Research Article Open Access
A Bristle-Less Tooth Brush Reduces Recession Risk Over One Year Compared to a Conventional Soft Manual Brush
Tobias K Boehm*, Clara S Kim, Sam Chui and Josephine FrancCollege of Dental Medicine, Western University of Health Sciences, 309 E Second Street, Pomona, California, USA
- *Corresponding Author:
- Tobias K Boehm
College of Dental Medicine
Western University of Health Sciences
309 E Second Street, Pomona
California 91766, USA
Tel: (909) 706-3831
E-mail: tboehm@westernu.edu
Received Date: April 05, 2017; Accepted Date: June 16, 2017; Published Date: June 23, 2017
Citation: Boehm TK, Kim CS, Chui S, Franc J (2017) A Bristle-Less Tooth Brush Reduces Recession Risk Over One Year Compared to a Conventional Soft Manual Brush. J Oral Hyg Health 5: 221. doi: 10.4172/2332-0702.1000221
Copyright: © 2017 Boehm TK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Oral Hygiene & Health
Abstract
Background: Aggressive tooth brushing can contribute to gingival recession, and we tested in a randomized clinical trial if use of a bristle-less tooth brush results in less recession compared to using a conventional soft brush. Methods: We recruited 23 subjects with gingival recession who received regular periodontal maintenance care at Western University of Health Sciences Dental Center, and who did not exhibit signs of acute dental and systemic disease, occlusal discrepancies and para-functional habits. We randomly assigned these subjects to two groups, one using a soft nylon-bristled tooth brush, and the other group using the experimental tooth brush that contains a brush head with short, soft, rubbery cones. Both groups received regular periodontal maintenance and periodontal exams by blinded examiners every 3-4 months measuring probing depth, bleeding on probing, plaque indices. Tooth brush use was monitored by phone follow-up and measuring tooth brush wear of the tooth brushes assigned to subjects. Gingival recession was assessed clinically and through use of a stent on diagnostic casts obtained at each visit. Results: Average probing depths, plaque levels, and the number of sites with bleeding on probing did not change over one year. Subjects were compliant with tooth brush use as tooth brushes showed consistent wear patterns, but with much less tooth brush damage in the bristle-less brushes. There was a small, but statistically significant improvement of gingival recession (0.4 mm, p<0.01) at sites with gingival recession in the experimental tooth brush group compared to the control group and compared to baseline gingival level. Conclusion: A bristle-less brush appears to be more suitable in preventing additional gingival recession in patients with a history of aggressive tooth brushing.
Keywords
Gingival recession; Oral hygiene; Tooth brushing
Introduction
Gingival recession can lead to exposed unsightly root surfaces, crown margins and pose a risk of root caries and tooth sensitivity, as well as worsened oral hygiene from unfavorable, plaque-retentive gingival architecture [1]. Depending on the size, extent and location of the gingival recession defect, it may not be possible to reverse gingival recession completely, and even for suitable gingival defects, it requires soft tissue grafting which can cause significant postoperative pain and other complications. Therefore, prevention and management of gingival recession through eliminating contributing factors is desirable. Gingival recession can be caused by periodontal diseases, anatomic factors or physical injury [2]. Aggressive brushing techniques using a hard tooth brush is thought to repeatedly injure the gingival margin leading to gingival recession [3-6], although some have expressed doubt about this association [7]. It appears that the brushing technique matters less than tooth brush characteristics as in a study on dental students using an atraumatic brushing technique did not prevent further recession [8].
With tooth brushes, several characteristics may contribute to their potential in causing gingival recession: the type of tooth brush, tooth brush hardness, design of individual bristles and bristle arrangement and abrasiveness of the dentifrice used with the brush.
Hard tooth brushes are stiff enough to remove cervical enamel weakened by acidic beverages, leading to a wedge-shaped defect that prevents continued gingival attachment [9]. Hard tooth brush bristles are also more likely to stab and abrade gingival tissue [10,11], and contribute to connective tissue loss that undermines the gingival margin, leading to gingival recession [12]. Therefore, soft brushes are usually recommended for patients with gingival recession, along with a gentle dentifrice, as abrasive dentifrices can contribute to gingival recession development [13].
For bristle properties, neither bristle arrangement pattern [14] or bristle shape [15] seem to influence recession development. However, the material may be important as nylon bristles compared to bristles made from other materials produced the most gingival damage in a dog model [16].
