Adult Acquired Flat Foot: A New Biomechanical Classification for the Deformity Based on two Point Failure of the Medial Column
Received: 01-May-2018 / Accepted Date: 28-May-2018 / Published Date: 04-Jun-2018 DOI: 10.4172/2329-910X.1000270
Abstract
Adult acquired flatfoot deformity (AAFD) is a common condition which is historically thought to be the result of tibialis posterior tendon dysfunction. As a result, the classification of the disease and its management centres around the state of the tibialis posterior tendon. This classification system has been accepted in the absence of substantial evidence to support it. In this paper, we propose a new biomechanical classification of (AAFD) based on available evidence that not only explains the progression of the disease but also aids clinicians to formulate a management plan.
Keywords: Flatfoot; Tibialis; Planovalgus foot; Synovitis
Introduction
Adult acquired flatfoot deformity (AAFD) is a common condition with a prevalence thought to be 3%-10% [1]. It is more common in females with high BMI [2,3]. The pathogenesis of AAFD is historically thought to be connected to posterior tibialis tendon dysfunction (PTTD). Traditionally the cascade of events was thought to begin with a spontaneous retro-malleolar primary synovitis of tibialis posterior (stage 1). Subsequently, further stretching and tears cause the tendon to elongate. It then becomes unable to perform its function in providing dynamic stabilisation of the medial longitudinal arch, resulting in a flat foot (stage 2).
As the tendon further degrades, it may rupture and in time this produces a fixed plano-valgus deformity (stage 3) [1]. This classification system was first described by Johnson et al. [4] based on their clinical findings of the foot which they then connected to the condition of the tibialis posterior tendon.
In this paper, we propose a new classification system to describe AAFD based on new biomechanical perspectives, which is helping to evolve our current understanding of the disease process.
Clinical Picture
Patients with AAFD, in the early stages, usually present with medial foot pain. Later as the disease progresses, patients develop lateral foot impingement pain and swelling and a subjective feeling of instability. Walking on uneven surfaces may be difficult and there may be a loss of stability in stance. As the medial longitudinal arch collapses, patients are often unable to perform a single stance leg raise [4,5]. In stage 3 the deformity can become fixed and patients develop hindfoot and midfoot arthritis.
Anatomy of the foot and the historically accepted theory for the planovalgus foot
The tendons of the tibialis anterior and posterior muscles attaching on the navicular and on the proximal end of the first metatarsal bones are able to hold the load of the arches very effectively. They are accompanied by the tendon of peroneus longus running lateral to medial across the pedis attaches to the proximal end of the first metatarsal bone. Together, these three tendons form a strong and elastic loop that supports the arch of the midfoot and compensates for the absent medial pillar [6].
Tibialis posterior adducts and supinates the foot and is also a secondary plantar flexor at the ankle. By supinating and adducting the foot, it locks the midfoot and allows its progression into stance [7].
It also has a role in counteracting the peroneus brevis muscle, to achieve an equilibrium of inversion and eversion. Therefore the lack of peroneus brevis function can be an important cause of pes cavus [8]. The tibialis posterior is the second strongest muscle in the leg and the foot. It has an excursion distance of 1-1.5 cm during locomotion. It was traditionally thought that small increases in its length possibly due to synovitis (stage 1) has a significant impact on its function and hence leads to collapse of the medial longitudinal arch (stage 2) [8].
The final result of this deformity consists of planus, hindfoot valgus and forefoot abduction (stage 3). Fixed joint changes and degeneration are a later stage phenomenon (stage 3) [4,5,8,9].
The plantar fascia, plantar ligaments and the spring ligaments also have paramount roles in supporting the arches and all of these fail prior to collapse of the medial longitudinal arch [6]. The plantar fascia has threefold strength in supporting the medial arch when compared to the tibialis posterior. The intrinsic muscles are also thought to play a role in supporting the arches [6,10].
