A New Approach to Ankle and Foot Arthrodesis Procedures Using a Living Cellular Bone Matrix: A Case Series
Received: 04-Sep-2018 / Accepted Date: 14-Sep-2018 / Published Date: 21-Sep-2018 DOI: 10.4172/2329-910X.1000274
Keywords: Cellular bone allograft; Ankle arthrodesis; Tibiotalocalcaneal arthrodesis; Lapidus revision; ViviGen
Level Of Evidence
Level 4.
Introduction
The number of foot and ankle arthrodesis procedures performed in the United States has been rapidly increasing [1]. These procedures include ankle arthrodesis to induce fusion between the tibia and talus [2], double arthrodesis of the hindfoot to fuse the talonavicular and subtalar joints while sparing the calcaneocuboid [3], tibiotalocalcaneal (TTC) arthrodesis to fuse the ankle and hind foot [4], and modified Lapidus to correct hypermobility of the first tarsal-metatarsal joint (TMJ) [5]. The goal of these procedures is to correct arthritis, instability, poor alignment, and pain, which can be debilitating. Arthrodesis has generally shown to improve function and quality of life with excellent patient satisfaction, but continuing complications warrant the need for continued research into improved approaches [6-8]. A major complication of hind foot or ankle fusions includes delayed union which extends the time patients spend being non-weight bearing, immobilized, and off-work for jobs requiring standing. Non-union in hind foot or ankle situations can lead to revision surgery to obtain fusion. This frequently requires removal of prior hardware, use of much more extensive incisions or dissection and internal fixation, permanent bracing or gait aide use, and a potentially longer time to achieve union than often required by primary fusion [9]. Any delay in union can lead to excessive motion about the fusion site causing bone erosion and loss as well as sclerosis making further surgery very difficult and unpredictable. Finally, delayed or non-union increases the cost of medical care by requiring re-operation (e.g., increased financial cost associated with the surgery, anesthesia time, operating room product costs) and time off work (e.g., social time lost, work income/vacation/ sick leave time lost).
New approaches should focus on early and lasting fusion of bone with minimal complications. A traditional approach to achieving fusion relies on the use of autograft, which provides osteoconductive, osteoinductive, and osteogenic properties, i.e., the three critical factors associated with successful fusion [10]. The disadvantages of autografts include additional pain at the second surgery site, the potential for donor-site morbidity, limited quantity, and the fact that the health of the bone from the donor site is limited by the patient’s health. As an alternative, a new allograft with living cellular bone matrix was recently developed, V-CBM. Like autograft, it provides all three of these properties necessary for fusion while also avoiding the limitations of autograft. The allograft tissue containing viable bone cells is recovered, carefully processed, and then cryopreserved in a solution developed to maintain bone cell viability. V-CBM also contains demineralized bone matrix (DBM) in addition to the viable cortico-cancellous bone matrix. The lineage committed living bone cells are thus committed to forming bone matrix. V-CBM can be thawed in ≤ 5 minutes which optimizes cell viability while also reducing time spent on preparation in the operating room. Preclinical research suggests bone cells could potentially improve fusion over MSCs by remaining in the defect site longer [11] and providing a faster and higher degree of bone deposition [12]. However, there have not been any clinical studies published on the use of V-CBM in foot and ankle arthrodesis procedures making generalizations to a clinical setting difficult. The purpose of this case series is to provide the first such published evidence of V-CBM in a variety of foot and ankle cases.
