HTLV I Myelopathy Prognostic Factors for Total Gait Disability in Patients with Human T Cell Lymphotropic Virus I Associated Myelopathy: a 12-Year Follow-Up Study
Received: 05-May-2013 / Accepted Date: 23-Aug-2013 / Published Date: 25-Aug-2013 DOI: 10.4172/2161-1165.1000131
Abstract
Objectives:
Analyze risk factors for progression towards total gait disability in patients with HAM/TSP.
Methods:
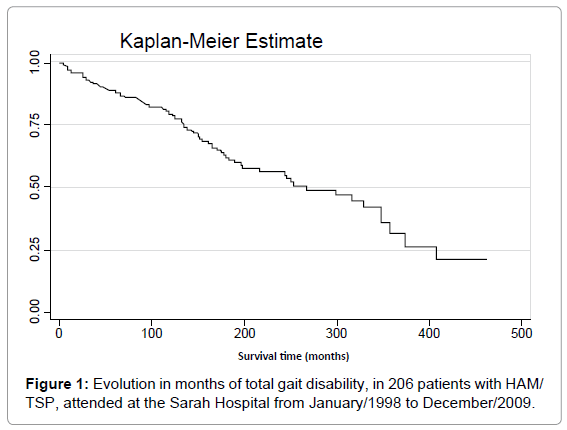
Cohort for investigation of clinical-epidemiological characteristics. The outcome variable of the study was total incapacity to walk. The analysis was conducted using the Kaplan-Meier curve and Cox regression model.
Results:
206 patients were included, with an average time of total gait disability of 22.3 years. The following variables did not have an influence on the prognosis: sex, marital status, educational level, presence of neuropathic pain, diabetes, hypertension, alcoholism and tabagism, blood transfusions, HTLV-1 seropositive partner or mother and spinal medulla atrophy in the MRI. After performing Cox regression, a higher age at onset, the presence of articular limitations in the lower limbs and the level of thoracic neurological lesion are kept as clinical predictors of total gait disability.
Conclusions:
It is necessary to prevent and improve articular limitations in the lower limbs. Patients over the age of sixty had the worst prognosis, probably related to senescence. Few clinical and epidemiological factors explain the different prognoses for the patients with HAM/TSP and the patients who had an initial neurological profile of greater severity presented total gait disabilities in a shorter time.
Keywords: Epidemiology, Human T-cell lymphotropic virus type 1 (HTLV-I), Tropical spastic Paraparesis, Prognosis, Risk factors, Cohort studies
160663Introduction
Human T cell Lymphotropic virus (HTLV-1) Associated Myelopathy (HAM/TSP), despite its rare frequency, is a serious incapacitating disease that presents a high morbidity rate, impairing the ability to perform daily activities and the quality of life. There are few investigations into the natural course of this pathology and treatment, so far, has not been well established.
The presence of HTLV-1 infection does not necessarily mean a pathological process for its carriers. Different factors in the virus/host interaction will determine whether a disease develops and what form it will take. It may behave as a hematological manifestation - T cell lymphoma - myelopathy, myopathy, uveitis or rheumatoid arthritis [1,2]. Myelopathy (HAM/TSP) is the most frequent manifestation of HTLV-1 and occurs in over 4% of the carriers of this virus [3]. HAM/ TSP presents an insidious beginning and slow progress, individuals turning symptomatic in their fourth and fifth decades of life, rarely prior to the age of 20 or after the age of 70. There is predominance of the female sex, with a sex ratio of about 2-3:1. Gait disturbances, weakness and stiffness in the lower limbs are consequences of the gradual decrease in muscular strength and spasticity in the affected myotomes [4].
HTLV-1-associated myelopathy has a progressive characteristic and, as the disease evolves, mobility worsens, generally following an advancing pattern: need for unilateral support, bilateral support and, finally, a wheelchair. Vesical-intestinal or sexual dysfunction may be one of the patient’s first complaints. Generally, they are characterized by vesical urge incontinence, intestinal constipation and erectile dysfunction, among the male population [4].
