Research Article Open Access
Are Double-Layer Stents Better than Plastic Stents and Self-Expandable Metal Stents in Palliating Malignant Biliary Obstruction? Meta-Analysis and Systematic Review
Harsha Moole1*, Matthew L. Bechtold2, Micheal Cashman3, Fritz H Volmar3, Sonu Dhillon3, David Forcione4 and Srinivas R Puli31Division of General Internal Medicine, University of Illinois College of Medicine at Peoria, Illinois, USA
2Division of Gastroenterology and Hepatology, University of Missouri, Columbia, Missouri, USA
3Division of Gastroenterology and Hepatology, University of Illinois College of Medicine at Peoria, Peoria, Illinois, USA
4Interventional Endoscopy Services, Gastrointestinal Unit, Massachusetts General Hospital, Harvard Medical School, Boston, Massachusetts, USA
- Corresponding Author:
- Harsha Moole, MD
Department of Internal Medicine
University of Illinois College of Medicine Peoria
530 NE Glen Oak Ave, Peoria, Illinois, 61637, USA
Tel: +1 (309) 655-2730
Fax: 001 (309) 655-2755
E-mail: harsha1778@yahoo.co.in
Received Date: June 18, 2016; Accepted Date: July 27, 2016; Published Date: August 03, 2016
Citation: Moole H, Bechtold ML, Cashman M, Volmar FH, Dhillon S, et al. (2016) Are Double-Layer Stents Better than Plastic Stents and Self-Expandable Metal Stents in Palliating Malignant Biliary Obstruction? Meta-Analysis and Systematic Review. J Gastrointest Dig Syst 6:459. doi:10.4172/2161-069X.1000459
Copyright: © 2016 Moole H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Gastrointestinal & Digestive System
Abstract
Background: Double layer stents (DLS) were designed to overcome the limitations of plastic stents (PS) and self-expandable metal stents (SEMS) in palliating inoperable malignant biliary obstructions (MBO). Aims: Primary outcomes are stent patency period, occlusion rates and adverse events. Methods: Study Selection Criteria: Studies using DLS, SEMS and PS for palliation of patients with inoperable MBO. Data collection and extraction: Articles were searched in Pubmed and Ovid. Statistical method: Pooled proportions were calculated using both fixed and random effects model. Results: Initial search identified 374 reference articles, of which 41 were selected and reviewed. Five studies (N=460) for DLS, SEMS and PS which met the inclusion criteria were included in this analysis. Pooled analysis by fixed effects showed DLS patency to be 118.9 days (95% CI=110.4 to 127.4) compared to 77.4 days (95% CI=70.2 to 84.6) in PS and 170.7 days (95% CI=154.4 to 187.0) in SEMS. Stent occlusion rates in DLS, PS and SEMS group were 8.1% (95% CI=7.1 to 9.0), 37.5% (95% CI=33.8 to 41.1) and 19.9% (95% CI=18.1 to 21.7) respectively. Conclusions: In palliating inoperable MBO patients, DLS seem to be superior to PS. SEMS tend to have higher occlusion rates compared to DLS.
Keywords
Double layer stent; Self-expandable metal stents; Plastic stents; Malignant biliary obstruction; Meta-analysis; Systematic review
Introduction
Malignant biliary obstruction (MBO) occurs as a result of primary neoplasms of pancreato-biliary tract and other local cancers (gall bladder and liver malignancies) that can compress the biliary tract. The local tumors manifest as strictures occluding the biliary tract [1]. The 5 year survival rate of most of these malignancies is less than 5% [2]. These malignancies are often unresectable at the time of presentation, thus making palliation with biliary stents a widely accepted management option [3-6]. Biliary obstruction can cause jaundice, malabsorption, pruritus, anorexia, or cholangitis [7,8]. Endoscopic retrograde biliary drainage (ERBD) with decompression and placement of biliary stents can relieve obstructive symptoms and improve the quality of life [9,10]. Furthermore, biliary stents have lower morbidity than bypass surgery and are often the preferred method for palliation [11-16].
