Allergic Fungal Otitis Media: A Case Series
Received: 14-Jan-2019 / Accepted Date: 05-Feb-2019 / Published Date: 13-Feb-2019 DOI: 10.4172/2161-119X.1000361
Abstract
With recent advances in Immunology and management of allergies, dealing with allergic and eosinophilic disease has gained a lot of importance. We present a case series of allergic fungal ear disease. Like how allergic fungal sinusitis has gained importance in treatment of nasal polyposis, this particular ear disease needs mention and hence this initiative to present the case series.
Keywords: Allergic fungal disease; Chronic suppurative otits media; Oedema
Introduction
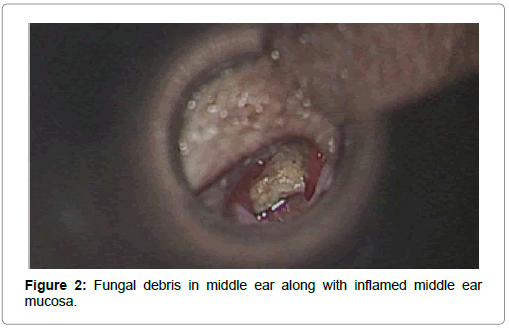
It is a recognised fact that fungal elements in an immunocompetent individual can cause significant mucosal oedema and hence result in sinus-nasal polyposis, which is termed as allergic fungal rhino sinusitis (AFRS). The middle ear, which is also part of the respiratory lining, can react in the same way as the sinus mucosa. In patients with hypersensitivity to fungal elements in the middle ear there is significant oedema, which results in chronic discharging ear. These patients commonly present with earache and mucoid ear discharge. The patients are usually diagnosed as a case of chronic suppurative otitis media tubotympanic disease, which requires surgery. We are submitting a series of three cases who presented with symptoms of CSOM with fungal debris in the middle ear cleft.
Case Report
In our series, we met three such patients. They presented with earache, mucoid ear discharge on and off, hard of hearing on the affected ear. All of the three patients had unilateral chronic suppurative otitis media with large central perforation and copious mucoid discharge with middle ear mucosal oedema with granulation. Audiology done on them revealed a moderate conductive hearing loss on the affected ear (Case 1-53 dB; Case 2-48 dB; Case 3-46 dB).
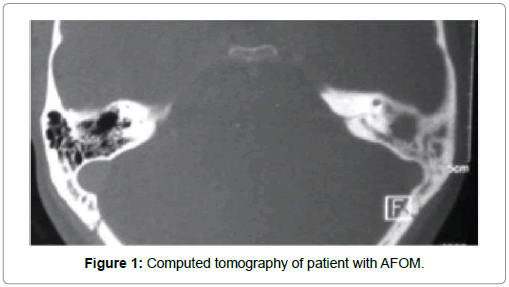
The examination of nose showed a significant mucosal oedema and mucous but no polyps. The radiological evaluation of the nose confirmed our clinical findings. The HRCT of temporal bone showed middle ear mixed dense lesion. We observed ossicular damage in one of the patients (Case 1). The culture was negative. The blood work came out unremarkable except for a slight elevation in eosinophils (Eosinophil / AEC-Case 1-7%/630; Case 2-8%/480; Case 3-7%/651). A remote history of bronchial asthma episode was described in one of the patients previous records (Case 1).
Like we do in all ear procedure, the patient was taken up for mastoidectomy with tympanoplasty after explaining the advantages and the disadvantages of the operation. We chose a post aural route. We harvested the temporalis fascia for grafting. The periosteum was incised and the lateral canal skin flap elevated. We did a posterior meatotomy, visualized the tympanic membrane.
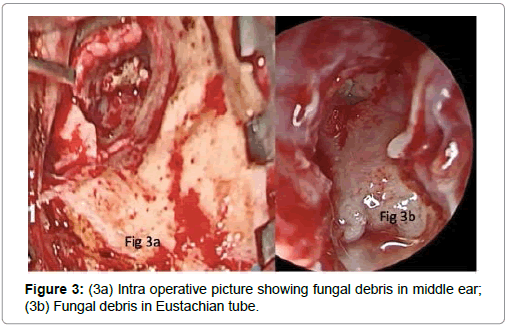
In the first patient (Case 1) there was huge fungal ball in the hypotympanum and attic. They were delivered out and complete mastoidectomy was done. Aditus patency was achieved after removing polypoidal tissue and granulation in the middle ear and mastoid antrum. The eroded incus was removed and augmented type 3 tympanoplasty was completed with underlay temporalis fascia grafting.