Little is known about why some patients develop total gait disability more quickly than others, and findings are still controversial in scientific literature. The average time of the evolution towards total gait disability, described in the literature, varies from a few months to several decades. It is estimated that 50% of the patients experience a significant clinical progression of myelopathy in the first ten years, and that, by then, only one third of patients remain able to walk without support for 500 meters, one quarter need a walker and the remaining third need a wheelchair [5].
Different factors in this virus-host relationship appear to influence the course of the myelopathy. A four-year cohort study in Japan suggests that the progression of myelopathy will occur mainly in the period immediately after the onset of symptoms, becoming stable after this [6]. Cross-sectional studies, in Brazil, also indicate that there is a neurological worsening in the first year of the disease, followed by a stabilization of the clinical profile presenting a worse prognosis for females, independent of the route of infection [7,8]. There is also a suggestion of a faster progression in older patients, those over 61 years of age, in Japan and over fifty years of age, in Martinique [9,10]. The progression to DSS 6 (KURTZKE 1955) in the first three years of disease manifestation was also found to be a prognostic factor to a rapid progress to a wheelchair in the Martinique study [10,11].
An analysis of a large series of Japanese cases proposes that the acquisition of the infection via blood transfusion would worsen the prognostics for physical incapacity [9]. Spasticity, measured by the Ashworth scale, appears to behave as an indicator of severity in a sectional study [5]. HTLV-1 viral load seems to have no influence in clinical progression [12].
The objective of this study is to identify clinical and epidemiological prognostic factors to total gait disability in a cohort of patients with HAM/TSP.
Materials and Methods
This is a longitudinal study classified as historical cohort of patients with HTLV-1-associated myelopathy, monitored through the Adult Spinal Injury Rehabilitation Program at the Belo Horizonte Unit of the Sarah Network of Rehabilitation Hospitals, and hereinafter called the Belo Horizonte Sarah Hospital. Patients were admitted from January of 1998 to December of 2007. The Sarah Network of Rehabilitation Hospitals is run by the Association of Social Pioneers, which is an independent, private, non-profit social entity dedicated to the rehabilitation and treatment of deformities, sequel as resulting from trauma, diseases that affect mobility and neurological development problems. In 2008, the nine hospitals in the Network attended an average of 6,398 patients per day, totalling, in this year, over 1,612,323 patients attended (source: www.sarah.br). The Belo Horizonte Sarah Hospital is one of these units and is the reference for rehabilitation assistance at the State of Minas Gerais, Southeast Region of Brazil, with approximately 17 million inhabitants (source: www.ibge.gov.br).
All 206 patients over the age of 18 that met the diagnostic criteria were included in the study. The diagnosis was established according to: 1) progressive paraparesis, varying from a few months to years, and neurogenic bladder symptoms, 2) detection of anti-HTLV-1 antibodies in blood serum and/or cerebrospinal fluid and 3) exclusion of other pathologies that are similar to HAM/TSP [13]. The clinical profile and epidemiology of the population is presented in greater detail in a previously published article [14].
Data were obtained from electronic records containing information about all consultations and exams for these patients. The outcome variable of the study was the presence of total incapacity to walk, that is, confinement to a wheelchair. Supports for walking assistance were defined as unilateral (“T” shaped cane) or bilateral (crutch or walker).
The time zero for the follow up of the cohort was defined as the date of the onset of symptoms. The end point date was the date when the use of a wheelchair was recommended or the end of follow up in December 01, 2009, whichever occurred first.
Patients that died prior to reaching the outcome variable - need of a wheelchair - or the study end, were treated as ‘censored’ and had their progression time calculated up to the moment of their exclusion from the cohort. Those who died after needing a wheelchair were treated as ‘non-censored’.
The prescription of wheelchair is determined by balance evaluation and the motor index that quantifies the extension of paralysis and is linked to physiological indices of energy expenditures and gait performance, in which a value lower than or equal to 40% is indicative of the need for a wheelchair (Perry 1992). The electronic health record supplies the exact dates of the prescriptions for walking supports and use of a wheelchair, when required.