Challenging the existing theory
Within the foot and ankle community the expression, Tibialis posterior insufficiency is still widely used to describe patients with painful AAFD. Indeed, classical teaching insists that the planovalgus foot can only occur as a result of the failure of the tibialis posterior to act effectively. For this reason, many people still focus on the tendon when addressing this problem surgically. The progression through the stages of PTTD as Johnson et al. described has however never been demonstrated in an anatomical or cadaveric study. There has been a long standing assumption that the disease starts with the foot in neutral posture and that with disease progression, planovalgus deformity then develops. However, the development of PTTD and painful AAFD has been well described in patients with pre-existing painless flat feet. In fact, there are case series in the literature that only include pre-existing painless AAFD [11,12]. It has been shown that 70% of patients present with unilateral symptomatic PTTD have contra lateral painless planovalgus, suggesting that the symptomatic foot was already planus prior to the onset of symptomatic tibialis posterior tendon synovitis and a painful AAFD [13].
It is well known that cavus feet can also develop valgus impingement pain. This has been described as pes cavus with planus where the foot has an overall posture of cavus but the overriding symptoms are that of planus [7.17]. We accept, however, that the biomechanically disadvantaged planus foot is more likely to progress to instability which explains its higher incidence in this group. Johnson and Strom’s original description contains no actual data and no subsequent publications has questioned the inter and intra observer reliability and the reproducibility of their system or even how it might help with clinical decision making. Stage 2 disease in their classification is a combination of clinically definable components: tarso-metatarsal instability, fixed supination deformity, tight gastrocnemius/tendoachilles and a failed spring ligament.
To better understand the complexity of stage 2, we believe that these components have to be clinically assessed and described individually [14]. No ultrasound or MRI has study has ever confirmed the elongation of the tibialis posterior tendon. These imaging modalities help image various aspects of the painful planovalgus deformity but are unable to state or quantify the amount of existing synovitis or ascertain the length of the posterior tibialis tendon. MRI and ultrasound investigations have also never been able to connect findings with prognostic evaluation. It is increasingly recognised that the fundamental difference between painless and painful planovalgus lies in the presence or absence of instability.
Static weight bearing radiographs of the foot and ankle are used routinely but cannot determine the presence or absence of instability present at a joint or quantify laxity that may be clinically visible. In painless planovalgus, the foot is biomechanically disadvantaged but the foot is statically restrained and therefore stable and painless with clinically intact ligaments. In painful planovalgus, the foot has lost its two point stability of the medial column as a result of spring ligament failure (largely pronatory/lateral plane failure) and first TMT joint instability (sagital plane failure). Abnormalities of the spring ligament have been shown in all cases with PTTD in symptomatic AAFD, along with abnormalities in the superficial deltoid, interosseous and talocalcaneal ligaments [13].
Stage 1 disease is misrepresented and it is unlikely that spontaneous synovitis is the cause of tibialis posterior tendon failure. In fact studies investigating the incidence of tibialis dysfunction in diseases that cause primary synovitis (such as rheumatoid arthritis) only have an 11% incidence of planovalgus deformity demonstrating that even in the presence of generalised inflamed synovium around the tendons and joints, the foot does not consistently develop a planovalgus deformity. Moreover, much of this data comes from pre anti TNF era where there may have been a higher presence of uncontrolled synovitis in this cohort of patients.
We believe that stage 1 disease is a biomechanical overload synovitis of the tibialis posterior tendon as a result of failure of the spring ligament. The failure of this tendon however does not contribute to the failure of the spring ligament. Evidence for this comes when one looks at the complete absence of tibialis posterior in 32 cases in three different studies. These studies demonstrate that iatrogenic loss of tibialis posterior following transfer for drop foot/pes cavus balancing does not result in a secondary planovalgus deformity or lateral translation of the foot at 75-96 months follow up [15,16].
This confirms that the absence of TP which we equate to as lengthening (as both scenarios effectively de-function the musculotendinous unit) will not automatically lead to planovalgus. The absence of the tibialis posterior tendon does not lead to an increase in the strain in the spring ligament despite changes in the biomechanical profile of the foot from cavus to a more neutral attitude [7]. Recent publications have demonstrated the importance of the static restraints including that of the spring ligament in the development of AAFD [14,17,18].
