphadenitis and investigations for tuberculosis like Ziehl-Neelsen staining for AFB, HPE of the excised node, Genexpert study was done and all of those reports came negative for tuberculosis. From the pus culture, we could not isolate any organism initially. We were able to identify Burkholdreria species only after 1 week time and antibiotic sensitivity a little later.
Burkholderia cepacia complex strains have been shown to be intrinsically resistant to aminoglycosides, first-and second-generation cephalosporins, polymyxins, and traditional antipseudomonal β-lactams, including piperacillin and ticarcillin [8,9]. The multipleantibiotic resistance of B. cepacia has been attributed to an impermeable selective outer membrane, an efflux pump mechanism, and/or the production of an inducible chromosomal beta-lactamase [10]. The organism is intrinsically resistant to most antibiotics, and even if individual strains show in vitro susceptibility to an antibiotic, there is little clinical response [11]. Even in our patients, culture directed antibiotic did not help in controlling infection during initial stage of treatment. Patient started showing response only after repeated debridement along with change of antibiotic combinations.
As such, recommended first-line therapy includes ceftazidime, TMP-SMX, minocycline, chloramphenicol, and meropenem or a combination of two or more of these agents in light of increasing resistance [12]. However, in vitro resistance to TMP-SMX and ceftazidime in Bcc isolates has been reported at approximately 10% to 40% and 30% to 40% cases respectively [13,14]. Data from synergy studies and the potential for emergence of resistance while on monotherapy suggest that therapy of serious B. cepacia complex infection should include at least two parenteral antimicrobial agents administered at standard doses. The choice of agents should be guided by results of in vitro susceptibility testing, and the duration of therapy should be based upon clinical assessment and microbiologic response [15]. For serious infection with susceptible strains, a two-drug combination of parenteral trimethoprimsulfamethoxazole (5 mg/kg trimethoprim component every 6-12 hr) plus a β-lactam (e.g., ceftazidime, piperacillin, meropenem) or a fluoroquinolone should be utilized. For serious infection with trimethoprim-sulfamethoxazole-resistant strains or sulfa drug allergy, combination therapy guided by in vitro susceptibility results should be administered [16].
Sporadic cases of Burkholdreria infection are quite uncommon. They should be kept as a differential diagnosis in patients with rapidly progressive infection, not showing much improvement with commonly prescribed drugs and also in situations where in culture reveals the presence of gram negative, non-fermenting bacilli. Burkholdreria infection once diagnosed must be treated with culture sensitive antibiotics and treatment must be continued for few months to achieve complete cure.
Conclusion
Sporadic cases of Burkholderia infection, especially in the head & neck region are quite uncommon. However, Burkholderia infection should be suspected in cases with rapidly spreading and progressive skin and soft tissue infection and in situations, where in the response to antibiotic therapy is very minimal. In laboratory diagnosis, Burkholderia species should not be confused with Pseudomonas species as both of them show similar features in culture and sensitivity testing. Long term oral antibiotic therapy is needed for complete disease eradication and to prevent disease recurrence.
Conflict of Interest
None.
References
- V Gautam, L Singhal, P Ray (2011) Burkholderia cepacia complex: Beyond pseudomonas and Acinetobacter. Indian J Med Microbiol 29: 4-12.
- Gautam V, Ray P, Vandamme P, Chatterjee SS, Das A, et al. (2009) Identification of lysine positive non-fermenting gram negative bacilli (Stenotrophomonas maltophilia and Burkholderia cepacia complex). Indian J Med Microbiol 27: 128–133.
- Vardi A, Sirigou A, Lalayanni C, Kachrimanidou M, Kaloyannidis P, et al. (2013) An outbreak of Burkholderia cepacia bacteremia in hospitalized hematology patients selectively affecting those with acute myeloid leukemia. Am J Infect Control 41: 312–316.
- Isles A, Maclusky I, Corey M, Gold R, Prober C, et al. (1984) Pseudomonas cepacia infection in cystic fibrosis: an emerging problem. J Pediatr 104: 206–210.
- Marioni G, Rinaldi R, Ottaviano G, Marchese-Ragona R, Savastano M, et al. (2006) Cervical necrotizing fasciitis: a novel clinical presentation of Burkholderia cepacia infection. J Infect 53: e219-e222.
- Moule MG, Spink N, Willcocks S, Lim J, Guerra-Assunção JA, et al. (2016) Characterization of New Virulence Factors Involved in the Intracellular Growth and Survival of Burkholderia. Inf Immun 84: 701-710.
- Zhou J, Chen Y, Tabibi S, Alba L, Garber E, et al. (2007) Antimicrobial susceptibility and synergy studies of Burkholderia cepacia complex isolated from patients with cystic fibrosis. Antimicrob Agents Chemother 51: 1085–1088.
- Lu D, Chang S, Chen Y, Luh K, Hsieh W (1997) In vitro activities of antimicrobial agents, alone and in combinations, against Burkholderia cepacia isolated from blood. Diagn Microbiol Infect Dis 28: 187–191.
- McGowan J (2006) Resistance in nonfermenting gram-negative bacteria: multidrug resistance to the maximum. Am J Med 119: S29–S37.
- Lewin C, Doherty C, Govan J (1993) In vitro activities of meropenem, PD127391 and PD 131628 Ceftazidime,Chloramphenicol,Co-Trimoxazole,andCiprofloxacinagainstPseudomonascepacia. Antimicrob Agents Chemother 37: 123-125.
- Nadim G, Chakhtoura E, Saade E, Wilson M, Perez F, Papp-Wallace K, Bonomo R.
- El Chakhtoura NG, Saade E, Wilson BM, Perez F, Papp-Wallace KM, et al. (2017) A 17-year nationwide study of Burkholderia cepacia complex bloodstream infections among patients in the United States Veterans Health Administration. Clin Infect Dis 65: 1253–1259.
- Papp-Wallace KM, Becka SA, Zeiser ET, Ohuchi N, Mojica MF, et al. (2017) Overcoming an extremely drug resistant (XDR) pathogen: avibactam restores susceptibility to ceftazidime for Burkholderia cepacia complex isolates from cystic fibrosis patients. ACS Infect Dis 3: 502–511.
- Chernish RN, Aaron SD (2003) Approach to resistant gram-negative bacterial pulmonary infections in patients with cystic fibrosis. Curr Opin Pulm Med 9: 509-515.
Citation: Pookamala S, Rajavel MAPS (2020) Unusual Cases of Abscess Involving Head and Neck Region Caused by Burkholdreria Species. Otolaryngol (Sunnyvale) 10: 389. DOI: 10.4172/2161-119X.1000389
Copyright: © 2020 Pookamala S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 2829
- [From(publication date): 0-2020 - Dec 07, 2025]
- Breakdown by view type
- HTML page views: 1989
- PDF downloads: 840