Biliary stents can broadly be classified into plastic stents (PS) and self-expandable metal stents (SEMS). Bore size of the stent plays a key role in stent patency. Smaller bore size leads to early blockade of stent from accumulation of biliary sludge [5]. Diameter of the PS is approximately 10 to 14 Fr compared to the diameter of the SEMS which is approximately 30 Fr after stent deployment. For a long time, PS have been used for palliation, however due to the short patency period, they had to be changed every few months. PS have significantly shorter patency period compared to uncovered self-expandable metal stents (USEMS) [11,12,17,18]. SEMS are relatively more expensive, have an increased susceptibility of tumor ingrowth/overgrowth that leads to stent dysfunction, and are not easily retrievable [19].
As an attempt to upgrade the PS and overcome its limitations, Double Layer stents (DLS) (Olympus, Japan) were developed. They are made of two layers separated by a stainless steel wire mesh. The outer layer is made of polyamide elastomer-this provides rigidity, elasticity and stiffness to ensure easy passage of the stent through a stricture. The inner layer is made of a specially processed fluorinated material that makes the inner surface smoother and provides water repellant properties. These properties would minimize the accumulation of bile or sludge on the inner surface of stent, there by delaying the stent occlusion. DLS has four flaps each on duodenal and distal ends to secure the stent in place [7].
Previous retrospective studies and randomized control trials (RCTs) comparing the efficacy of DLS with other stents showed that DLS had longer patency period and lower risk of occlusion compared to PS, however SEMS had longer patency compared to DLS [7,19-22]. Thus far, there has not been any systematic review article or meta-analysis that looked at the overall efficacy of DLS.
In this meta-analysis and systematic review, we sought to include all the available studies including RCTs and retrospective cohort studies comparing the efficacy of DLS with PS and SEMS in palliation of inoperable malignant biliary obstruction (intrahepatic, hilar, and distal biliary obstruction). Primary outcomes are stent patency periods (number of days the stent is patent) and stent occlusion rates of DLS, PS and SEMS in managing malignant biliary strictures. Secondary outcomes include overall adverse events in all the groups.
Methods
Inclusion criteria
Studies comparing DLS with PS and / or SEMS for palliation in patients with inoperable malignant biliary stricture/obstruction were included in this meta-analysis and systematic review. Studies should have looked at a minimum of two variables that must include stent patency days and adverse events. Patients in the studies should have had a malignant biliary stricture that is either non-resectable (probably due to extensive distant metastasis or vascular invasion) or inoperable (due to other co-morbidities).
Exclusion criteria
Studies without a comparison arm (non-comparison studies) were excluded. Studies that looked at patients with prior radiological biliary procedures, prior biliary surgical procedures, and prior biliary stent placement were also excluded. Patients with American Society of Anesthesiologists (ASA) grade 4 or 5, inability to follow up, duodenal obstruction, potentially benign biliary obstruction were all excluded. Studies that were done on patients receiving chemotherapy were excluded from this analysis. Studies not looking at post-stenting complications and stent occlusion rates were also excluded from the study.
Data collection and extraction
Articles were searched in Medline, PubMed, and Ovid journals, EMABSE, Cumulative Index for Nursing & Allied Health Literature, ACP journal club, DARE, International Pharmaceutical Abstracts, old Medline, Medline non indexed citations, OVID Health star, and Cochrane Central Register of Controlled Trials (CENTRAL). The search was performed for the years 1966 to December 2015. Abstracts were manually searched in the major gastroenterology journals for the past three years. Study authors for the abstracts included in this analysis were contacted when the required data for the outcome measures could not be determined from the publications. The search terms used were Double Layer Stent, self-expandable metal stents, plastic stents, palliation, malignant biliary stricture, patency, occlusion rate, stent migration, mortality, morbidity, complications, metaanalysis, and systematic review. Two authors (HM and SP) independently searched and extracted the data into an abstraction form. Any differences were resolved by mutual agreement. The agreement between reviewers for the collected data was quantified using the Cohen's κ [23].
Definitions
Stent patency is defined as the interval between stent insertion and stent occlusion or stent replacement. Stent occlusion is defined as development of jaundice with biochemical evidence of cholestasis, worsening transaminasemia and/or cholestasis with episodes of fever suggestive of cholangitis.