Methods
All cases were performed by the first author (TS) at the author’s hospital-based practice. Informed consent was obtained from all patients for participation in this case series report. Each of these four cases explored the used V-CBM or VF-CBM (ViviGen Cellular Bone Matrix or ViviGen Formable Cellular Bone Matrix, LifeNet Health, VA Beach, VA) in a different type of foot and ankle fusion procedure with multifactorial treatment. The two different formulations, V-CBM and VF-CBM, contain the same cortico-cancellous living bone cell component. The DBM component in V-CBM is particulate and in VF-CBM is fibers. The two formulations thus have different handling characteristics. Case information can be found in Table 1. Follow-up time ranged from 8 to 20 months with no complications observed in any case. Fusion time ranged from 7.5 to 10 weeks and time to weight bearing ranged from 2 to 3 months. Each patient underwent general anesthesia with endotracheal intubation and single injection popliteal and saphenous nerve block. Positioning was in the supine position with a gel roll bump placed under the ipsilateral thigh to control physiologic external rotation. All surgeries were performed under thigh tourniquet control with continuous recovery observation and conversion to admission hospitalization in situations where pain control was not adequate to allow discharge home. Large C-arm image intensification was employed for all surgeries.
| Case | Age | Sex | BMI | Procedure | Time to Fusion | Time to Weight bearing | Latest Follow-up | Complications |
|---|---|---|---|---|---|---|---|---|
| 1 | 62 | M | 31 | Ankle arthrodesis | 8 weeks | 2 months | 8 months | None |
| 2 | 69 | F | 39 | Double Hindfoot Arthrodesis | 7.5 weeks | 2 months | 14 months | None |
| 3 | 39 | F | 38 | Tibiotalocalcaneal Arthrodesis | 10 weeks | 3 months | 20 months | None |
| 4 | 45 | F | 29 | Revision Lapidus | 7.5 weeks | 2 months | 8 months | None |
Table 1: Case information.
Results
Case 1: Ankle arthrodesis
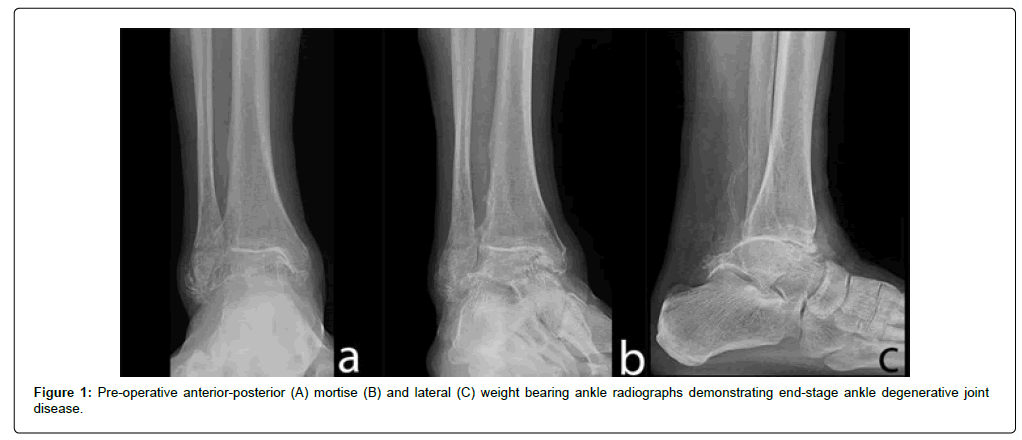
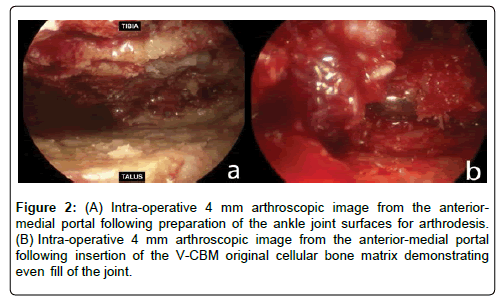
A 62-year-old male presented with end stage ankle arthritis due to chronic lateral ankle instability in the right ankle (Figure 1). The patient complained of debilitating and life altering pain that interfered with quality of life and activities of daily living. Pain consistently scored 7-10 out of 10 on a daily basis using the visual analog scale (VAS). The patient had a body mass index (BMI) of 31 and did not use alcohol or tobacco. In addition to a diabetes comorbidity, he was immunecomprised from taking from tacrolimus and prednisone due to a renal transplant in 2006. Other medication included glucocorticoids, aspirin, and medication