In a recent study of planovalgus, sequential sectioning the spring ligament, tibialis posterior and the FDL tendon showed that an intact tibialis posterior and FDL did not provide any resistance to lateral translation when the spring ligament was sectioned in isolation. In a further study, correction of the lateral translation deformity was achieved by reconstruction the spring ligament alone [19]. The transfer of the FDL tendon and loading this to mimic the reconstitution of the TP failed to show any significant decrease in resistance to the lateral translation that occurs as a result of the spring ligament failure [17]. This evidence supports our theory regarding the importance of the spring ligament and the importance of its reconstruction by operative measures aimed to address this pathology.
Other cadaveric studies have demonstrated the importance of the spring ligament as the major stabiliser of the arch during mid-stance. Isolated spring ligament sectioning has been shown to create instability in the foot and leads to significant changes in talar, navicular and calcaneal rotations that the loaded tibialis posterior tendon cannot compensate for in a custom frame loaded dynamic model [20]. These studies show that in flat foot deformity the spring ligament complex should be assessed and if necessary repaired when planning a reconstruction. Isolated spring ligament failure in patients has been shown to lead to planovalgus foot without tibialis posterior tendon synovitis [18]. Reconstruction of the spring ligament helps reduce the talonavicular joint and restore the normal foot position [21].
The establishment of a new theory and biomechanical classification of the adult acquired flat foot
Several authors now believe that painful AAFD is fundamentally a mechanical failure of the medial column of the foot at two points: The spring ligament and the first plantar TMT ligament. We seek to establish this 2 point ligament failure of the medial column as the pathogenesis of the disease.
The key primary structure to fail in painful AAFD is the spring ligament. Failure of this structure results in tibialis posterior synovitis, which is a secondary reactive phenomenon to the biomechanical overload of this tendon. The pathogenesis of spring ligament failure is multifactorial and includes both biomechanical and biological factors. Intrinsic factors may include poor collagen states, pre-existing planovalgus foot, race, obesity, age related collagen changes and genetic profile. Extrinsic factors include the tight gastrocnemius, high load activity, obesity and acute overload leading to rupture. This in time leads to a secondary mechanical overload of the medial structures, including tibialis posterior which then results in its inflammation, dysfunction and ultimately its failure/rupture. This is akin to peroneal overload/dysfunction in pes cavus where the peroneus brevis tendon becomes synovitic due to its overload from a biomechanically disadvantaged state.
Johnson et al. description of stage one disease which refers to the posterior tibial tendon developing spontaneous synovitis is highly unlikely. When the spring ligament fails, it results in biomechanical instability in the hindfoot which then induces a secondary tibialis posterior overload synovitis. Posterior tibialis synovitis may occur as a consequence of the tendon’s attempt to compensate for the lack of the spring ligament resulting in its overload or due to the third pulley affect. This early presence of spring ligament failure with the tendon becoming secondarily synovitic has been described as stage 1 disease. Clinically this is identified as retro malleolar tenderness along the course of tibialis posterior.
However, spring ligament failure often goes unrecognised and is not identified as it is predominantly a lateral plane deformity with no clinical evidence of foot planus. At this stage however, spring ligament strain can be clinically detected using the neutral heel lateral push test which is pathognomonic for spring ligament failure/laxity. This is performed by placing the thenar eminence on the anterior process of the calcaneum thus reducing the heel into neutral and placing a lateral force on the forefoot. Lateral translation of the foot can only occur due to a failed/strained spring ligament. This test uses talonavicular axis and the first ray to amplify the strain that develops in the spring ligament medially. This cannot be identified by direct observation of the stance phase foot [11,17]. Operative failure to reconstruct the spring ligament and just debride the tendon can result in higher recurrence rates and fail to address the fundamental problem. Spring ligament laxity in the absence of tibialis posterior tendon synovitis has recently been described by Pasapula et al. as stage 0 disease [14,17].