The independent variables were: 1) socio-epidemiological characteristics: gender, age, marital status, level of education, probable route of transmission, seropositivity of spouse or mother, 2) lifestyle: alcohol or tobacco consumption 3) clinical: blood transfusion prior to 1993, presence of neuropathic pain and co- morbidities (diabetes mellitus and hypertension), 4) physical signs: spasticity, the use of some type of support for locomotion, the presence of articular limitations in lower limbs and the level of neurological lesions (cervical, thoracic or lumbosacral) and 5) presence of atrophy of spinal cord on Magnetic Resonance Imaging (MRI).
The age of the patients was considered as the age when the symptoms appeared and not when they were admitted into the rehabilitation service. All the clinical diagnostics and physical evaluation criteria follow standardized international guidelines. Hypertension was defined as PA ≥ 140/90 mmHg and/or the use of anti-hypertensive drugs [15]. Diabetes mellitus was defined through fasting blood glucose or a glucose tolerance test [16]. The classification from the American Spinal Injury Association (ASIA) was used to establish criteria for neurological lesions, at sensory and motor levels [17]. Range of motion measurement was conducted using a goniometer, with articular range of motion being measured in the passive manual exam [18].
Statistical analysis
The data from the electronic health records were fed into an Excel spreadsheet and analyzed using the STATA 9.0 statistical program. An exploratory analysis of the data was performed in order to ascertain the characteristics of the study population and the incidence of the variables described.
The Kaplan-Meier survival function curve was used to evaluate the survival time until gait disability in this population. All the variables that present p<0.20, in the univariate analysis, were selected for multivariate analysis and, as the time variable was followed unequally, the Cox logistic regression was chosen. The significance value considered for the hazard ratio in the multivariate analysis was p<0.05. The proportional assumption that the ratio of the hazard functions for two observations does not depend on time was verified graphically.
Ethical aspects
This study was approved by the Research Ethics Committees of the Federal University of Minas Gerais (ruling 664/08 COEP UFMG) and of the Sarah Network of Rehabilitation Hospitals.
Results
The study population is predominantly female, with a proportion of 2:1 in relation to the male gender. The average age of the patients, at the onset of symptoms, was 44.8 (± 14.1) years of age and, at the time of admission into the service, their average age was 53.8 (± 13.1), or that is, there was an average period of 9.0 (± 7.8) years between the beginning myelopathy and their admission into the rehabilitation service (Table 1). A low level of education was observed among the patients, 72% of whom had no more than eight years of schooling. The majority came from the metropolitan and central regions of Minas Gerais State (81%). Fifty-four (26%) individuals were identified as smokers. The daily consumption of alcohol was referred by 24 (12%) patients.
| Characteristic | N of cases (%) |
|---|---|
| Gender | |
| Female | 139 (67%) |
| Male | 67 (33%) |
| Age at the onset of symptoms, in years | |
| Mean (standard deviation) | 44.8 (± 14.1) |
| Median | 46 |
| Time of illness, in years | |
| Mean (standard deviation) | 9.0 (± 7.8) |
| Median (confidence interval) | 6.5 (3.0 -12.0) |
| Educational Level | |
| Illiterate | 27 (13%) |
| 1 to 8 years | 148 (72%) |
| 9 to 11 years | 25 (13%) |
| More than 12 years | 6 (3%) |
| Origin of Patient | |
| Central Region of Minas Gerais and Metropolitan Belo | 166 (81%) |
| Horizonte | |
| 31 (15.0%) | |
| Other regions of Minas Gerais State | |
| 9 (4.4%) | |
| Other States in Brazil | |
| Symptoms reported when admitted | |
| Gait disturbance | 157 (76%) |
| Neurogenic bladder | 182 (88%) |
| Intestinal constipation | 161(78%) |
| Pain | 104 (50%) |
| Spasticity | 163 (79%) |
| Erectile dysfunction | 39(58%) |
Table 1: Clinical-epidemiological profile of the 206 patients with HAM/TSP, admitted from January of 1998 to December of 2007 at the Belo Horizonte Sarah Hospital.