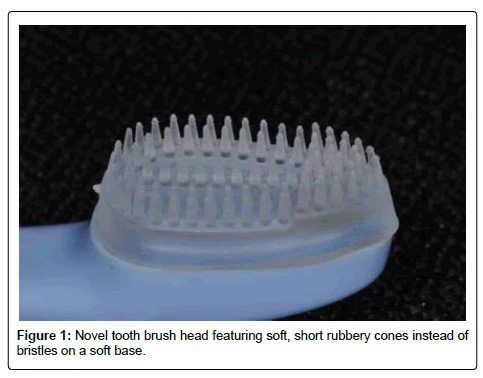
Recently, researchers demonstrated that an electric tooth brush designed for gentle plaque removal is more likely to prevent gingival recession [17]. Therefore it seems that gingival recession caused by aggressive tooth brushing may be prevented if patients are given a very soft tooth brush that can be used in a simple and gentle way for oral hygiene, as it will allow gingiva to recover once the constant trauma from a tooth brush is eliminated [18]. In this study we tested if a novel tooth brush containing a head made of soft, short rubbery cones was more effective in preventing gingival recession over time than a tooth brush with soft nylon bristles in periodontal maintenance patients.
Materials and Methods
Trial design
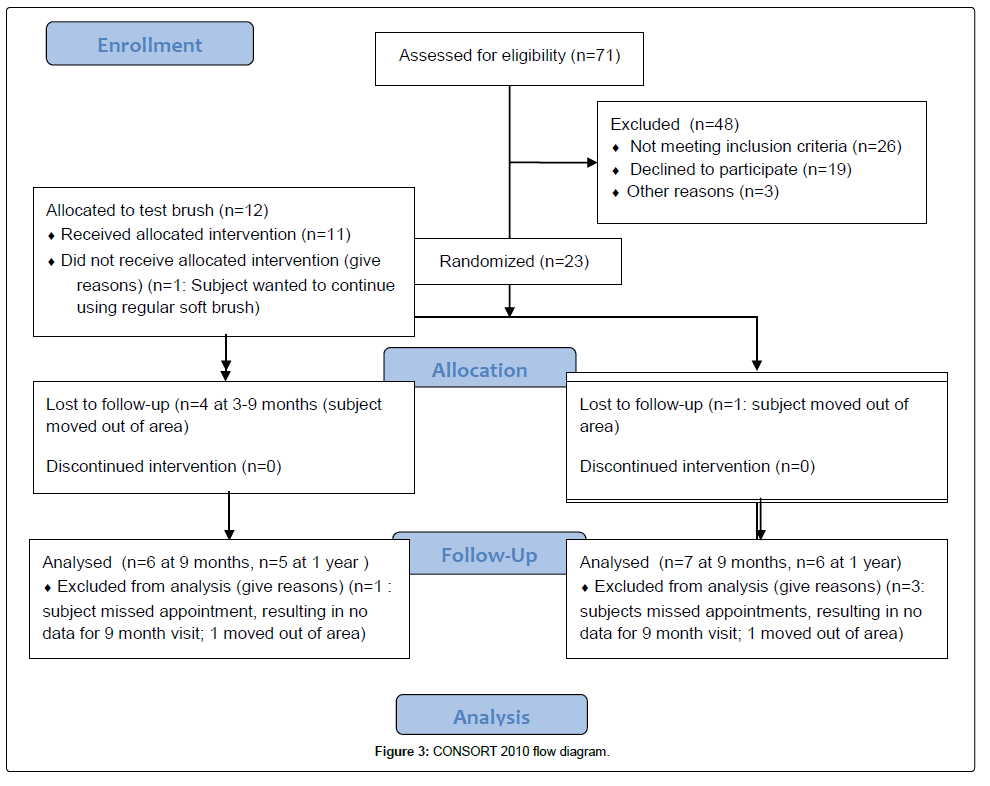
This was a single-blinded randomized parallel group clinical trial. We report the data following the CONSORT (Consolidated Standards of Reporting Trials) guidelines [19]. Subjects were allocated to two groups with an allocation ratio of one to one. Eligibility criteria and method were not changed during the trial. The study was approved by the Institutional Review Board at Western University of Health Sciences (Approval number 14-IRB-054) and conducted in accordance with the declaration of Helsinki. This study has been registered at ClinicalTrials. gov (Identifier: NCT02951065).
Participants
We recruited 23 subjects who received regular periodontal treatment at the Western University of Health Sciences Dental Center, and who had facial gingival recession with at least 1 mm clinical attachment loss in the anterior region of their mouths and were between 18 and 80 years of age. We excluded patients who could not provide consent; had severe uncontrolled medical conditions resulting in an American Society of Anesthesiologist’s Physical Status Class greater than III; acute pain or infection; caries near the gingival margin; restorations covering the gingival recession defect; presence of Miller Class III or IV defects [20]; severe or aggressive periodontitis; missing more than one anterior tooth; severe malocclusion; presence of occlusal trauma requiring more than limited adjustment; Tobacco use; ongoing or planned orthodontic therapy; oral piercings; or a history of bruxism, clenching, nail biting, holding pins with teeth, or gum scratching habits. We also excluded subjects who preferred to use an electric tooth brush over a manual brush. Subjects were enrolled between March 2015 and September 2015, and the last subject finished participation in February 2017.