This is the earliest stage in the pathogenesis of AAFD that can be detected. The spring ligament laxity fails to support the excess medial pressure of the talus head. This initial talus head motion is medial. However, as it progresses it moves inferomedially resulting in the foot pronating excessively around the subtalar axis. Excessive foot pronation is the reciprocal motion of talar head inferomedial subluxation. On weight bearing this excessive pronation is secondarily resisted by the stability of the first ray.
The introduction of stage 0 disease both fundamentally recognises the primary cause of the disease and also has implications on its early and middle management of AAFD. Early diagnosis of spring ligament laxity and early intervention may stop reactive secondary tibialis synovitis and progressive biomechanical failure of the foot.
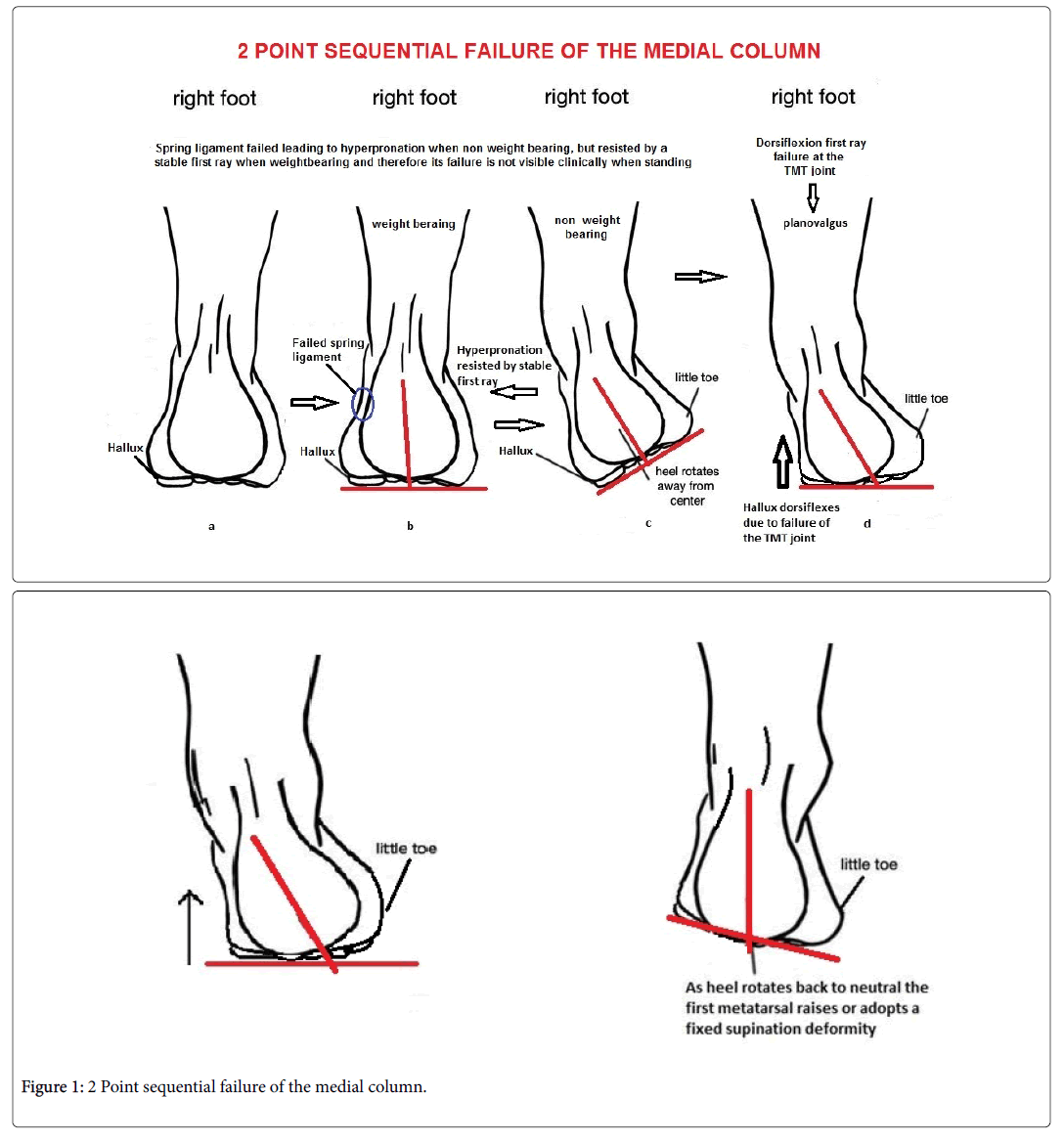
In stage 2 disease spring ligament strain allows excess lateral deviation of the foot and excess subtalar joint pronation. This pronatory movement puts the medial column closer to the ground. This pronatory movement is resisted by the stable first ray which counteracts this to keep the foot in neutral (Figure 1). The first ray TMTJ continues to overload, the first ray becomes dorsally unstable as a result of failure of the first plantar tarso-metatarsal ligament and the plantar fascia. This dorsiflexion failure of the first ray in the presence of spring ligament failure drives and allows forefoot planus and hind foot valgus. The spring ligament strain loses its ability to control the talonavicular axis, its principle medial static restraint and hence allows the first ray dorsiflexion instability to drive the planovalgus deformity (Figure 1).
Both of these points of sequential failure are required to develop planovalgus. This is commonly defined stage 2 deformity is a mixture of complex problems when clinically interpreted. A secondary permanently dorsiflexed first ray can be interpreted as a fixed supination deformity when the hind foot is brought back into neutral. Once the hindfoot deformity becomes fixed, this can be defined as stage 3 disease.
The following diagram depicts the 2 point failure of the medial column
• Spring ligament: Spring ligament failure allows hyper pronation of the forefoot around the subtalar axis Diagram C. This is the essential lesion or primary point of failure. This is resisted by the first metatarsal. However, at this point there is excessive lateral translation (neutral heel lateral push test) however the foot adopts a normal posture.
• The stability of the first ray maintains the foot in neutral as in (B).