for managing diabetes and cholesterol. The patient previously underwent open ankle arthrodesis with five screws in the contra-lateral left ankle 5.5 years prior by another provider that resulted in an asymptomatic fibrous non-union despite 13 weeks of non-weight bearing. Non-surgical medical management with ice/heat, topical liniment, over the counter bracing, 9 inch high lace up boots, and a cane was attempted but did not resolve complaint. Surgery was performed 10 years after initial onset. Tourniquet time was 90 minutes. Standard anterior-medial and anterior-lateral ankle arthroscopic portals, ankle joint synovectomy, debridement of hypertrophic synovium and dense bands of fibrotic tissue were performed with an arthroscopic shaver and radiofrequency wand. Remaining cartilage and sclerotic subchondral bone plate were removed with curettes and arthroscopic acromionizer burr to bleeding subchondral substrate that was further fenestrated with a chondral pick similar to performing a microfracture technique. V-CBM (5 cc) was inserted into ankle joint using a modified syringe as a cannula delivery system. V-CBM passed through the cannula syringe smoothly into ankle joint and was easily manipulated around the ankle joint space (Figure 2). Three percutaneously inserted 6.5 mm cannulated headless compression screws (DePuy Synthes, West Chester, PA) were used for fixation. The patient remained 100% nonweight bearing for 8 weeks then became weight bearing as tolerated in a controlled ankle motion walking boot for an additional 4 weeks. He was compliant with all instructions. Fusion was achieved at 8 weeks. The post-operative VAS dropped to 0 from consistent daily pre-operative scores of 7-10. He returned to activities and shoe gear as desired at 12 weeks. The patient remains free of complications as of the latest followup at 8 months post-operative.
Figure 2: (A) Intra-operative 4 mm arthroscopic image from the anteriormedial portal following preparation of the ankle joint surfaces for arthrodesis. (B) Intra-operative 4 mm arthroscopic image from the anterior-medial portal following insertion of the V-CBM original cellular bone matrix demonstrating even fill of the joint.
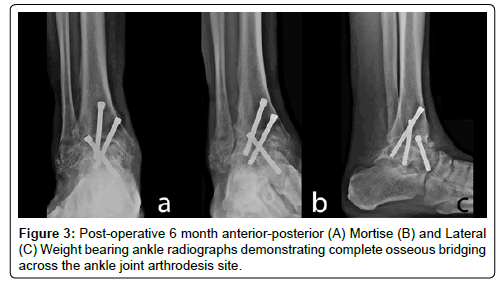
With known non-union of the other ankle, despite it not being painful, that was performed with more internal fixation and an open extensive surgery dissection, it was critical to achieve a solid ankle fusion through a minimally invasive approach. Accordingly, the arthroscopic approach employed included limited dissection, thus preserving vascular supply to bone and tissues, but it appeared V-CBM improved the speed and quality of arthrodesis (Figure 3). The headless compression screws were very sound.