Intervention: Subjects were randomly assigned to a test or control group through block assignment in blocks of 4 subjects at a time. At each visit, subjects received a comprehensive periodontal exam, personalized oral hygiene instruction demonstrating the modified Stillman technique for the soft brush or scrubbing technique for the bristle-less brush. Subjects received a low abrasivity toothpaste (Arm & Hammer™ Complete Care™ Plus Enamel Strengthening, York, Pennsylvania) and either a regular soft brush (Oral-B® Indicator Contour Clean Toothbrush, Iowa City, Iowa) or a specialty brush (PeriClean, Great Neck, New York) (Figure 1). Subjects were instructed to brush twice a day with the provided brush and toothpaste, and use waxed dental floss (Johnson&Johnson REACH Mint waxed floss, New Brunswick, New Jersey) twice daily. After oral hygiene instruction, subjects received periodontal maintenance. None of the subjects received occlusal adjustments as none of the teeth with recession defects had interference contacts at the onset of the study. For record keeping and future analysis, we obtained diagnostic casts using polyvinylsiloxane impressions. To ensure compliance with the oral hygiene regimen and monitor for unexpected problems associated with the brushes, subjects were contacted by phone to answer questions and concerns from the subjects about using the tooth brush. Periodontal exam, oral hygiene instruction and periodontal maintenance were repeated every 3-4 months for at least 9 months during the course of this study.
Outcomes
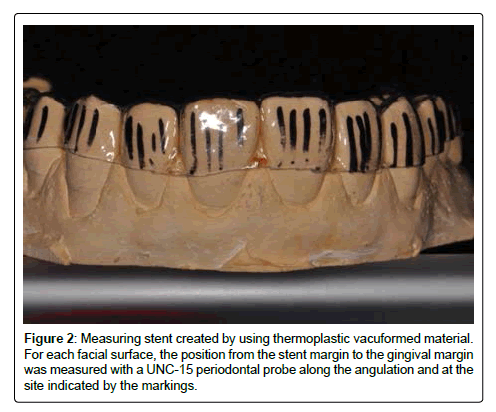
At each visit, a full mouth periodontal exam was conducted that measured probing depths, bleeding on probing, plaque levels and gingival recession. Measurements were recorded by the subject’s primary 3rd or 4th year dental student, and verified by a team of calibrated faculty (1 periodontist, 1 general dentist, 1 hygienist) on a virtually random basis. Neither students nor the verifying faculty were aware of the subject assignment. Periodontal probing was performed using light probing force and by gently walking the probe through the entire sulcus, recording the worst probing depths in the distobuccal, midbuccal, mesio-buccal, distolingual, midlingual and mesiolingual area of each tooth. For each area, bleeding on probing was recorded if a drop of blood appeared immediately after probing, and the percentage of sites with bleeding on probing calculated. Since effective facial/lingual cleaning was considered the most important aspect of the tested tooth brushes, plaque levels were assessed visually for the facial and lingual half of each tooth using the Turesky-modified Quigley-Hein plaque index [21]: facial and lingual tooth surfaces were scored as “0” if no plaque was present, “1” if specks of plaque were present and “2” if a thin continuous band of plaque was present less than 1 mm. A “3” indicated a thick band of plaque between 1 mm and 1/3 of the tooth surface, “4” meant that 1/3 to 2/3 of the tooth surface was covered in plaque, and “5” was reserved for heavy plaque accumulation covering more than 2/3 of the crown. Gingival recession was measured clinically at any site where the cemento enamel junction was exposed, and measurements were taken for these sites at the mesiofacial line angle, mid-facial center of tooth, disto-facial line angle, mesiolingual line angle, mid-lingual center of tooth and distolingual line angle from the cemento-enamel junction to the gingival margin. All measurements were carried out using a UNC-15 periodontal probe (Hu-Friedy, Chicago, Illinois), and the measurement method was not changed during the trial. As a second method for monitoring changes in gingival recession, we obtained polyvinylsiloxane impressions at the initial and 6 month visit, and fabricated a stent for measuring recession relative to the stent (Figure 2). We measured then relative recession at defined measurements paths on 4 sites per tooth on the facial gingiva from the gingival margin to the stent edge. We monitored use of the brushes not only by questioning subjects, but also checking the brushes for signs of wear as we collected the subject’s used tooth brushes at every visit. Tooth brush wear was determined using a normalized Rawl’s Tooth brush wear index. Since the Test brush had a convergent head shape, we normalized the wear index measurements to the wear index of a new tooth brush.