• The failure of the spring ligament and then the subsequent failure of the first plantar TMT ligament then allows dorsiflexion destabilisation of the first ray which initially remains stable. Destabilisation of the first ray allows forefoot planus and hindfoot valgus and hence planovalgus. This drives the hindfoot deformity. This is the biomechanical reverse of pes cavus where plantarflexion of the first ray drives hindfoot varus (D).
• The above diagram shows the biomechanical basis of the establishment of a fixed supination deformity and the basis of the hintermans first metatarsal rise sign. As heel rotates back to neutral the fixed dorsiflexed first ray raises or adopts a fixed supination deformity.
Hence we propose a new biomechanical classification to reflect the above which has been outlined below (Tables 1 and 2).
| Stage | Pathology | Tests | Lesion | Clinical findings | Radiographic findings | Gastroctight |
|---|---|---|---|---|---|---|
| 0 flexible | Spring ligament laxity/failure | Lateral push test | Spring ligament failure | No planovalgus Symptoms of instability |
Nil | +/- |
| 1 flexible | Spring ligament laxity/failure and secondary tibialis synovitis | Lateral push test | Spring ligament failure and tibilais posterior has become synovitic | No planovalgus Symptoms of instability |
Nil | +/- |
| 2a flexible | Failure if the first plantar TMT ligament causing first Ray instability with preeisitingSpring ligament failure with | Hicks Test for instability of the first ray Lateral push test |
1st TMT instability | Planovalgus, 1st ray instability leads to hind foot valgus and talonavicular subluxation | Drop in mearys axis Talonavicular uncoverage Radiographicall not possible to distniguid 2a/2b |
+/- |
| 2b | 2A with First ray fixed dorsiflexed | Metatarsal rise sign/Hinterman Lateral push |
TMT fixed dorsiflexed | Planovalgus, swelling laterally and flexible planovalgus with too many toes | Mearys axis dropped Talonavicular uncoverage Calcaneal valgus |
+/- |
| 3 | Fixed hindfoot valgus with failure of the TMT joint | Unable to single stance leg raise (late sign) Lateral push may have disappeared |
Hindfoot fixed valgus | Stage 2 with inability to reduce the hindfoot | All of the above. Not possible to distinguish stage 2 a/b with stage 3 | +/- |
| 3b | Fixed hindfoot valgus with failure of the TMT joint and degeneration of the subtalar joint | Unable to single stance leg raise(late sign) | Hindfoot fixed valgus | Above with pain ful hindfoot and contant pain at rest due to degeneratin | Degeneration of the subtalar joint with the above | +/- |
| 4 | Deltoid failure | Nil | Exacerbated hindfoot valgus | Large valgus deformity | Tibiotalar tilt | +/- |
Table 1: A biomechanical classification.
| Stage | Pathology | Test |
|---|---|---|
| Stage 0 | Spring ligament failure | Lateral push positive |
| Stage 1 | Spring ligament failure and tibialis synovitis | Lateral push positive and retromalleolar tenderness |
| Stage 2 | 1st TMT plantar ligament failure causing and driving hinfoot lagus and hence planovalgus | Positive Dynamic Hicks test Positive Klaue test |
| Stage 2b | First TMT failure and fixed dorsiflexed first ray or fixed supination deformity with hindfoot reduced | Hintermans Positive metatarsal rise sign |
| Stage 3 | Fixed hindfoot valgus | Hindfoot Rigid non correctible |
| Stage 3b | Fixed hindfoot valgus with degeneration | Hindfoot rigid Tender and non-correctible |
| Stage 4 | Deltoid failure | Excess valgus |
Table 2: Simplified Classification.
This modification of the classification system acknowledges the mandatory secondary point of failure of the TMT joint which must fail to induce planovalgus. This is the second essential lesion which is not represented in early classification systems. This can currently be assessed by the dynamic Hicks test for TMT instability. The tibialis posterior synovitis can occur as a reaction to overload at any point is the disease process. We feel that this happens early, and in nearly all our cases of early spring ligament laxity have resulted in some secondary reaction of the tibialis posterior tendon even in the absence of no visible planovalgus.
Whilst the addition of stage 0 disease and reclassification around the spring ligament would allow us to both change our perception of the disease, there are still fundamental flaws in the original classification. We believe the original classification still puts too much emphasis on the TP tendon. We seek to rectify this perception and establish a new biomechanical classification of AAFD whist retaining some aspects of the structure of the original classification system by Johnson et al. to progress its understanding.
The presence of a primary or secondary tight gastrocnemius may be present at any stage. We believe that gastrocnemius tightness or TA tightness may lead to an early heel raise or contribute to excess midfoot strain on the spring ligament. Therefore, it is important to acknowledge that it may be part of a primary contribution to spring ligament failure. Whilst gastrocnemius tightness may be contributory increasing the down force at the TN joint in the second rocker, it may also be a consequence if the hind foot goes into valgus resulting in tightening of the achilles tendon.
Management of AAFD based on the new biomechanical classification
Reagardless of the foot having prior cavus, planus or neutral attitude the fundamental aim of the foot surgery in AAFD is to restore stability. In terms of operative treatment of the spring ligament the best method of reconstructing this is based on cadaveric studies and clinical data. Augmented devices such as the Arthrex internal brace leads to far superior lateral strain resistance than non-augmented reconstructions [17]. FDL transfer alone without spring ligament reconstruction has failed to show improvement in lateral translation of the foot in the static and dynamic cadaveric model [17]. Historic use of isolated FDL transfer has failed to show any improvement. Any operative intervention must restore first ray stability as the second point of correction. We believe that both these interventions restore talonavicular joint reduction and corrects hind foot valgus. The traditional view that hind foot valgus correction can be achieved with an osteotomy is questionable. A shift of 1 cm in high valgus angles if achieved does not change the line of pull of the line of the tendoachillies. If the calcaneum is in mild valgus it is questionable why it should be done at all. We believe that reconstitution of the spring ligament complex helps to improve the talonavicular coverage and hence reduce calcaneal valgus.