Case 2: Double hindfoot arthrodesis
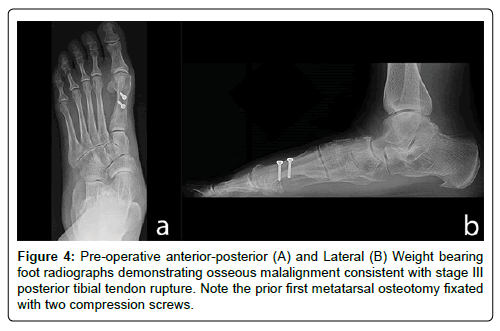
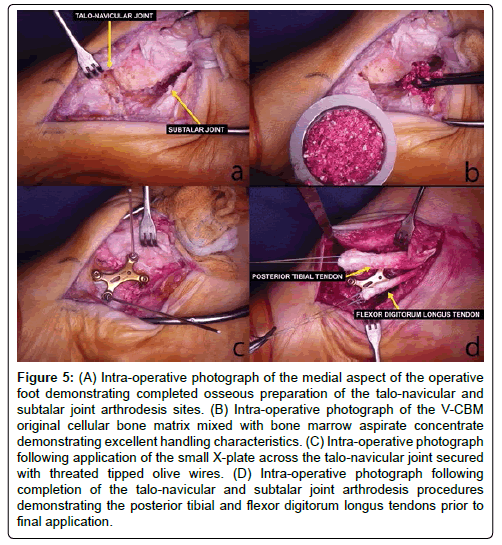
A 69-year-old female presented with a stage III posterior tibial tendon rupture on the left side (Figure 4). The severe collapse of her medial longitudinal arch made shoe gear selection limited and required a gait aide (cane) for daily use. Debilitating and life altering pain that had progressively worsened over previous 10 years’ time interfered with quality of life and activities of daily living. Her pain scored 4 out of 10 at rest and 9 out of 10 during activity using a VAS assessment. The patient had a BMI of 39 and did not use alcohol or tobacco. Comorbidities included fibromyalgia, osteopenia, hypothyroidism, and hypercholesterolemia. Medication included cyclobenzaprine, tramadol, and management for thyroid hormone replacement and blood pressure. Failed non-surgical management included ice/heat, massage, shoe gear changes, activity restrictions, gait aide (cane), in-shoe podiatric orthotics and UCBL device, over-the counter and custom ankle bracing, transcutaneous electrical nerve stimulation (TENS), and ultrasound. Surgery was performed 10 years after onset (Figure 5). Tourniquet time was 131 minutes and the spring ligament complex had been completely ruptured. Medial approach “double arthrodesis” of the talo-navicular and subtalar joints was performed in a standard manner. A small 2.4/2.7 mm VA X-plate with 2.7 mm screws and a 2-hole straight 2.4/2.7 mm VA fusion plate were used for talonavicular joint fusion. Two 6.5 mm cannulated headless compression screws (DePuy Synthes, West Chester, PA) were used for subtalar arthrodesis. Bone marrow aspirate (BMA) was aspirated from the ipsilateral calcaneus, concentrated, and added to 10 cc of V-CBM. The BMA+V-CBM mixture was grafted into talo-navicular and subtalar joints. Bone-tendon procedures included peroneus brevis intra-muscular recession lengthening to reduce valgus pull of this tendon, flexor d igitorum longus tendon transfer secured to the talonavicular plate fixation as an anchor, posterior tibial tendon tenosynovectomy, debridement, and Kidner-type advancement performed.
Figure 5: (A) Intra-operative photograph of the medial aspect of the operative foot demonstrating completed osseous preparation of the talo-navicular and subtalar joint arthrodesis sites. (B) Intra-operative photograph of the V-CBM original cellular bone matrix mixed with bone marrow aspirate concentrate demonstrating excellent handling characteristics. (C) Intra-operative photograph following application of the small X-plate across the talo-navicular joint secured with threated tipped olive wires. (D) Intra-operative photograph following completion of the talo-navicular and subtalar joint arthrodesis procedures demonstrating the posterior tibial and flexor digitorum longus tendons prior to final application.
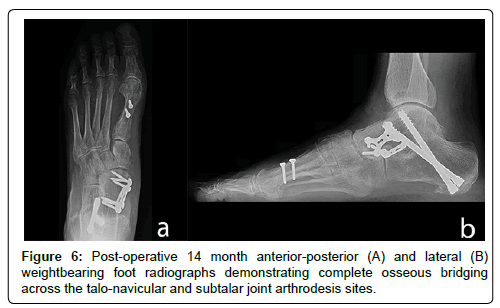
The patient demonstrated fusion at 7.5 weeks and was weight bearing at 2 months post-operative. She was compliant with all instructions. Pain during activities decreased from a pre-operative VAS 9 to a post-operative 1-2 with just a general achiness. A speedy and complete arthrodesis of the talo-navicular and subtalar joint was achieved and remained free of complications at the most recent, 14 month post-operative follow-up (Figure 6). The additional tendon procedures allowed for medial restraint to support the deltoid ligament complex (flexor digitorum longus transfer, posterior tibial tendon advancement) and to reduce valgus pull across hindfoot (peroneus brevis tendon lengthening).