With regard to HTLV-1 possible route of transmission, 23 (11%) patients mentioned blood transfusions prior to 1993. The presence of seropositive family members was observed in 47 (22%) patients and, of these, 32 (68%) of the family members were spouses and nine (19%) were children. Positive maternal serology was found in 11 (23%) of them, suggesting vertical transmission. The patients whose mothers presented positive serology for HTLV had a lower average age at the onset of symptoms, of 31.9 years (bilateral Student test p<0.001).
The most frequent symptoms were a reduction in strength in the lower limbs and consequent gait complications, which were reported by 157 (76%) patients, the presence of a neurogenic bladder in 182 (88%) and intestinal constipation in 161 (78%) of the cases. One hundred and four (50%) patients reported pain, characterized as neuropathic in 65 (63%) of the cases, as osteomuscular in 35 (33%) and mixed (osteomuscular and neuropathic) in four patients.
The level of neurological lesion most frequently found was lumbosacral, in 106 (51.5%) patients, followed by thoracic lesion, in 61 patients (29.6%). Motion range limitation in the lower limbs was observed in 34 (16.6%) individuals.
During the study period, 16 (7.7%) patients died, after an average of 13.5 (± 7.94) years from the beginning of HAM/TSP. The average age at death was 67.12 (± 18.60) years of age. The causes mentioned on death certificates were pneumonia in six cases, pulmonary embolism in two and one case of cerebral vascular accident, another of congestive cardiac insufficiency and other neoplasia. The cause of death was unknown in four cases (Table 1).
The average time for evolution until total gait disability was 267.8 months, 22.3 years. Figure 1 shows the survival curve in months towards total gait disability, demonstrating that over 80% of the individuals did not require the use of a wheelchair in the first 100 months following the onset of symptoms but, after 400 months, only 25% of the patients were wheelchair free.
The results of the survival analysis and the log rank tests for the association of clinical and epidemiological factors with time to gait disability are summarized in Tables 2 and 3. Briefly, of the 19 variables tested, six were shown to be associated with a faster progression towards total gait disability: age equal or greater than 60 years, spasticity in lower limbs, motion range limitations in lower limbs, level thoracic of neurological lesion and the use of support for walking in less than 1 and to 3 years after disease onset (Tables 2 and 3).
| Characteristics | Time of evolution to wheelchair 25% (133.9) 50% (267.8) | Qui-square (Logrank) 75%( 407.8) | p | ||
|---|---|---|---|---|---|
| Gender | |||||
| Male | 164.4 | 346.9 | 373.4 | 0.54 | 0.460 |
| Female | 124.8 | 267.8 | 407.8 | ||
| Age = 50 years | |||||
| No | 152.1 | 298.3 | 407.8 | ||
| Yes | 117.7 | 0. 0 | 0. 0 | 1.59 | 0.200 |
| Age = 60 years | |||||
| No | 143.1 | 298.3 | 407.8 | 6.01 | 0.010 |
| Yes | 59.8 | 0. 0 | 0. 0 | ||
| Educational Level | |||||
| Illiterate | 133.9 | 316.5 | - | 0.27 | 0.870 |
| 1 to 8 years | 124.7 | 298.3 | 373.3 | ||
| More than 8 years | 170.4 | 253.6 | 407.8 | ||
| Marital status | |||||
| Single | 183.6 | 328.7 | 373.4 | 2.75 | 0.430 |
| Married | 137.9 | 253.6 | - | ||
| Separated | 131.9 | 243.5 | 407.8 | ||
| Widowed | 117.7 | 188.8 | - | ||
| Seropositive spouse | |||||
| No | 131.9 | 267.8 | 373.3 | 0.74 | 0.380 |
| Yes | 137.9 | - | - | ||
| Seropositive mother | |||||
| No | 133.9 | 253.6 | 407.8 | 0.74 | 0.380 |
| Yes | - | - | - | ||
| Blood Transfusion | |||||
| No | 132.9 | 253.6 | 407.8 | 0.13 | 0.710 |
| Yes | 177.5 | 316.5 | 328.7 | ||
| Smoking | |||||
| No | 133.9 | 267.8 | 373.3 | 0.02 | 0.890 |
| Yes | 146.1 | 328.7 | 407.8 | ||
| Alcohol consumption | |||||
| No | 133.9 | 267.8 | 407.8 | 0.05 | 0.820 |
| Yes | 146.1 | 328.7 | 346.9 | ||
Table 2: Evolution in months of gait disability as per sociodemographic characteristics, means of transmission and lifestyle, in 206 patients with HAM/TSP, admitted to the Belo Horizonte Sarah Hospital from January/1998 to December/2007.