Sample size, randomization, blinding
We were interested in detecting a clinically significant effect of 0.5 mm difference in recession, and assumed a standard deviation of 0.7 mm (based on research comparing powered vs. manual brushes [22], yielding a minimum number of 31 sites with recession needed per group. (Assumptions for sample size calculation were: Type I error of 5%; power 80%). Subjects in sets of four were assigned randomly to allocation blocks by a series of coin tosses. Allocation of subjects and enrollment was performed by the lead investigator of this study (TKB), and verifying faculty were not informed of the subject allocation to either control or test brush. To increase the degree of concealment, students were not informed on the specific expected effect of the tooth brushes.
Data analysis
Group characteristics such as average age, recession, probing depths were compared using student t-test, and proportions of gender and ethnicity/race were compared using Chi-Square analysis. Normality of data such as the recession measurements were confirmed using the Shapiro-Wilk test. We analyzed recession by calculating the difference in measurement for each recession site at the initial visit and each followup visit (3 months, 6 months, 9 months), averaged recession changes for each group and compared these using the Welch Two sample t-test. Proportions of improved sites were compared with Fisher’s exact test. We also averaged plaque levels, probing depths and percent bleeding sites for all subjects, and compared the two averages for each clinical parameter using the Welch Two sample t-test. The Welch Two-sample t-test was also used for comparison of the normalized Rawl’s wear indices. All analyses were done using the R statistical package (Vienna, Austria) and data plotted using the ggplot2 package [23].
Results
We approached 71 subjects of possible inclusion in this study, and accepted 23 subjects from March to September 2015. While many potential subjects were not interested in participating in this study, we noticed a high preponderance of bruxism history (20 out of 26 patients meeting exclusion criteria) in patients with slight gingival recession. The 23 accepted subjects were distributed to the test and control group as described before. In the test group, four subjects dropped out over the course of the trial, but did not report a reason for dropping out. One subject in the test group did not want to continue using the test brush, but preferred a conventional soft brush. The control group had a lower drop-out rate with only one subject dropping out because of relocation, but three subjects did not attend the 3-month follow-up visit (Figure 3).
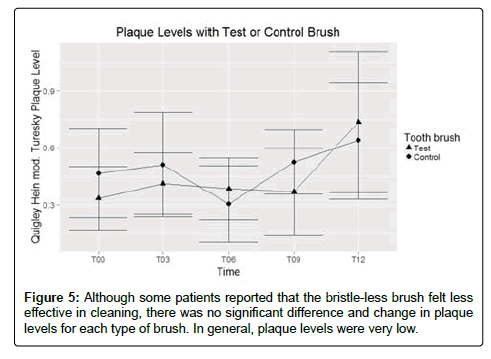
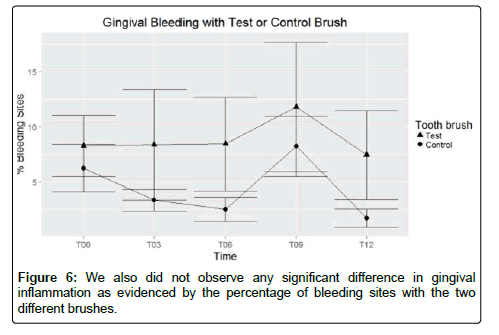
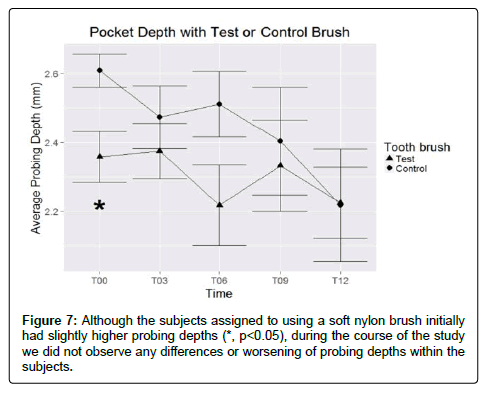
Randomization was largely successful with both groups not statistically significant in age, gender and ethnic make-up. Subjects generally had small amounts of gingival recession (0.4-0.5 mm on average) on facial surfaces of anterior teeth mostly with very little interproximal gingival recession at the onset of the study. Subjects were all well periodontally maintained at the onset and throughout the study, with minimal probing depths (2.4-2.6 mm, with the control group having a slightly higher initial probing depth), few sites exhibiting probing (6-8%) and low facial/lingual plaque levels (0.3-0.4 Quigley- Hein index as modified by Turesky). Generally patients had a history of generalized mild chronic periodontitis or gingivitis as indicated in their dental records and based on past clinical attachment readings (Table 1).
| Characteristic | Test | Control | |
|---|---|---|---|
| Number | 11 | 11 | |
| Female | 55% | 60% | |
| Averafe Age | 49 | 49 | |
| Tobacco Users | 0 | 0 | |
| Parafunction History | 0 | 0 | |
| Teeth Exhibiting Fremitus | 0 | 0 | |
| Ethnicity | |||
| Caucasian | 4 | 3 | |
| Hispanic | 2 | 6 | |
| Other | 5 | 1 | |
| Average Probing depth | 2.4 mm | 2.6 mm* | |
| Average % BOP Sites | 6 | 8 | |
| Average Plaque level | 0.3 | 0.4 | |
| Average Recession | 0.5 mm | 0.4 mm | |
| Number of sites with recession | 228 | 289 | |
Table 1: Subject composition- randomization produced experimental groups quite similar to each other, with no significant differences in demographics, initial number of sites with bleeding on probing, plaque level or amount of gingival recession. The control group initially had a slightly higher average probing depth which was considered a statistically significant difference.
Interexaminer agreement between the lead investigator (TKB) and verifying faculty for probing depths and recession measurements within 1 mm was about 96% (unweighted kappa scores ranged from 0.65 to 0.86). For plaque scores, this interexaminer agreement for plaque scores ranged between 80 to 100% (kappa score not determinable). Intraexaminer agreement for relative recession measurements was 92% (unweighted kappa 0.72).
Subjects used the tooth brushes as the returned brushes exhibited typical wear patterns associated with tooth brush use. Phone follow-up was done, and no problems reported with the toothbrushes.
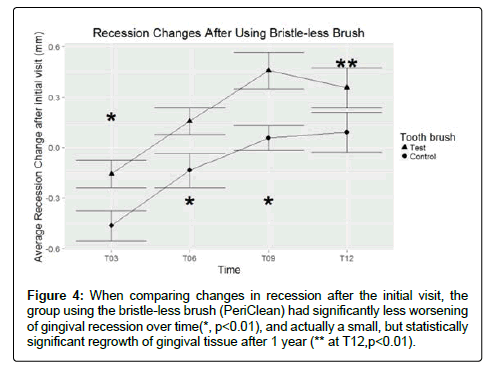
We followed recession changes over time for the test and control group, monitoring between 179 to 97 sites for the test group, and 156 to 115 sites for the control group. The number of sites varied as subjects dropped out of the study or missed appointments. We noted that although both groups initially seemed to have increased gingival recession after 3 months, only the control brush users exhibited significant additional recession compared to baseline measurements (p<0.001, 95% CI: 0.27 to 0.64 mm increased recession at sites with recession). As time went on, the initial increase in gingival recession reversed itself with no significant loss of gingival tissue at the end of the trial in the control group. Meanwhile, the test group showed significant gingival rebound, with an actual decrease of gingival recession compared to the original gingival margin position. Additionally, through the first 9 months, the test group experienced significantly less recession than the control group (p<0.05, about 0.4 mm difference in recession). At 12 months, the difference was not quite significant because of patient drop-out, although only the test group had significant improvement compared to the initial recession level (p<0.01) (Figure 4). When comparing the percentage of improved sites at 12 months, the test group had significantly more improved sites (55%) than the control group (36%, p<0.01).
Figure 4: When comparing changes in recession after the initial visit, the group using the bristle-less brush (PeriClean) had significantly less worsening of gingival recession over time(*, p<0.01), and actually a small, but statistically significant regrowth of gingival tissue after 1 year (** at T12,p<0.01).
We evaluated plaque levels to determine effectiveness of the brushes, and noted low plaque levels for both groups that generally amounted to no more than few specks of plaque on a given tooth surface. There were no statistically significant differences in plaque levels (p>0.05) (Figure 5).
Although facial and lingual plaque levels appeared similar for both groups, we could not rule out that there was a difference in interproximal cleaning efficiency between the brushes. We postulated if there was a difference in plaque removal between the brushes, it would result in increased gingival inflammation, which could cause gingival swelling and decreased gingival recession. To rule out inflammation as a source of the improved recession, we determined bleeding sites and probing depths, which should also increase if there is increased inflammation from poorer plaque removal. We did not see any significant difference in the number of sites with gingival bleeding (p>0.05) (Figure 6), and although initially the groups had slightly different probing depths, there was no significant difference in average probing depths between the groups (p>0.05) (Figure 7).