Case 3: Tibiotalocalcaneal arthrodesis
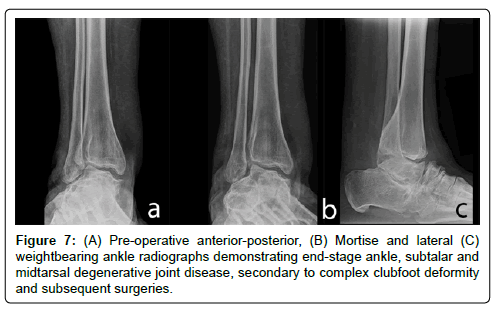
A 39-year-old female presented with end stage degenerative joint disease on the right ankle/subtalar joint due to multiple prior surgeries for clubfoot deformity (Figure 7). The patient was morbidly obese with a BMI of 39, bipolar, depressed, and had a pain contract requiring periodic narcotic monitoring by her primary care provider. She took glucocorticoids, anti-seizure or mood-altering medication, and blood pressure medication. Her pain scored 4 out of 10 at rest and 9 out of 10 during activity using a VAS assessment. She did not use alcohol or tobacco. Failed conservative medical care included use of antiinflammatory medication, glucocorticoids taken orally and also injected into ankle/subtalar joints, topical liniments, ice/heat, and physical therapy. Mechanical controls were also tried with multiple bracing attempts, wheelchair, and intermittent crutch use. The patient had a left lower leg below knee amputation prosthesis following amputation nine years ago for failed ankle replacement. A salvage alternative to below knee amputation was attempted here.
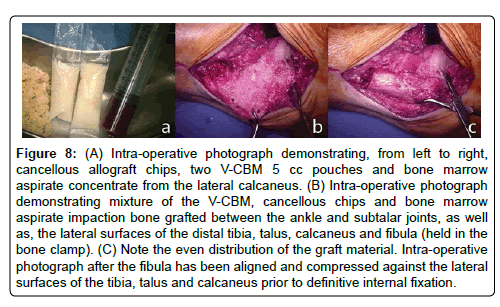
Surgery was performed 4.5 years after onset (Figure 8). A lateral transfibular approach was taken to the ankle and subtalar joints. The joint resection was performed with hand instruments (curettes, osteotomes) and power instruments (rotary burr, drill) to the viable cancellous bone substrate. Two 5 cc syringes of V-CBM were grafted into exposed bone surfaces and the osseous defect and notably remained in place even after irrigation. Calcaneal fixation was achieved using 13 mm diameter, 150 mm length Expert Cannulated Hindfoot Arthrodesis Nail (DePuy Synthes, West Chester, PA) and 6 mm diameter locking screw and spiral blade. Posterior soft-tissues were maintained on the fibula allowing it to be used as an onlay graft that was secured to the tibia and calcaneus with 3.5 mm cortical screws with washers.
Figure 8: (A) Intra-operative photograph demonstrating, from left to right, cancellous allograft chips, two V-CBM 5 cc pouches and bone marrow aspirate concentrate from the lateral calcaneus. (B) Intra-operative photograph demonstrating mixture of the V-CBM, cancellous chips and bone marrow aspirate impaction bone grafted between the ankle and subtalar joints, as well as, the lateral surfaces of the distal tibia, talus, calcaneus and fibula (held in the bone clamp). (C) Note the even distribution of the graft material. Intra-operative photograph after the fibula has been aligned and compressed against the lateral surfaces of the tibia, talus and calcaneus prior to definitive internal fixation.