Follow up period for all the studies included in this analysis was either till patient’s death or stent occlusion or 12 months after first stent placement; which ever occurred first. Survival benefit was assessed using time till death. Time till death is defined as the number of days the patient was alive after the first biliary stent placement as a palliative attempt.
Quality of studies
Clinical trials designed with a control and treatment arms can be assessed for quality of the study. A number of criteria have been used to assess this quality of a study (e.g. randomization, selection bias of the arms in the study, concealment of allocation, and blinding of outcome) [24,25]. There is no consensus on how to assess studies designed without a control arm. Hence, these criteria do not apply to studies without a control arm [25].
Statistical methods
This meta-analysis was performed by calculating pooled proportions. First the individual study proportion of stent patency periods, stent occlusion rates, and overall complications were transformed into a quantity using Freeman-Tukey variant of the arcsine square root transformed proportion.
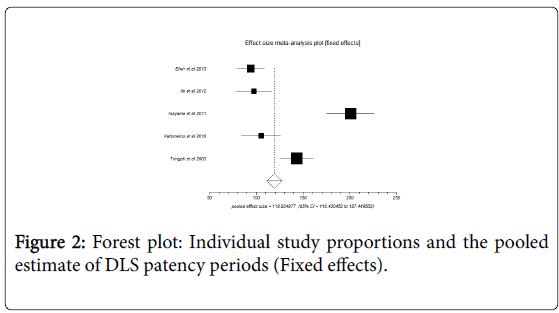
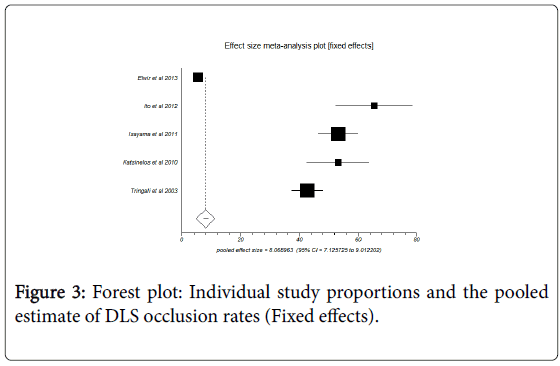
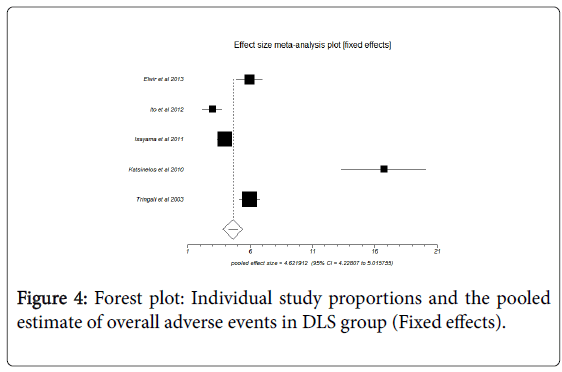
The pooled proportion is calculated as the back-transform of the weighted mean of the transformed proportions, using inverse arcsine variance weights for the fixed effects model and DerSimonian-Laird weights for the random effects model [26,27]. Forest plots were drawn to show the point estimates in each study in relation to the summary pooled estimate. The width of the point estimates in the Forest plots indicates the assigned weight to that study.
The heterogeneity among studies was tested using Cochran’s Q test based upon inverse variance weights [28]. If p value is >0.10, it rejects the null hypothesis that the studies are heterogeneous.
The effect of publication and selection bias on the summary estimates was tested by both Harbord-Egger bias indicator [29] and Begg-Mazumdar bias indicator [30]. Also, funnel plots were constructed to evaluate potential publication bias using the standard error and diagnostic odds ratio [31,32], Microsoft Excel 2013 (Seattle, USA) was used to perform statistical analysis.
Results
Initial search identified 374 reference articles, of which 41 articles were selected and reviewed. Data was extracted from five studies [7,19-22] (N=460) for DLS compared with SEMS and/or PS which met the inclusion criteria.