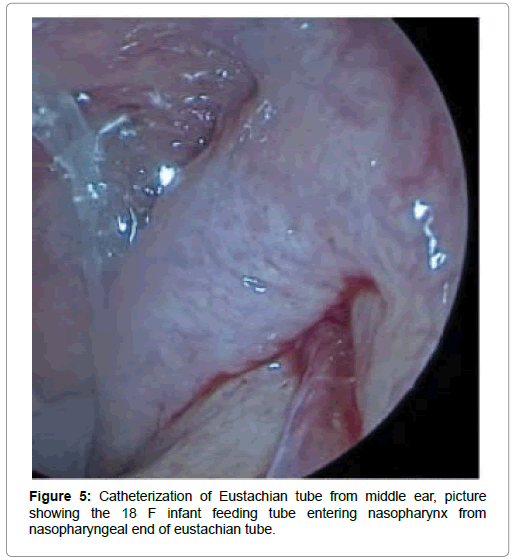
In the second patient (Case 2) there was significantly more mucous and glue which was suctioned out. The amount of fungal debris was also significantly higher even extending into the Eustachian tube with significant middle ear polypoidal changes. In order to obtain complete clearance, we catheterized the Eustachian tube with infant feeding tube (8F), visualized the transit endoscopically into the nasopharynx and flushed the Eustachian tube with saline. The entire procedure was done under vision so no debris was left behind. The surgery was completed with underlay temporals fascia grafting.
In the third patient (Case 3) mucoid discharge was present along with fungal debris with polypoidal middle ear and minimal granulation, which were removed and the same procedure as in case 2 was completed.
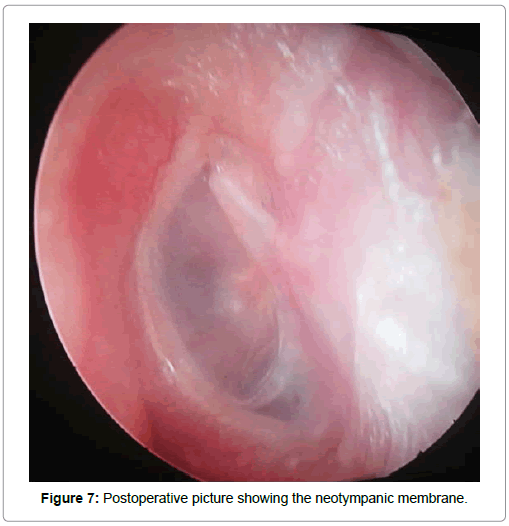
The wound was closed in layers with 3-0 Vicryl and 3-0 ethylene. The membrane was seen 3 weeks postoperatively and patient had good hearing improvement. The patient was on a tapering dose of steroids for 3 weeks. All the patients are on regular follow up and are doing well post operatively (Table 1).
| Case 1 | Case 2 | Case 3 | |
|---|---|---|---|
| Presenting complaint | Pain, discharge , hard of hearing | Discharge, ear block | Discharge, intermittent ear block |
| Clinical exam | Large CP, Mucoid discharge, Polyp | Large CP, Mucoid discharge | Large CP, Mucoid discharge |
| PTA of the affected ear | 53dB | 48dB | 46dB |
| HRCT | Middle ear soft tissue, Incus erosion | Middle ear soft tissue with ET block | Minimal ME soft tissue |
| Per Op | Fungal debris in the middle ear, anterior attic,Aditus and antrum with Granulation tissue and eroded incus (long process) | Fungal debris in the anterior attic extending into the eustachian tube anterior attic space with minimal granulation tissue in the middle ear | Fungal debris in the epitypanum and glue |
| Technique | Mastoidectomy with augmented type3 tympanoplasty with good saline wash | Mastoidectomy with eustachian tube catheterisation and thorough saline wash | Mastoidectomy and saline wash |
| Post op care | Nasal steroid spray and tapering dose of oral prednisone and Budesonide inhaler | Steroid spray and oral tapering dose of prednisone | Steroid spray and oral tapering dose of prednisone |
| Eosinophil/AEC | 7%/630 | 8%/480 | 7%/651 |
Table 1: Series of three cases who presented with symptoms of CSOM with fungal debris in the middle ear cleft.