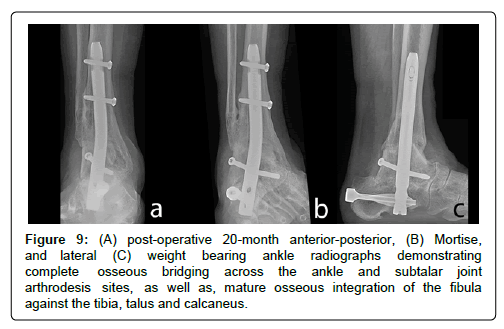
The patient demonstrated fusion at 10 weeks and was weight bearing at 3 months post-operative. Pain during activities decreased from a preoperative VAS 10 to a post-operative 4 in the midfoot/forefoot and 0 in the hindfoot/ankle. The patient does not use brace, is able to use offthe- shelf shoe gear, and ambulates without gait aide. There have been no complications after 20 months post-operative follow-up (Figure 9).
Figure 9: (A) post-operative 20-month anterior-posterior, (B) Mortise, and lateral (C) weight bearing ankle radiographs demonstrating complete osseous bridging across the ankle and subtalar joint arthrodesis sites, as well as, mature osseous integration of the fibula against the tibia, talus and calcaneus.
Case 4: Revision lapidus
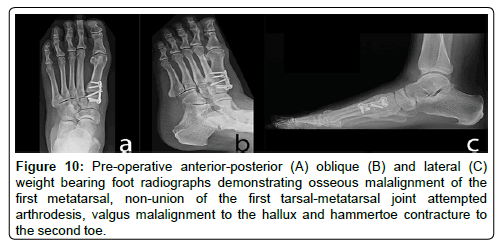
A 45-year-old female presented with symptomatic nonunion of the left first tarsal-metatarsal (TMT) joint (Figure 10). The patient had hypercholesterolemia and was on lisinopril. Her pain scored 4 out of 10 at rest and 9 to 10 out of 10 during activity using a VAS assessment. She had a BMI of 29 and did not use alcohol or tobacco. The patient previously underwent a modified Lapidus first TMT joint arthrodesis by an outside provider with modified McBride bunionectomy for symptomatic moderate hallux valgus with metatarsus primus varus. She was 100% non-weight bearing for 9 weeks and then partial weight bearing for 4 weeks in a controlled ankle motion boot. There was nonunion and external bone growth developed into a second hammertoe. External bone stimulation was used post-operative. In addition to the failed surgery, ice/heat, massage, shoe gear changes, activity restrictions, gait aide (cane), in-shoe podiatric orthotics and UCBL device, over-the counter and custom ankle bracing, TENS, and ultrasound were tried.
Figure 10: Pre-operative anterior-posterior (A) oblique (B) and lateral (C) weight bearing foot radiographs demonstrating osseous malalignment of the first metatarsal, non-union of the first tarsal-metatarsal joint attempted arthrodesis, valgus malalignment to the hallux and hammertoe contracture to the second toe.
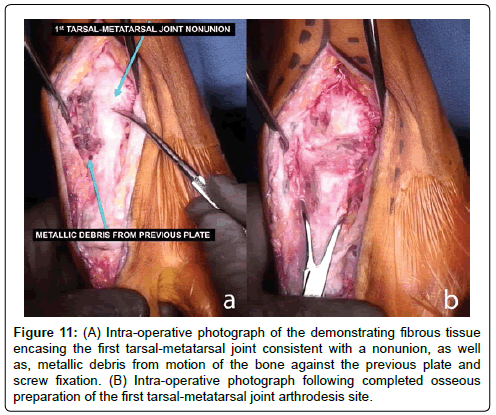
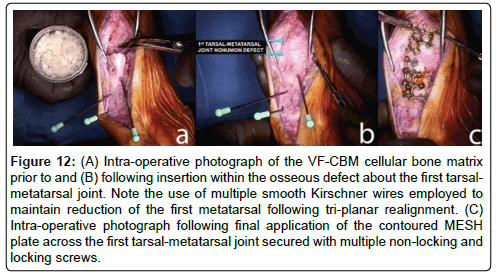
Revision surgery was performed 8 months after the failed first surgery. Tourniquet time was 145 minutes. Prior plate/screws removed with metallic debris in soft-tissues were noted. The nonunion at the first TMJ was very fibrous and required resection of an additional 6 mm from both sides of joint leaving a 1.8 cm defect (Figure 11). Five cc of VGF-CBM was pressed fit into the exposed bone surfaces and osseous defect and again remained in place even after irrigation (Figure 12). The first metatarsal was realigned in frontal, sagittal, transverse planes and stabilized with multiple smooth temporary Kirschner wires. Contoured VA MESH plate (DePuy Synthes, West Chester, PA) with 2.4 and 2.7 mm screws employed to span the arthrodesis site with stout fixation. The 1st metatarsal head had articular cartilage erosion centrally with stiff first metatarsal-phalangeal joint. This was treated using an Akin- Moberg osteotomy to hallux proximal phalanx fixated with a 3.5 mm compression screw. A second toe proximal interphalangeal arthrodesis with Hammerlock 2 was performed.