We reviewed diagnostic casts and clinical photographs to see if there were clinically noticeable changes. In both groups, there were no major changes in gingival color or shape, and plaque levels remained low. For the test group, we did notice a slight improvement in gingival architecture that produced slightly narrower recession defects, more parabolic gingival margin scallop and less visible erythema and edema. At some sites, we noticed a slight coronal creep of the gingival margin. The study was uneventful, and no subjects suffered adverse events from either tooth brush used. Control brush users expressed no comment or concerns about the brush or study, while test brush users either felt very satisfied with the brush, or felt that the brush was not aggressive enough in plaque removal. We noted that all subjects who had concerns about the brush’s effectiveness also had crowded teeth, which we answered by providing additional training for the subjects in using floss for interproximal cleaning.
We verified that the subjects did use the assigned tooth brushes through phone follow-up and by collecting the old tooth brushes at every visit. We noted that all returned brushes showed usage signs such as water stains, impacted food debris, discoloration of the tooth brush material, loss of bristles and splaying of bristles. We noted that the test brushes (Rawl’s index 0.026) withstood continued use much better than the control brushes (Rawl’s index 0.48, p<0.01). While the majority of control brushes showed some degree of bristle damage suggesting continued aggressive tooth brushing technique, the test brushes showed little damage other than water stains and patchy yellow to brown discoloration in all but one subject. The brushes returned from one subject showed no shape alteration, but loss of up to a third of rubber cones from the tip of the brush. Together with the comments from the test brush users, it seemed that the test brush design discouraged aggressive brushing techniques since it lacked bristles the subjects “could work into the spaces between the teeth” as one subject put it.
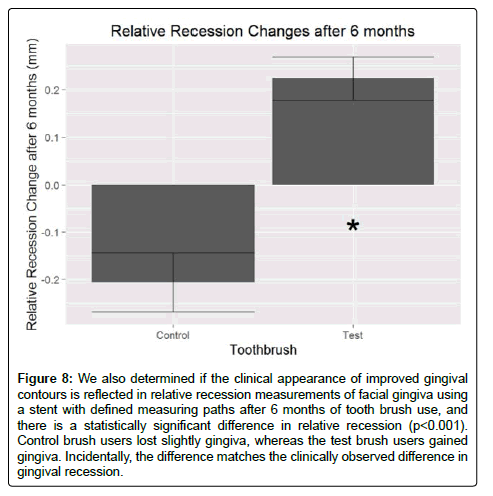
We verified the clinical measurements and observed changes by measuring relative recession as recorded on diagnostic casts obtained at the initial and 6 month visit. As seen in Figure 8, there was a statistically significant difference in the position of the gingiva relative to the fabricated stent (p<0.001). While the control brush users lost a small amount of facial gingiva, the test brush users gained a small amount. The difference observed mirrored what was observed clinically, and validated the clinical observations.
Figure 8: We also determined if the clinical appearance of improved gingival contours is reflected in relative recession measurements of facial gingiva using a stent with defined measuring paths after 6 months of tooth brush use, and there is a statistically significant difference in relative recession (p<0.001). Control brush users lost slightly gingiva, whereas the test brush users gained gingiva. Incidentally, the difference matches the clinically observed difference in gingival recession.
Discussion
We followed subjects for more than 12 months and we did not observe any adverse effects related from tooth brush use in either group, suggesting that the test brush can be used safely over long time periods. Both bristle-less and conventional brush designs can produce consistent plaque and inflammation control in patients on periodontal maintenance. While we did not see complete recovery of lost gingiva at sites with deep gingival recession, we noticed development of improved gingival appearance in the test group and slight, but statistically significant improvement of gingival recession in sites with facial or lingual recession. This may be clinically relevant as a soft, bristle-less tooth brush may be better at maintaining gingival margin positions in patients with a history of aggressive tooth brushing.
It is possible that that the decrease in gingival recession seen with the soft, bristle-less tooth brush is due to the inherent difficulty in inducing gingival abrasion and chronic trauma with such brush. It is known that generic bristled tooth brushes can induce gingival abrasion [24], especially if the bristles are hard and not rounded [25,26]. This may occur even in those who use little force while brushing [27]. In our subjects, we asked them to return their used tooth brushes, and about 5 subjects surrendered the tooth brush they originally used prior to the study. All of these brushes were generic brushes of indeterminate hardness, and together with the scrubbing technique used by most subjects prior to this study may have caused continuous tooth brush trauma leading to the gingival recession seen at the onset of the study. The continued loss of gingiva within the first 3 months, and then gradual improvement may be related to the subjects relearning their brushing technique at every visit. Since the recession initially got worse, it may indicate that the subjects continued with their old brushing technique and gradually modified it in response to our oral hygiene instruction, which then allowed gingival recovery. In contrast, using the bristle-less brush most likely prevents gingival abrasion immediately for lack of bristles, and regrowth of the gingival margin as there is no abrasion taking place. The effect of marginal regrowth was also likely amplified by the use of a dentifrice with known low abrasivity as abrasive dentifrices can enhance gingival abrasion [15], and the subjects had not used this type of dentifrice before.