All the studies are published as full text articles. Figure 1 shows the search results. All the pooled estimates given are estimates calculated by the fixed and random effect models.
Table 1 shows the baseline characteristics of the studies. Of the five studies included in this study, three [20-22] are randomized controlled trials (RCT) and two [7,19] are retrospective cohort studies. The pooled effects estimated by fixed and random effect models were similar.
| No | Study | Type of study | Â Age* | Sex: M/F | Total No of patients | No of patients with DLS | No of patients with SEMS | No of patients with PS | Location of biliary stricture |
|---|---|---|---|---|---|---|---|---|---|
| 1 | Elwir et al.[7] | Retrospective | 66 | 77/37 | 114 | 37 | 44 | 33 | Mixed |
| 2 | Ito et al.[19] | Retrospective | 70 | 44/20 | 64 | 24 | 27 | - | Distal |
| 3 | Isayama et al.[20] | Randomized Prospective | 70 | 63/50 | 113 | 58 | 55 | - | Distal |
| 4 | Katsinelos et al. [21] | Randomized Prospective | 72 | 23/26 | 49 | 24 | - | 25 | Distal |
| 5 | Tringali et al. [22] | Randomized Prospective | 71 | 50/70 | 120 | 60 | - | 60 | Mid to Distal |
Table 1: Basic characteristics of the included studies. *Age: Median age in years, DLS: Double layer stent; SEMS: Self-expandable metal stent, PS: Plastic stent.
The p for chi-squared heterogeneity for all the pooled accuracy estimates was >0.10. This article looked at various outcomes including stent occlusion rates, survival rates, cholangitis episodes etc.
However, most of the studies did not have information on all the variables studied in this meta-analysis. Studies with pertinent information regarding a particular variable were included in calculated the pooled effect of that particular variable.
Stent patency period and stent occlusion rates
Pooled analysis by fixed effects showed DLS patency to be 118.9 days (95% CI=110.4 to 127.4) compared to 77.4 days (95% CI=70.2 to 84.6) in PS and 170.7 days (95% CI=154.4 to 187.0) in SEMS. Bias indicator: Egger bias was 14.71 (95% CI=-11.79 to 41.21) with P=0.17.
Figure 2 shows forest plot of individual study proportions and pooled estimate for DLS patency periods. Percentage of stents occluded in DLS, PS and SEMS group were 8.1% (95% CI=7.1 to 9.0), 37.5% (95% CI=33.8 to 41.1) and 19.9% (95% CI=18.1 to 21.7) respectively.
Figure 3 shows forest plot of individual study proportions and pooled estimate for DLS occlusion rates.
Overall adverse events
Pooled analysis by fixed effects showed the overall adverse events in DLS group, PS group and SEMS group to be 4.62 (95% CI=4.22 to 5.02), 3.44 (95% CI=2.99 to 3.89) and 2.17 (95% CI=1.73 TO 2.61) respectively. Figure 4 shows forest plot of individual study proportions and the pooled estimate of overall adverse events in DLS group (Fixed effects). The adverse events include pancreatitis, cholangitis, perforation, stent occlusion, haemorrhage after Endoscopic retrograde cholangiopancreatography (ERCP), biliary leakage, delayed gastric emptying, myocardial infarction, portal vein thrombosis, pneumonia, need for repeated laparotomy and intra-abdominal abscess.
Discussion
Biliary obstruction is found in most patients with malignancies of the bile-duct system [12,15,33]. However, disease is usually detected in late stages because most patients do not have early symptoms [7,9]. Surgical resection offers the greatest chance of cure for common bile malignancy [7]. Yet, five-year survival rates remain less than 10% and the prognosis is extremely poor [9,34]. Metastatic or locally advanced disease cannot be cured in greater than 80% of patients [12,15,33]. As mentioned above, decompression of biliary system using a biliary stent has proved beneficial in these patients.
SEMS have a longer patency periods compared to plastic stents [11,12,17,18]. Stent diameter plays a key role in stent patency. After deployment, SEMS can expand to a diameter of approximately 30 Fr, whereas the maximum diameter of PS that can be deployed is 10-14 Fr due to the limited diameter of the accessory channel of endoscope. USEMS are associated with an increased tumor ingrowth, easily embedded into the biliary tract, and are difficult to retrieve [11,12,17,18].