Figure 11: (A) Intra-operative photograph of the demonstrating fibrous tissue encasing the first tarsal-metatarsal joint consistent with a nonunion, as well as, metallic debris from motion of the bone against the previous plate and screw fixation. (B) Intra-operative photograph following completed osseous preparation of the first tarsal-metatarsal joint arthrodesis site.
Figure 12: (A) Intra-operative photograph of the VF-CBM cellular bone matrix prior to and (B) following insertion within the osseous defect about the first tarsalmetatarsal joint. Note the use of multiple smooth Kirschner wires employed to maintain reduction of the first metatarsal following tri-planar realignment. (C) Intra-operative photograph following final application of the contoured MESH plate across the first tarsal-metatarsal joint secured with multiple non-locking and locking screws.
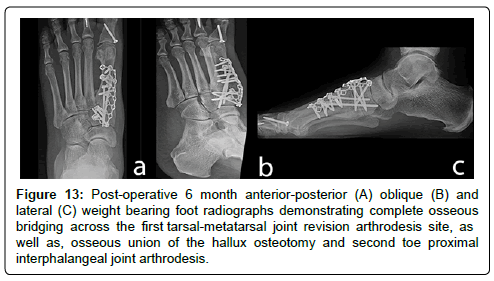
The patient demonstrated fusion at 7.5 weeks and was weight bearing at 2 months post-operative (Figure 13). Pain during activities decreased from a pre-operative VAS 9 to a post-operative 0-1 with great toe stiffness/arthritic pains after activities as only symptomatic area. The patient had very high expectations and was fearful of having her other foot operated on due to her complicated recovery involving two surgeries to her left foot to achieve a quality result. There have been no complications observed as of 8 months post-operative.
Figure 13: Post-operative 6 month anterior-posterior (A) oblique (B) and lateral (C) weight bearing foot radiographs demonstrating complete osseous bridging across the first tarsal-metatarsal joint revision arthrodesis site, as well as, osseous union of the hallux osteotomy and second toe proximal interphalangeal joint arthrodesis.
Discussion
The results of these cases suggest that the use of V-CBM and VFCBM may be an effective approach for multiple types of foot and ankle bone fusion procedures. These results cannot be generalized but do support continued research into the use of a living bone cell containing matrix for arthrodesis procedures. Initial observations of V(F)-CBM suggest that preparation is simple with ≤ 5 minutes required for thawing, a 2 hour window to use before implantation, mixes well with autogenous BMA, is easy to mix with cancellous bone chips if additional structure is necessary, while also accepts being impaction bone grafted as well. V-CBM contains demineralized bone particulate which provides easy handling for tight bone voids. V(F)-CBM can be molded and shaped to a defect due to the putty-like consistency provided by interconnected demineralized bone fibers that allow this allograft to hold its form. Furthermore, the volumes available are ideal for foot and ankle surgery indications from primary first metatarsalphalangeal fusions to extensive revision hindfoot and ankle fusions with large bone defects. The biggest limitation of this case series was the small sample size. There was only one patient described for each type of procedure, though four different case types were covered. Additionally, in support of transparency, one author (BS) is an employee of LifeNet Health, the non-profit organization that invented V-CBM. All patient outcomes were evaluated solely by the practitioner minimalizing any potential for bias.