While there is some clinical significance in that gingival recession may be able to be reversed slightly with a gentle dentifrice, tooth brush design and technique, this study has several limitations. For one, this is a pilot study that tested the brush on relatively few subjects as most patients with gingival recession defects at the Dental Center did not meet our strict inclusion criteria. We kept the inclusion criteria stringent to avoid known contributing factors to gingival recession such as periodontal disease, smoke-less tobacco use and occlusal trauma, which could obscure the effect of tooth brush design on gingival recession, and most of the excluded subjects had a history of parafunctional habits and gingival recession. The study also suffered from a significant amount of attrition in both groups as subjects dropped out or missed recall appointments, which was not related to the study but typical of the patient population served by this clinic. In general, compliance with treatment in a dental school clinic setting seems low as reported elsewhere [28]. A solution for this problem would be to conduct a larger trial of this brush in a group of private dental practices.
We addressed the possibility of inaccurate clinical measurements by dental students (un-weighted kappa was about 0.5-0.6 to a periodontist for recession measurement) by having the measurements verified by calibrated faculty, which improved interexaminer agreement and kappa to the reported value. In addition, we independently assessed recession changes using a measuring stent on diagnostic casts obtained during the study, which confirmed the clinical measurement results. The observed effect of about 0.4 mm improved recession in this study is similar to that observed by Acunzo’s powered vs. manual study [17], which suggests that this effect may be obtainable through a variety of methods. It also provides some assurance that a small degree of gingival margin recovery is possible even in the confines and less than ideal clinical setting of a dental school clinic.
No adverse effects were seen as consequence from the use of either test or control brush. Three subjects in the test group reported that “the brush does not feel like it cleans between teeth”, or “feels not aggressive enough”. Since plaque removal is one of the most important characteristics of a functional tooth brush, we evaluated plaque level trends as seen on facial and lingual surfaces, as neither brush in this trial was designed for interproximal cleaning. We did not see any statistically significant differences in plaque levels for both groups (p>0.05) (Figure 5). Both brushes appear to be equally effective in facial and lingual plaque removal, and we believe that these subjects did not feel the effectiveness of the test brush since it lacked bristles and did not provide a sensation of stiff bristles reaching between the teeth.
Conclusion
Based on the results of this limited trial, it seems that bristle-less brushes can be a safe alternative to conventional soft brushes in patients with gingival recession, and that they may be better at preventing additional gingival recession as they allow slight coronal expansion of the gingival margin.
Funding
This study was supported by a grant from PeriSwab, LLC (Great Neck, New York) that provided funds for supplies, tooth brushes, clinical procedure costs and publication cost. The authors have no financial interest or employment ties to this company.
Acknowledgement
We thank student doctor Mrs. Hyunok Jo for conducting the phone follow-up and student doctor Mr. Aleksey Kozlov for critical review of the manuscript.
References
- Merijohn GK (2016) Management and prevention of gingival recession. Periodontol 2000 71: 228-242.
- Litonjua LA, Andreana S, Bush PJ, Cohen RE (2003) Toothbrushing and gingival recession. Int Dent J 53: 67-72.
- Gillette WB, Van House RL (1980) Ill effects of improper oral hygeine procedure. J Am Dent Assoc 101: 476-480.
- Khocht A, Simon G, Person P,Denepitiya JL (1993) Gingival recession in relation to history of hard toothbrush use. J Periodontol 64: 900-905.
- Mythri S, Suryanarayan MA, Hegde S, Rajesh SK, Munaz M, et al. (2015) Etiology and occurrence of gingival recession - An epidemiological study. J Indian Soc Periodontol 19: 671-675.
- Goutoudi P, Koidis PT,Konstantinidis A (1997) Gingival recession: A cross-sectional clinical investigation. Eur J Prosthodont Restor Dent 5: 57-61.
- Rajapakse PS, McCracken GI, Gwynnett E, Steen ND, Guentsch A, et al.(2007) Does tooth brushing influence the development and progression of non-inflammatory gingival recession? A systematic review. J Clin Periodontol 34: 1046-1061.
- Daprile G, Gatto MR, Checchi L (2007) The evolution of buccal gingival recessions in a student population: a 5-year follow-up. J Periodontol 78: 611-614.