We believe that any surgical approach must be aimed at restoring stability to the failed medial column rather than to address planovalgus which may have been pre-existing or address the tendon of the tibialis posterior primarily. The complete absence of the latter has not been shown to induce planovalgus [7]. Many feet with AAFD start in a state of painless planovalgus that are stable. The primary aim should be to restore the integrity of the failed medial column at its two points of failure, the spring ligament and the TMT joint. Secondary procedures that may improve the biomechanical environment of the foot would be in the form a calcaneal osteotomies or lateral column lengthening or a gastrocnemius release. A gastrocnemius release decreases the pressure on the spring ligament during the second rocker or stance phase of the gait cycle. These procedures however in isolation cannot substitute the restoration of two point stability to the medial column and whilst indirectly may augment stability, they do not however by themselves intrinsically achieve it. They may have a role in augmenting the stability once it is achieved. All of these secondary procedures help improve the biomechanical environment of the spring ligament and decrease the overload in the tibialis posterior although there is little medium or long term evidence to support their use in the presence of an augmented reconstruction of the spring ligament. Some studies have shown the isolated use of an FDL transfer and calcaneal osteotomy may achieve a pain free state. However some studies show 50% have reverted back to planovalgus in the long term. Also, this procedure alone does not address first TMT joint instability. Non augmented reconstruction of the spring ligament has been shown not to restore its integrity in a cadaveric model [17]. The authors believe that much of the calcaneal valgus is reduced with spring ligament reconstitution to reduce and hold the medial butress of the talonavicular joint. Addressing the first ray gives additional stability. If the biomechanical profile warrants e.g. high persistent planovalgus or high BMI, this can be addressed with a calcaneal slide or lateral column lengthening which in affect augments the medial reconstruction of the spring ligament.
Secondary operations that improve the biomechanical environment of the foot and prevent secondary failure of the medial column should not be confused with primary procedures that restore the integrity of the medial column. Therefore, the aims of all operative interventions should be:
1. To restore the two point stability to medial column.
a. spring ligament reconstruction/augmentation.
b. restoring plantar flexion and stability to the 1st TMT joint +/- NC joint with fusion of osteotomy.
2. Further improve the biomechanical environment of the spring ligament or augment the medial side if required.
Stage 3 diseases is continued to be addressed with the hind foot triple fusion.
Conclusion
In summary instability is the key to determining if the foot will become symptomatic regardless of the cavus, neutral or planus status of the foot to begin with. It is this 2 point instability that changes the painless planovalgus foot into a painful planovalgus foot. These two states are not discernible with static plain film weight bearing radiographs and must be clinically distinguished.
The essential lesion of stage 2 deformity is the secondary failure of the first plantar tarso-metatarsal ligament inducing dorsiflexion of the first metatarsal and driving hindfoot into valgus when the spring ligament is incompetent. The midfoot instability drives the hindfoot valgus deformity.
The historically accepted classification for AAFD used by Johnson et al. is not validated and erroneously focuses primarily on the tendon. We emphasise the importance on the lateral push test to diagnose the early spring ligament failure and advise on management options to treat AAFD in different stages.
References
- Smyth N, Aiyer A, Kaplan J, Carmody C, Kadakia A (2017) Adult-acquired flatfoot deformity. Eur J Orthop Surg Traumatol 27: 433-439.
- Holmes GB, Mann R (1992) Possible epidemiological factors associated with rupture of the posterior tibial tendon. Foot Ankle 12: 70-79.
- Mueller TJ (1991) Acquired flatfoot secondary to tibialis posterior dysfunction: biomechanical aspects. J Foot Surg 30: 2-11.
