Research Article
Burden of Vascular Risk Factors on the Evolution of Alzheimer's Disease: A Longitudinal Observational Study
Takashi Yamazaki*, Daiki Takano and Ken NagataDepartment of Neurology, Yokohama General Hospital, Yokohama, Japan
- *Corresponding Author:
- Takashi Yamazaki
Department of Neurology
Yokohama General Hospital
2201-5 Kurogane-Cho, Aoba-Ku
Yokohama 225-0025, Japan
Tel: +81-45-902-0001
Fax: +81-45-903-3098
E-mail: yamazaki@yokoso.or.jp
Received date July 26, 2016; Accepted date August 02, 2016; Published date August 09, 2016
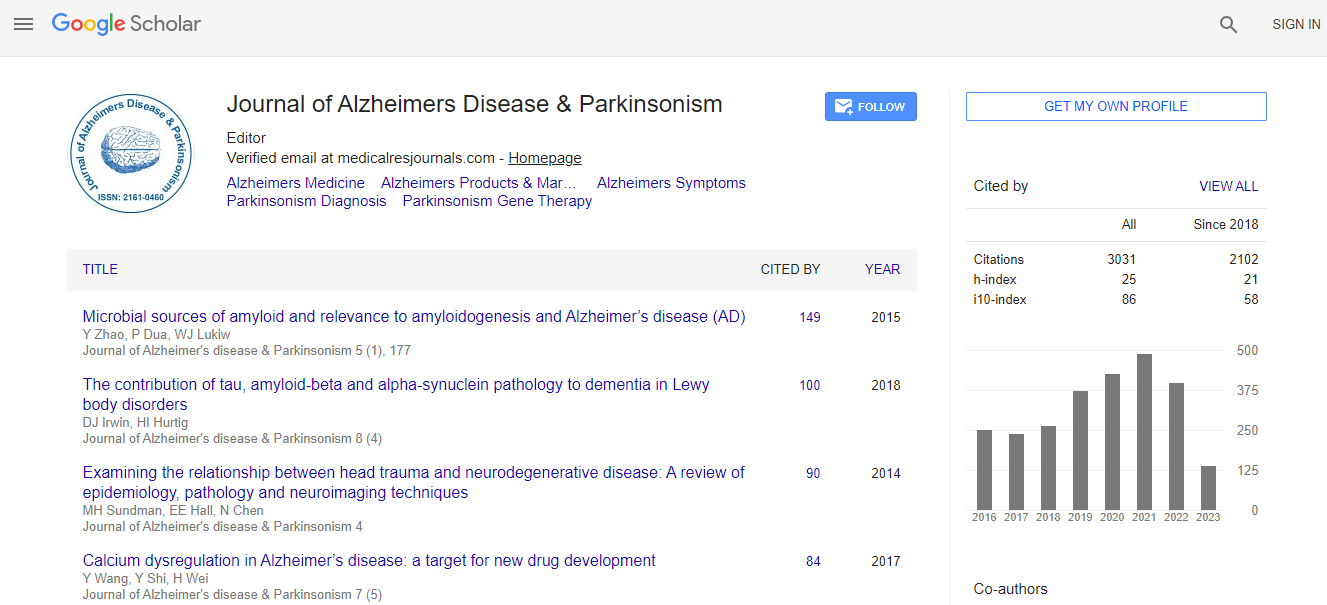
Citation: Yamazaki T, Takano D, Nagata K (2016) Burden of Vascular Risk Factors on the Evolution of Alzheimer’s Disease: A Longitudinal Observational Study. J Alzheimers Dis Parkinsonism 6:254. doi:10.4172/2161-0460.1000254
Copyright: © 2016 Yamazaki T, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Abstract
Background and objective: Although hypertension, diabetes, dyslipidemia and congestive heart failure are now considered as vascular risk factors (VRFs) for Alzheimer’s disease (AD), it is still unclear whether they influence the effect of treatment in elderly AD patients. To elucidate the influence of VRFs on the effect of cholinesterase inhibitors, we investigated the relationship between the presence of VRF and evolution of cognitive function in AD patients. Methods: The present study included 174 patients (59 men and 115 women) who were diagnosed as having probable AD according to the NINCDS-ADRDA criteria. All patients underwent laboratory examination, neuropsychological evaluation including Mini-Mental State Examination (MMSE), and assessment of VRFs at baseline, and were treated with donepezil hydrochloride for 2 years. The evolution of the MMSE score was evaluated by comparing the total MMSE score between the baseline and 2 year follow-up. Results: The MMSE score was improved or unchanged from the baseline in 52 patients (responders), whereas the MMSE score declined from baseline in 122 patients (non-responders). The responder status correlated negatively with baseline MMSE scores (p<0.01) and positively with body mass index (P<0.05). Although the response to donepezil did not correlate statistically with the presence of VRFs in the overall analysis, there was a tendency that there were less responders when there were more VRFs. Conclusion: The present study suggested that a good nutritional state in addition to the aggressive treatment of VRFs may slow down the progression of cognitive deterioration in elderly AD patients on donepezil.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi