Research Article
Worries about Alzheimer's Disease and Subjective Cognitive Decline in Proxies of AD Patients and Controls
Annika Philipps1, Stephan Müller1, Oliver Preische1,2 and Christoph Laske1,2*1Section for Dementia Research, Hertie Institute for Clinical Brain Research and Department of Psychiatry and Psychotherapy, University of Tübingen, Tübingen, Germany
2German Center for Neurodegenerative Diseases (DZNE), Tübingen, Germany
- *Corresponding Author:
- Christoph Laske
Section for Dementia Research
Department of Psychiatry and Psychotherapy
Calwer Street 14, D-72076 Tübingen, Germany
Tel: +4970712983444
E-mail: christoph.laske@med.uni-tuebingen.de
Received date: January 23, 2017; Accepted date: January 27, 2017; Published date: February 04, 2017
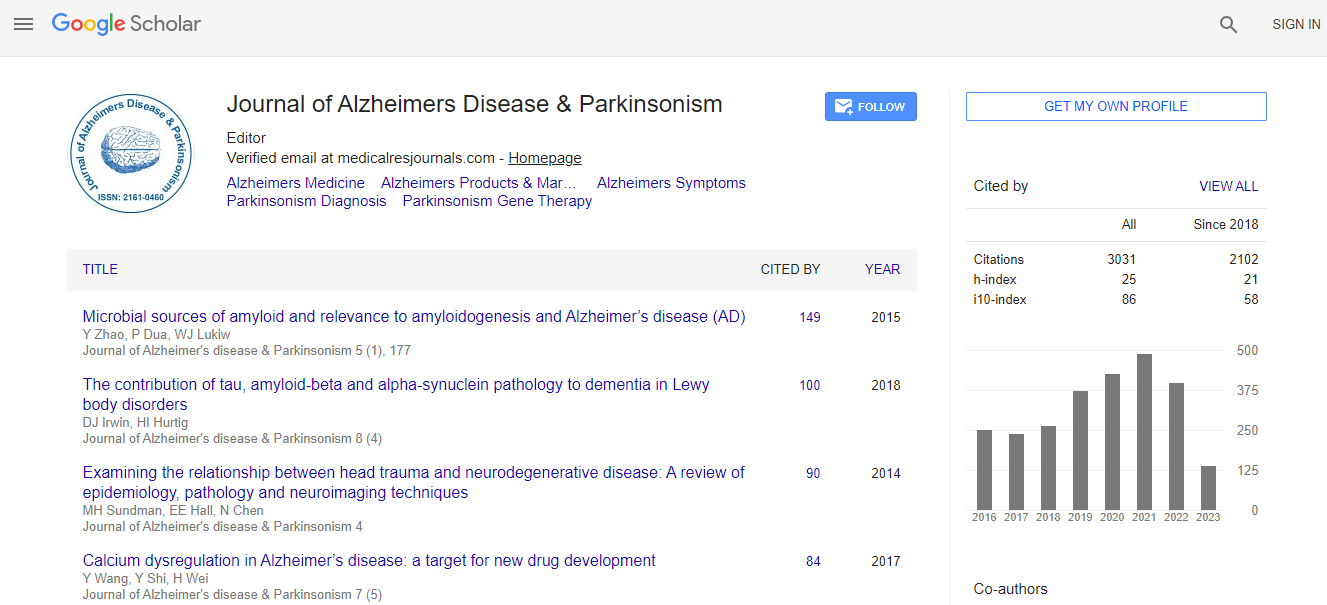
Citation: Philipps A, Müller S, Preische O, Laske C (2017) Worries about Alzheimer’s Disease and Subjective Cognitive Decline in Proxies of AD Patients and Controls. J Alzheimers Dis Parkinsonism 7:302. doi: 10.4172/2161-0460.1000302
Copyright: © 2017 Philipps A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Objective: Subjective Cognitive Decline (SCD) is actually considered to be associated with an increased likelihood of future cognitive impairment and dementia. Much less is known about worries concerning Alzheimer’s disease (AD Worry) and their relation to SCD, SCD with worries (SCD+Worry) and objective cognitive performance. Methods: We examined the prevalence and relation of AD Worry, SCD and SCD+Worry along with cognitive measures (MMSE, DemTect) among 100 proxies of persons with AD and 119 age-, gender- and education-matched controls. Results: AD Worry, SCD and SCD+Worry were frequently present in proxies of persons with AD (64.0%/47.0%/21.0%) and controls (62.2%/51.3%/16.8%) without significant group differences concerning frequency of occurrence and cognitive measures. Among proxies of AD patients, AD Worry occurred more frequently in first degree relatives (sons/daughters; 76.5%) compared to spouses (45.5%; p=0.002). Proxies with AD Worry were significantly younger (58.9 years) than proxies with SCD+Worry (67.4 years; p=0.012). Proxies of AD patients with feelings of burden reported SCD (55.6%) significantly more frequently than proxies without feelings of burden (32.4%; p=0.025). Controls with AD Worry reported SCD+Worry (23.0%) significantly more frequently compared to controls without AD Worry (6.7%; p=0.021). In line with the latter result, there was a significant positive correlation between AD Worry and SCD+Worry (r=0.211, p=0.021) in the control sample. Conclusion: AD Worry is a widespread phenomenon within the examined cohorts of proxies of AD patients and controls. It is not associated with objective cognitive impairment. However, the higher presence of SCD+Worry in those controls who reported AD Worry and the higher presence of AD Worry among sons and daughters of AD patients compared to spouses indicate that AD Worry could be an early indicator of future cognitive impairment. Longitudinal studies examining larger samples are needed to further elucidate the potential association between AD Worry, SCD and future cognitive decline.

 Spanish
Spanish  Chinese
Chinese  Russian
Russian  German
German  French
French  Japanese
Japanese  Portuguese
Portuguese  Hindi
Hindi