Discussion
The concept of fungal antigens reaction to the respiratory epithelium has been of great interest in the recent years. The immunological reaction and hypersensitivity cascade that results in fungal ball formation in the sinus cavity is not a new theory. All our cases in this series had a tendency to occupy the anterior attic space where the goblet cells are maximum in the ear. The mucoid discharge was copious in all the three cases. Otopolyposis has been reported previously in a patient with Samter’s triad and another with chronic eosinophilic otitis media in 2009 and 2015, respectively [1,2] which was seen in all three cases.
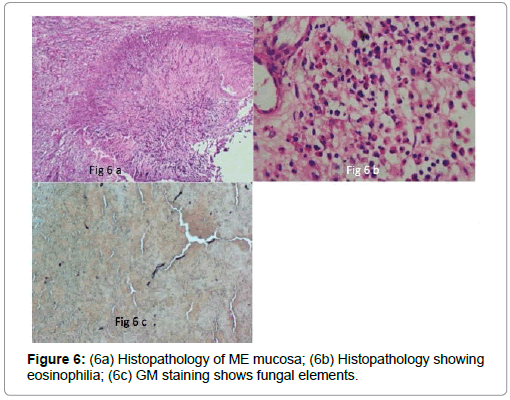
Eosinophilic otitis media (EOM) is an intractable disease characterised by a remarkably viscous effusion and accumulation of numerous eosinophils [3]. Postoperative histopathology and staining determined, our initial diagnosis of eosinophilic and allergic fungal middle ear disease.
This brings us to the concept of allergic reaction of the middle ear mucosa to the fungal antigens, which have traversed the Eustachian tube or got implanted in the middle ear due to exposure because of the perforation. Patients with asthma have a higher predisposition as the T helper dominant predisposition cause ascending inflammation through the Eustachian tube and can cause middle ear eosinophilic inflammation and secretions [4].
The fungal elements coming in contact with the middle ear mucosa is not just enough to start the inflammatory cascade as it is now believed to be multifactorial including mucosal damage and IgE-mediated response [5]. Like in allergic fungal rhino sinusitis the concept of getting rid of the causative antigens that are the fungal elements becomes the prime aim of the surgical procedure. This includes thorough saline wash of the middle ear cleft after standard mastoidectomy procedure. As mentioned earlier, one of the patients (Case 2) required Eustachian tube intubation with an infant feeding tube (8F) for a thorough clearance of the disease from the middle ear cleft. Thick mucoid effusion resembling nasal allergic mucin was encountered. Debris was noted within the antrum and mastoid cavity like it was reported in the work of Azadarmaki et al. [6] (Figures 1-3).
We suggest all patients presenting with excessive mucoid discharge with large central perforation should have a good middle ear cleft wash with normal saline. These groups of patients were termed as allergic fungal otitis media/eosinophilic otitis media. A patient who shows otitis media with effusion or chronic otitis media with eosinophil- dominant effusion (major criterion) and with two or more among the highest four items (minor criteria-middle ear polyposis, sinusitis-unilaterally or bilaterally, granulation tissue, ossicular damage) can be diagnosed as having EOM [3] and with fungal debris in the cavity can be precisely termed as allergic fungal otitis media (AFOM) (Figures 4-6).
The histopathological findings of AFOM are reminiscent of allergic fungal rhinosinusitis (AFRS) and suggest a similar pathophysiology. Optimal treatment in these instances may require a combination of surgical debridement and medical management. AFOM should be considered in the differential diagnosis of chronic otitis media, particularly in the presence of fungal debris, aural polyps and thick otorrhea [7].