- Johnson KA, Strom DE (1989) Tibialis posterior tendon dysfunction. Clin Orthop Relat Res 239: 196-206.
- Bluman EM, Title CI, Myerson MS (2007) Posterior tibial tendon rupture: A refined classification system. Foota Ankle Clin 12: 233-249.
- Kobezda T (2009) The role of the foot in the mechanism of shock absorption. Biomechanica Hungarica 2: 31-38.
- Pecheva M, Devany A, Nourallah B, Cutts S, Pasapula C (2018) Long-term follow-up of patients undergoing tibialis posterior transfer: Is acquired pes planus a complication? Foot 34: 83-89.
- Myerson MS (1997) Adult acquired flatfoot deformity: Treatment of dysfunction of the posterior tibial tendon. Instr Course Lect 46: 393-405.
- Myerson MS, Corrigan J, Thompson F, Schon LC (1995) Tendon transfer combined with calcaneal osteotomy for treatment of posterior tibial tendon insufficiency: A radiological investigation. Foot Ankle Int 16: 712-718.
- Sulowska I, Oleksy Å, Mika A, Bylina D, SoÅ‚tan J (2016) The influence of plantar short foot muscle exercises on foot posture and fundamental movement patterns in long-distance runners, a non-randomized, non-blinded clinical trial. PLoS One 11: e0157917.
- Jahss MH (1982) Spontaneous rupture of the tibialis posterior tendon: Clinical findings, tenographic studies, and a new technique of repair. Foot Ankle Int 3: 158-166.
- Myerson M, Solomon G, Shereff M (1989) Posterior tibial tendon dysfunction: Its association with seronegative inflammatory disease. Foot Ankle 9: 219-225.
- Dyal C, Feder J, Deland J, Thompson F (1997) Tendon disorders of the foot and ankle. Pes planus in patients with posterior tibial tendon insufficiency: Asymptomatic versus symptomatic foot. 18: 85-88.
- Pasapula C, Devany A, Magan A, Memarzadeh A, Pasters V, et al. (2015) Neutral heel lateral push test: The first clinical examination of spring ligament integrity. Foot 25: 69-74.
- Yeap JS, Birch R, Singh D (2001) Long-term results of tibialis posterior tendon transfer for drop-foot. Int Orthop 25: 114-118.
- Mizel M, Temple H, Scranton PJ, Gellman R, Hecht PJ, et al. (1999) Role of the peroneal tendons in the production of the deformed foot with posterior tibial tendon deficiency. Foot Ankle Int 20: 285-289.
- Pasapula C, Devany A, Fischer N, Wijdicks C, Hübner T, et al. (2017) The resistance to failure of spring ligament reconstruction. Foot 33: 29-34.
- Borton DC, Saxby T (1997) Tear of the plantar calcaneonavicular (spring) ligament causing flatfoot. A case report. J Bone Joint Surg Br 79: 641-643.
- Deland JT, Arnoczky SP, Thompson FM (1992) Adult acquired flatfoot deformity at the talonavicular joint: reconstruction of the spring ligament in an in vitro model. Foot Ankle 13: 327-332.
- Jennings MM, Christensen JC (2008) The effects of sectioning the spring ligament on rearfoot stability and posterior tibial tendon efficiency. J Foot Ankle Surg 47: 219-224.
- Orr JD, Nunley JA (2013) Isolated spring ligament failure as a cause of adult-acquired flatfoot deformity. Foot Ankle Int 34: 818-823.
Citation: Pasapula C, Shariff S, Cutts S, West J, Kobezda T (2018) Adult Acquired Flat Foot: A New Biomechanical Classification for the Deformity Based on two Point Failure of the Medial Column. Clin Res Foot Ankle 6: 270. DOI: 10.4172/2329-910X.1000270
Copyright: © 2018 Pasapula C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 9225
- [From(publication date): 0-2018 - Aug 31, 2025]
- Breakdown by view type
- HTML page views: 8188
- PDF downloads: 1037