Conclusions
While clinical guidance cannot be provided based on this small series, these outcomes do provide an informative view of a new approach to ankle and hind foot arthrodesis using V-CBM and support additional research with a larger sample group including multiple surgeons for additional foot and ankle surgical procedures.
Declarations
Acknowledgements
Special thanks to Julie McLean, PhD (LifeNet Health) for writing assistance.
Conflict of interest
TR is a consultant for DePuy Synthes and received support for this work. BS is an employee of LifeNet Health, the non-profit organization that processes ViviGen.
References
- Best MJ, Buller LT, Miranda A (2015) National trends in foot and ankle arthrodesis: 17-Year analysis of the national survey of ambulatory surgery and national hospital discharge survey. J Foot Ankle Surg 54: 1037-1041.
- Yasui Y, Hannon CP, Seow D, Kennedy JG (2016) Ankle arthrodesis: A systematic approach and review of the literature. World J Orthop 7: 700-708.
- DeVries JG, Scharer B (2015) Hindfoot deformity corrected with double versus triple arthrodesis: Radiographic comparison. J Foot Ankle Surg 54: 424-427.
- Burns PR, Dunse A (2017) Tibiotalocalcaneal arthrodesis for foot and ankle deformities. Clin Podiatr Med Surg 34: 357-380.
- Hamilton GA, Mullins S, Schuberth JM, Rush SM, Ford L (2007) Revision lapidus arthrodesis: Rate of union in 17 cases. J Foot Ankle Surg 46: 447-450.
- Esparragoza L, Vidal C, Vaquero J (2011) Comparative study of the quality of life between arthrodesis and total arthroplasty substitution of the ankle. J Foot Ankle Surg 50: 383-387.
- Dalat F, Trouillet F, Fessy MH, Bourdin M, Besse JL (2014) Comparison of quality of life following total ankle arthroplasty and ankle arthrodesis: Retrospective study of 54 cases. Orthop Traumatol Surg Res 100: 761-766.
- Fuchs S, Sandmann C, Skwara A, Chylarecki C (2003) Quality of life 20 years after arthrodesis of the ankle. J Bone Joint Surg Br 85: 994-998.
- Overley BD, Rementer MR (2017) Surgical complications of ankle joint arthrodesis and ankle arthroplasty procedures. Clin Podiatr Med Surg 34: 565-574.
- Khan WS, Rayan F, Dhinsa BS, Marsh D (2012) An osteoconductive, osteoinductive, and osteogenic tissue-engineered product for trauma and orthopaedic surgery: How far are we? Stem Cells Int 2012: 1-7.
- Tortelli F, Tasso R, Loiacono F, Cancedda R (2010) The development of tissue-engineered bone of different origin through endochondral and intramembranous ossification following the implantation of mesenchymal stem cells and osteoblasts in a murine model. Biomaterials 31: 242-249.
- Reichert JC, Quent VM, Noth U, Hutmacher DW (2011) Ovine cortical osteoblasts outperform bone marrow cells in an ectopic bone assay. J Tissue Eng Regen Med 5: 831-844.
Citation: Roukis TS, Samsell B (2018) A New Approach to Ankle and Foot Arthrodesis Procedures Using a Living Cellular Bone Matrix: A Case Series. Clin Res Foot Ankle 6: 274. DOI: 10.4172/2329-910X.1000274
Copyright: © 2018 Roukis TS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 10511
- [From(publication date): 0-2018 - Dec 18, 2025]
- Breakdown by view type
- HTML page views: 9486
- PDF downloads: 1025