Stent occlusion usually occurs due to bio-film formation from accumulation of bacteria and proteins to the inner surface of the stent. This is usually followed by precipitation of biliary contents and eventually clogging the stent. In addition to these mechanisms, tumor ingrowth and outgrowth also contribute to stent occlusion in SEMS [7,35-37]. Double layered stents were developed to overcome the limitations of plastic stents. DLS structure is essentially designed to improve the patency period and to promote easy insertion in to the biliary tract. The inner layer is smooth and has water-repellant properties. This minimizes bile adhesion and accumulation. The outer layer is more rigid and this facilitates smooth insertion. DLS does not have side holes; thereby reducing bile accumulation in the lumen [7]. DLS also have four flaps each on both ends to keep it in place.
A recent study that compared DLS with SEMS and PS showed that DLS might be a cost effective alternative in palliation of malignant biliary obstruction. Their study showed that DLS is superior to PS and are comparable to SEMS. DLS and SEMS had comparable complications [7]. Few studies comparing DLS to SEMS showed that SEMS have a longer patency period [19,20]. Katsinelos et al. [21] showed that DLS and PS are comparable in-terms of stent patency and complication. However, Tringali et al. [22] showed that DLS had longer patency period and lesser occlusion rates compared to PS.
In our meta-analysis, the final outcomes showed that DLS have a longer patency period, lower stent occlusion rates and slightly more adverse effects compared to PS. In a patient with a shorter life expectancy, DLS may be used in place of PS if the cost of the stents are practically comparable. In this meta-analysis, SEMS showed longer patency period and less adverse events compared to DLS. This shows that SEMS could be superior to DLS.
Cost effectiveness of DLS versus PS and SEMS is another area of interest that would determine the practical feasibility of DLS in palliation. In our meta-analysis, we were not able to derive any conclusions in regards to cost effectiveness. This is due to the nonuniformity of cost effectiveness criteria used in the aforementioned studies. Cost-effective analysis must be performed in future RCTs involving DLS. Based on the results of this meta-analysis, which inturn is supported by the conclusions from prior studies, we can conclude that in patients with malignant biliary obstruction receiving palliation with SEMS, DLS may not yet be an equally effective alternative.
There are a few limitations for this study. Different type of stents with slightly variable bore size have been used in these studies. Few studies used trial stents that were not used in another study. The DLS used in all the studies was from ‘Olympus, Japan’ except one study that used a customized DLS [21]. Uncovered metal stent was used in Ito et al. [19] Covered metal stent was used in Isayama et al. [20], Kastinelos et al. compared Tannenbaum stent to DLS [21]. Regular polyethylene plastic stents were used in two studies, Elwir et al. and Tringali et al. [7,22]. The type of malignancy causing the biliary obstruction, stage of the malignancy, presence of metastasis could have all influenced the results. Retrospective cohort studies were included in this metaanalysis along with RCTs.
Strengths of this meta-analysis include the high quality methodology of statistical analysis, high quality methodology used in individual studies, total number of patients included in this analysis (N=460) and homogeneity of data among the individual studies.
Studies with statistically significant positive results tend to be published and cited. Additionally, smaller studies may show larger treatment effects compared to larger studies. This publication and selection bias may affect the summary estimates. The bias can be estimated using Egger bias indicators and the construction of funnel plots, whose shape can be affected by bias. In the present meta-analysis and systematic review, bias calculations both Egger [29] and Begg- Mazumdar [30] bias indicators showed no statistically significant bias. Furthermore, analysis using funnel plots showed no significant publication bias among the studies included in the present analysis.
Conclusions
DLS seem to be superior to plastic stents. DLS remain patent for a longer duration and are less prone to occlusion compared to PS. DLS and PS is comparable in regards to their overall adverse effects. SEMS seem to remain patent for a longer duration and have less adverse effects compared to PS. When the patients were followed up till death, SEMS tend to have higher occlusion rates compared to DLS. DLS might not yet be a standard alternative for SEMS in palliating patients with unresectable MBO. Further RCTs with cost effectiveness analysis could provide more specific guidelines regarding the stent preference.