| Characteristics | Time of evolution until wheelchair 25% (133.9) 50% (267.8) | Qui-square (Logrank) 75%( 407.8) | p | ||
|---|---|---|---|---|---|
| Neuropathic pain | |||||
| No | 132.9 | 267.8 | 373.3 | 0.38 | 0.530 |
| Yes | 137.9 | - | - | ||
| Hypertension | |||||
| No | 143.0 | 267.8 | 407.8 | ||
| Yes | 131.86 | 197.9 | - | 0.62 | 0.430 |
| Diabetes | |||||
| No | 133.9 | 267.8 | 407.8 | 1.14 | 0.280 |
| Yes | 47.7 | 170.4 | - | ||
| Spasticity | |||||
| No | 328.7 | 346.9 | 346.9 | 5.53 | 0.010 |
| Yes | 124.7 | 243.5 | 407.8 | ||
| Limited in lower limbs | |||||
| No | 146.1 | 328.7 | - | 6.05 | 0.010 |
| Yes | 40.53 | 216.1 | 316.5 | ||
| Level of neurological | |||||
| lesion | |||||
| Cervical | 183.7 | 316.5 | 407.8 | 9.0 | 0.020 |
| Thoracic | 143.0 | 179.5 | 346.9 | ||
| Lumbosacral | 131.9 | 328.7 | - | ||
| Spinal Cord MRI | |||||
| No | 117.7 | 253.6 | 357.06 | 0.14 | 0.700 |
| Yes | 121.7 | 243.5 | 373.3 | ||
| Use support = 1 year | |||||
| No | 151.2 | 298.3 | 407.8 | 2.08 | 0.140 |
| Yes | 89.3 | 245.5 | - | ||
| Use support = 3 years | |||||
| No | 161.3 | 328.7 | 407.8 | 9.63 | 0.001 |
| Yes | 111.6 | 197.8 | 267.8 | ||
Table 3: Evolution in months of gait disability as per clinical characteristics, magnetic resonance imaging and use of support for walking, in 206 patients with HAM/TSP, admitted to the Belo Horizonte Sarah Hospital from January/1998 to December/2007.
Using the Cox proportional hazard regression, three variables remained statistically associated with total gait disability: older age (60+ years), presence of limitation in articular motion in the lower limbs at the time of admittance to the service and neurological lesion at the thoracic level (Table 4).
| Variable | Risk Rate | CI (95%) | P value |
|---|---|---|---|
| Age = 60 years | 3.02 | 1.0-5.0 | 0.003 |
| Thoracic neurological level | 2.13 | 1.27-22 | 0.030 |
| Limited motion range in Lower Limbs | 2.52 | 1.43-5.5 | 0.010 |
Table 4: Multivariate Analysis of the total gait disability time for 206 patients with HAM/TSP.
As not all the patients were monitored for the same duration of time, Table 5 shows the Cox regression results considering only the patients that were followed up for at least 36 months. The need of unilateral or bilateral support in the first three years (or 36 months) after the onset of symptoms doubled the risk of total gait incapacity. In this analysis, presence of spinal cord lesion at the thoracic level and articular limitation in the lower limbs were not statistically significant (Tables 4 and 5).
| Variable | Risk Rate | CI (95%) | P value |
|---|---|---|---|
| Age = 60 years | 2.69 | 1.3-5.7 | 0.007 |
| Unilateral or bilateral support = 3 years | 2.45 | 1.1-3.8 | 0.014 |
Table 5: Multivariate Analysis of the total gait disability time, with support use variable = 3 years, for 194 patients with HAM/TSP.
Discussion
To our knowledge, this is the largest cohort of patients with HAM/ TPS and the first Brazilian one to achieve 12 years of follow up. The few studies that investigated risk factors associated with the progress to gait disability in patients with HAM/TSP are, in their majority, crosssectional or cohort studies with short follow up times [5,7,9,19,20].
The prognostic studies of myelopathy have, in common, evidence of the insidious beginning and slowly progressive evolution, with few subacute groups. In this study, the mean time for total gait disability was about 22 years, similar to that detected in the population of Martinque. As with all the other studies, there was no evidence of a remission in the neurological profile, the patient gradually loses the capacity to walk and requires, over time, assistance to walk (canes or walkers) until; finally, the condition may evolve to the use of a wheelchair.
Mortality rate was low among the population of this study; only 7.7% of the patients died. However, in confirmation of previous findings, the patients with HAM/TSP had a life expectancy roughly 7.8 years lower than that expected for the population of the State of Minas Gerais, which is 74.9 years (www.ibge.gov.br) and at least 50% of the deaths may be related to a physical condition compromised by HTLV- 1 (pneumonia and pulmonary embolism).
Older patients (60+ years of age) had the fastest progression to total gait disability, as has been shown [9]. The rapid progression in older patients raises questions regarding two important aspects: the spinal cord of these patients would be more susceptible to the action of the HTLV-1, with greater neuronal damage; and/or the physiological capacity to adapt and to compensate in older individuals is worse, leading to articular limitations through shortening of muscles, poor posture, and shorter muscular contraction time.
In the present study, the female gender was not a prognostic marker for total gait disability, which differs from what has been previously published in a Brazilian cross-sectional study, but similar to the findings of the Martinique cohort study [8,9]. Apparently, the action of female hormones increases the chance of developing the illness, but, once the myelopathy has begun, the speed of progression is similar to that of male patients.
Presence of articular limitation in the lower limbs at the time of patient’s admission to the rehabilitation service was predictive of total gait disability. It has been already demonstrated a decreased range of motion on rheumatologic exam among seropositive subjects in comparison to HTLV-1- negative individuals [2]. This physical sign is the result of spasticity and muscular contracture, since the most common cause of deficit in the motion arc is due to muscular shortening. Each affected joint will present a specific problem: ankle limitation blocks the movement of the limb over the supporting foot; contracture, when bending the knee, blocks progression during support, due to inhibition of the advance of the thigh and, by extension, increases the energy cost of walking; and limitation of hip flexion generates walking instability in the support phase. Compromised muscular strength, related with a limited motion arc, prevents the patient from making compensations that may modify the duration of the muscular action and avoid incorrect postures, utilizing subtle modes of advancing the limb when walking. The worst prognosis for patients with articular limitation shows the need to invest in stretching of the lower limbs, not only as a means of prevention, but also as a treatment for some of the shortening already experienced.
Upon admission to the rehabilitation service, 163 (79%) patients presented spasms during the physical exam. Spasticity, hypertonia essentially constituted by the exacerbation of reflex activities that utilize the myotatic reflex arc, is a frequent finding in patients with HAM/ TSP and is considered an indicator of disease severity. The presence of spasticity may be one of the causes of lower amplitude of the lower limbs, which is a disability marker detected during analysis. Spasticity was not retained as a predictive variable in the multivariate analysis, indicating that other factors are more important to predict a worse clinical prognosis. However, clinically, it was noted that muscular spasms obstructed excentric quality during the walking support phase, and there was a lack of selective control that prevented the patient from controlling the duration and intensity of the muscular action.
A neurological lesion at the thoracic level was a predictor to fast gait disability probably due to the compromise of the torso, which causes alterations in balance. A lesion at the thoracic neurological level means that the patient, in addition to sensory-motor loss in the lower limbs (lesion at the lombo-sacral level), also suffers a sensory loss in the torso. This alteration in sensibility deprives the patient of the capacity to perceive the position of the hips, the knee, the ankle or the foot and of the type of contact with the ground, and this may negatively influence their ability to walk. Neuropathic pain, in itself, is not the cause of neurological worsening, though it is known that it exerts an influence on the physiological reactions of the patient who, in a protection reflex, takes up anti-algic postures that may result in deformity and muscular weakness. Nevertheless, the lack of statistical significance indicates that pain is not related to HAM/TSP prognosis.
Having a mother HTLV-1 seropositive, an indicator of probable vertical transmission, made no statistical difference in relation to the speed of progress to confinement to a wheelchair, perhaps due to the small number of cases. However, the average time for the onset of symptoms in these patients is roughly 13 years lower than for the other patients (31.9 vs. 45.4 years of age; p< 0.001). This fact has already been described in other studies and points out to the potential for earlier presentation of myelopathy in those infected since birth. However, in this study, this did not mean a worse prognosis, since the evolution time to total gait disability.
Blood transfusion had no prognostic value, perhaps because only a small number of patients had received blood transfusions prior to December of 1992. This date is significant as, routine screening for HTLV-1 antibodies in Brazilian blood banks began in early 1993 [21].
Previous studies suggest that HAM/TSP would have a greater neurological progression in the first year after the onset of symptoms, followed by the stabilization of the clinical profile [21,22]. This study demonstrates that individuals that present a more serious presentation at beginning, requiring the use of some support for walking within a period less than or equal to three years, lose the ability to walk roughly 11 years earlier.
HTLV-1-associated myelopathy, despite being rare, is a serious, debilitating illness that progresses with an elevated morbidity rate, compromising the ability to engage in day-to-day activities and the quality of life. There have been few investigations into the natural course of this pathology.
This study identified four clinical markers for worse evolution of the disease: the onset of symptoms after the age of 60; early need for support for walking (up to 36 months), movement amplitude limitations in the lower limbs and lesion at the thoracic neurological level. These factors must be continually monitored and the population at risk must receive special attention from rehabilitation professionals.
The control of spasticity with medication and therapeutic exercise and the prevention of the shortening of muscles by stretching must be begun early, because this may benefit patients.
The host’s clinical and epidemiological factors explain a small part of the variability and seriousness of the clinical expression of this disease. Studies that evaluate the different virus-host interactions in an effort to identify factors related to the viral antigens and proviral load, in addition to immune response elements, such as the expression of T CD4+ e T CD8+ lymphocyte activation molecules are also important.
References
- Costa CM, Dom R, Carton H, Santos TJ, Andrada-Serpa MJ (2002) Neuropathology of human and experimental TSP/HAM: a critical review. Acta Neurol Belg102: 21-29.
- Poetker SK, Porto AF, Giozza SP, Muniz AL, Caskey MF, et al. (2011) Clinical manifestations in individuals with recent diagnosis of HTLV type I infection. J Clin Virol 51: 54-58.
- Kaplan JE, Osame M, Kubota H, Igata A, Nishitani H, et al. (1990) The risk of development of HTLV-I-associated myelopathy/tropical spastic paraparesis among persons infected with HTLV-I. J Acquir Immune Defic Syndr 3:1096-1101
- Goncalves DU, Proietti FA, Barbosa-Stancioli EF, Martins ML, Ribas JG, et al. (2008) HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP) inflammatory network. Inflamm Allergy Drug Targets. 7: 98-107.
- Carod-Artal FJ, Mesquita HM, Ribeiro LS (2008) Neurological symptoms and disability in HTLV-1 associated myelopathy. Neurologia 23: 78-84
- Kuroda Y, Yukitake M, Kurohara K, Takashima H, Matsui M (1995) A follow-up study on spastic paraparesis in Japanese HAM/TSP. J Neurol Sci 132:174-176
- Araujo AQ, Leite AC, Dultra SV, ndrada-Serpa MJ (1995) Progression of neurological disability in HTLV-I-associated myelopathy/tropical spastic paraparesis (HAM/TSP). J Neurol Sci 129: 147-151.