- Attin T,Buchalla W, Gollner M, Hellwig E (2000) Use of variable remineralization periods to improve the abrasion resistance of previously eroded enamel. Caries Res 34: 48-52.
- Zimmer S, Ozturk M, Barthel CR, Bizhang M, Jordan RA (2011) Cleaning efficacy and soft tissue trauma after use of manual toothbrushes with different bristle stiffness. J Periodontol 82: 267-271.
- Iwakami K, Watanabe Y (1989) Gingival response by the effect of brushing method and hardness of the toothbrush bristle. Meikai Daigaku Shigaku Zasshi 18: 244-266.
- Smukler H, Landsberg J (1984) The toothbrush and gingival traumatic injury. J Periodontol 55: 713-719.
- Addy M, Hunter ML (2003) Can tooth brushing damage your health? Effects on oral and dental tissues. Int Dent J 53 Suppl 3: 177-186.
- Cifcibasi E, Koyuncuoglu CZ, Baser U, Bozacioglu B, Kasali K, et al. (2014) Comparison of manual toothbrushes with different bristle designs in terms of cleaning efficacy and potential role on gingival recession. Eur J Dent 8: 395-401.
- Caporossi LS, Dutra DAM, Martins MR, Prochnow EP, Moreira CHC, et al. (2016) Combined effect of end-rounded versus tapered bristles and a dentifrice on plaque removal and gingival abrasion. Braz Oral Res 30.
- Anneroth G, Poppelman A (1975) Histological evaluation of gingival damage by toothbrushing. An experimental study in dog. Acta Odontol Scand 33: 119-127.
- Acunzo R, Limiroli E, Pagni G, Dudaite A, Consonni D, et al. (2016) Gingival margin stability after mucogingival plastic surgery. The effect of manual versus powered toothbrushing: A randomized clinical trial. J Periodontol 87: 1186-1194.
- Yanagishita Y, Yoshino K, Taniguchi Y, Yoda Y, Matsukubo T (2012) Nonsurgical recovery of interdental papillae under supportive periodontal therapy. Bull Tokyo Dent Coll 53: 141-146.
- Schulz KF, Altman DG, Moher D (2010) CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. BMJ 340: c332.
- Miller PD (1985) A classification of marginal tissue recession. Int J Periodontics Restorative Dent 5: 8-13.
- Turesky S, Gilmore ND, Glickman I (1970) Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol 41: 41-43.
- McCracken GI, Heasman L, Stacey F, Swan M, Steen N, et al. (2009) The impact of powered and manual toothbrushing on incipient gingival recession. J Clin Periodontol 36: 950-957.
- Wickham H (2009) Elegant graphics for data analysis, ggplot2. Springer-Verlag, New York
- Faus-Damia M, Segarra-Vidal M, Lucas-Alcahuz E, López-Roldán A,Gil-Loscos F, et al. (2015) Comparison of the clinical effects of white brand toothbrushes versus Vitis Suave(R). J Clin Exp Dent 7: e489-e494.
- Breitenmoser J,Mormann W, Muhlemann HR (1979) Damaging effects of toothbrush bristle end form on gingiva. J Periodontol 50: 212-216.
- Alexander JF, Saffir AJ, Gold W (1977) The measurement of the effect of toothbrushes on soft tissue abrasion. J Dent Res 56: 722-727.
- Danser MM, Timmerman MF, Jzerman Y, Bulthuis H, van der Velden U, et al. (1998) Evaluation of the incidence of gingival abrasion as a result of toothbrushing. J Clin Periodontol 25: 701-706.
- Plagmann HC,Engelsmann U, Koc her T (1990)Assessment of the acceptance of modern periodontal treatment. Dtsch Zahnarztl Z 45: 548-552.
Relevant Topics
- Advanced Bleeding Gums
- Advanced Receeding Gums
- Bleeding Gums
- Children’s Oral Health
- Coronal Fracture
- Dental Anestheia and Sedation
- Dental Plaque
- Dental Radiology
- Dentistry and Diabetes
- Fluoride Treatments
- Gum Cancer
- Gum Infection
- Occlusal Splint
- Oral and Maxillofacial Pathology
- Oral Hygiene
- Oral Hygiene Blogs
- Oral Hygiene Case Reports
- Oral Hygiene Practice
- Oral Leukoplakia
- Oral Microbiome
- Oral Rehydration
- Oral Surgery Special Issue
- Orthodontistry
- Periodontal Disease Management
- Periodontistry
- Root Canal Treatment
- Tele-Dentistry
Recommended Journals
Article Tools
Article Usage
- Total views: 6168
- [From(publication date):
July-2017 - Sep 20, 2024] - Breakdown by view type
- HTML page views : 5318
- PDF downloads : 850