The histological finding should have suggested an allergic reaction with rich infiltration of eosinophils in the middle ear with few fungal elements, but cultures were not fruitful, although fungal staining with GMS stains revealed filaments unlike the work of Chen and Chiang [8] where no amorphous mucin or fungal hyphae were mentioned in the report which is possible in pure eosinophilic middle ear disease. Culture of middle ear mucous showed no evidence of fungal growth [9]. Hence a positive fungal culture may not always be necessary.
All our patients responded well with standard post-operative mastoid management of antibiotics, analgesics and antihistamines along with a tapering dose of oral steroids (prednisone) [6]. The mean audiological gain was 22 dB post operatively. All the patients were put on long-term nasal steroid sprays to prevent excess mucous production and Eustachian tube related ascending inflammation or allergies in the middle ear. The neomembrane was seen and documented in all the three patients to confirm the success of the outcome (Figure 7).
Fungal mastoiditis is a rare disease entity and occurs almost exclusively in immunocompromised patients. In immunocompetent patients, the disease has only been sporadically reported [10]. Hence we wanted to share our series.
Conclusion
This disease brings us to the gentle reminder of old teaching-to always look into the nose and paranasal sinuses before treating any ear disease. Allergic fungal otitis media is on the rise and we will be seeing more such patients in the future. The treatment guidelines for this ear disease have to be formed like other ear diseases treatment protocols that already exist. We suggest thorough middle ear cleft examination and saline wash along with postoperative steroids in tapering dose along with standard post-operative management of a mastoid/middle ear surgery. Long-term Nasal steroid spray and follow up forms the vital cog in the treatment protocol.
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship and/or publication of this article: The authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript.
Funding
The author(s) received no financial support for the research, authorship and/or publication of this article.
References
- Kumar MS, Panella NJ, Magliocca KR, Vivas EX (2016) Otopolyposis with middle ear allergic mucin in a patient with allergic fungal rhinosinusitis. Annals of Otology, Rhinology & Laryngology 125: 862-865.
- Brobst R, Suss N, Joe S, Redleaf S (2009) Bilateral inflammatory aural polyps: A manifestation of samter's triad. Int J Otolaryngol 2: 464-958.
- Lino Y, Tomioka-Matsutani S, Matsubara A, Nakagawa T, Nonaka M, et al. (2011) Diagnostic criteria of eosinophilic otitis media, a newly recognized middle ear disease. Auris Nasus Larynx 38: 456-461.
- Lino Y, Kakizaki K, Saruya S, Katano H, Komiya T, et al. (2006) Eustachian tube function in patients with eosinophilic otitis media associated with bronchial asthma evaluated by sonotubometry. Arch Otolaryngol Head Neck Surg 132: 1109-1114.
- Marple BF (2001) Allergic fungal rhinosinusitis: current theories and management strategies. Laryngoscope 111: 1006-1019.
- Azadarmaki R, Westra W, Prasad S (2015) Eosinophilic mucin otomastoiditis and otopolyposis: a progressive form of eosinophilic otitis media. Ann Otol Rhinol Laryngol 124: 752-756.
- Zhu BZ, Bishop JA, Chien WW (2017) A case of allergic fungal otomastoiditis with aural polyps. Otolaryngology Case Reports 2: 4-6.
- Chen CM, Chiang CW (2013) Allergic fungal otomastoiditis: A case report. Laryngoscope 123: 1040-1042.
- Kim EJ, Catten MD, Lalwani AK (2002) Detection of fungal DNA in effusion associated with acute and serous otitis media. Laryngoscope 112: 2037-2041.
- Ohki M, Ito K, Ishimoto S (2001) Fungal mastoiditis in an immunocompetent adult. Eur Arch Otorhinolaryngol 258: 106-108.
Citation: Ramalingam V (2019) Allergic Fungal Otitis Media: A Case Series. Otolaryngol (Sunnyvale) 9:361. DOI: 10.4172/2161-119X.1000361
Copyright: © 2019 Ramalingam V. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4828
- [From(publication date): 0-2019 - Nov 10, 2025]
- Breakdown by view type
- HTML page views: 3878
- PDF downloads: 950