- Lima MA, Bica RB, Araujo A (2005) Gender influence on the progression of HTLV-I associated myelopathy/tropical spastic paraparesis. J Neurol Neurosurg Psychiatry 76: 294-296.
- Nakagawa M, Izumo S, Ijichi S, Kubota H, Arimura K, et al. (1995) HTLV-I-associated myelopathy: analysis of 213 patients based on clinical features and laboratory findings. J Neurovirol 1: 50-61.
- Olindo S, Cabre P, Lézin A, Merle H, Saint-Vil M, et al. (2006) Natural history of human T-lymphotropic virus 1-associated myelopathy: a 14-year follow-up study. Arch Neurol 63: 1560-1566.
- Kurtzke JF (1955) A new scale for evaluating disability in multiple sclerosis. Neurology 5: 580-583.
- Martin F, Fedina Al, Youshya S, Taylor G (2010) A 15-year prospective longitudinal study of disease progression in patients with HTLV-1.associated myelopathy in the UK. J Neurol Neurosurg Psychiatry 81: 1336-1340
- De Castro-Costa CM, Araújo AQ, Barreto MM, Takayanagui OM, Sohler MP, et al. (2006) Proposal for diagnostic criteria of tropical spastic paraparesis/HTLV-I-associated myelopathy (TSP/HAM). AIDS Res Hum Retroviruses 22: 931-935.
- Ali Shoeibi, Houshang Rafatpanah, Amir Azarpazhooh, Naghme Mokhber, Mohammad Reza Hedayati-Moghaddam, et al. (2010) HTLV-1Associated Myelopathy: clinical and epidemiological profile in a 10 years cross-sectional study. Rev Soc Bras Med Trop 43: 668-672
- Sociedade Brasileira de Cardiologia (2007) V Diretrizes Brasileiras de Hipertensão Arterial. Arq Bras Cardiol 89: 24-79.
- Gross Jorge, Silveiro Sandra P, Camargo Joiza L, Reichelt Angela J, Azevedo MJ (2002) Diabetes Melito: Diagnóstico, Classificação e Avaliação do Controle Glicêmico. Arq Bras Endocrinol Metab 46:16-26.
- American Spinal Injury Association (2002) International standards for neurological classification of spinal cord injury. (6thedn), Chicago, IL.
- Hislop HJ, Montgomery J (2002) Daniels and Worthingham's muscle testing: techniques of manual examination. (7th edn.) W.B. Saunders, Philadelphia.
- Franzoi AC, Araujo AQ (2005) Disability profile of patients with HTLV-I-associated myelopathy/tropical spastic paraparesis using the Functional Independence Measure (FIM). Spinal Cord 43: 236-240.
- Franzoi AC, Araujo AQ (2007) Disability and determinants of gait performance in tropical spastic paraparesis/HTLV-I associated myelopathy (HAM/TSP). Spinal Cord 45: 64-68.
- Passos VM, Calazans FF, Carneiro-Proietti AB (1998) Counseling blood donors seropositive for Human T-Lymphotropic Virus Type I and li in a developing country. Cadernos de Saúde Pública(Fiocruz).14: 416-420.
- Kuroda Y, Fujiyama F, Nagumo F (1991) Analysis of factors of relevance to rapid clinical progression in HTLV-I-associated myelopathy. J Neurol Sci. 105: 61-66.
Citation: Silva Champs AP, de Azeredo Passos VM, Barreto SM, Vaz LS, Ramos Ribas JG (2013) HTLV I Myelopathy Prognostic Factors for Total Gait Disability in Patients with Human T Cell Lymphotropic Virus I Associated Myelopathy: a 12-Year Follow-Up Study. Epidemiol 3:131. DOI: 10.4172/2161-1165.1000131
Copyright: © 2013 Silva Champs AP, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 16242
- [From(publication date): 8-2013 - Nov 16, 2025]
- Breakdown by view type
- HTML page views: 11360
- PDF downloads: 4882