References
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, et al. (2009) Cancer Statistics, 2009. CA Cancer J Clin59: 225-249.
- Ries LAG, Harkins D, Krapcho M (2005) SEER Cancer Statistics Review, 1975-2003. Bethesda: National Cancer Institute.
- Shepherd HA, Royle G, Ross AP, Diba A, Arthur M, et al. (1988) Endoscopic biliary endoprosthesis in the palliation of malignant obstruction of the distal common bile duct: a randomized trial. Br J Surg 75:1166-1168.
- Smith AC, Dowsett JF, Russell RC, Hatfield AR, Cotton PB (1994) Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet 344:1655-1660.
- Speer AG, Cotton PB, Russell RC (1987)Randomised trial of endoscopic versus percutaneous stent insertion in malignant obstructive jaundice. Lancet 12: 57-62.
- Andersen JR, Sørensen SM, Kruse A, Rokkjaer M, Matzen P (1989)Randomised trial of endoscopic endoprosthesis versus operative bypass in malignant obstructive jaundice Gut 30:1132-1135.
- Elwir S, Sharzehi K, Veith J, Moyer MT, Dye C, et al. (2013) Biliary stenting in patients with malignant biliary obstruction: comparison of double layer, plastic and metal stents. Dig Dis Sci 58:2088-2092.
- Moses PL, Alnaamani KM, Barkun AN (2013) Randomized trial in malignant biliary obstruction: plastic vs partially covered metal stents. World J Gastroenterol 19:8638-8646.
- Raju RP, Jaganmohan SR, Ross WA, Davila ML, Javle M, et al. (2011) Optimum palliation of inoperable hilarcholangiocarcinoma: comparative assessment of the efficacy of plastic and self-expanding metal stents. Dig Dis Sci 56:1557-1564.
- Mukai T, Yasuda I, Nakashima M, Doi S, Iwashita T, et al. (2013) Metallic stents are more efficacious than plastic stents in unresectable malignant hilar biliary strictures: a randomized controlled trial. J HepatobiliaryPancreatSci 20:214-222.
- Knyrim K, Wagner HJ, Pausch J, Vakil N (1993) A prospective, randomized, controlled trial of metal stents for malignant obstruction of the common bile duct. Endoscopy 25:207-212.
- Davids PH, Groen AK, Rauws EA, Tytgat GN, Huibregtse K (1992) Randomised trial of self-expanding metal stents versus polyethylene stents for distal malignant biliary obstruction. Lancet 340:1488-1492.
- Wagner HJ, Knyrim K, Vakil N, Klose KJ (1993) Plastic endoprostheses versus metal stents in the palliative treatment of malignant hilar biliary obstruction. A prospective and randomized trial. Endoscopy 25:213-218.
- Kaassis M, Boyer J, Dumas R, Ponchon T, Coumaros D, et al. Plastic or metal stents for malignant stricture of the common bile duct? Results of a randomized prospective study. GastrointestEndosc 57:178-182.
- Soderlund C, Linder S (2006) Covered metal versus plastic stents for malignant common bile duct stenosis: a prospective, randomized, controlled trial. GastrointestEndosc 63:986-995.
- Abraham NS, Barkun JS, Barkun AN (2002) Palliation of malignant biliary obstruction: a prospective trial examining impact on quality of life. GastrointestEndosc 56:835-841.
- Prat F, Chapat O, Ducot B, Ponchon T, Pelletier G, et al. (1998) A randomized trial of endoscopic drainage methods for inoperable malignant strictures of the common bile duct. GastrointestEndosc 47:1-7.
- Lammer J, Hausegger KA, Flückiger F, Winkelbauer FW, Wildling R, et al. (1996) Common bile duct obstruction due to malignancy: treatment with plastic versus metal stents. Radiology 201:167-172.
- Ito K, Igarashi Y, Mimura T, Kishimoto Y, Kikuchi Y, et al. (2012) Efficacy of the new double-layer stent for unresectable distal malignant biliary obstruction: a single-center retrospective study. DiagnTherEndosc2012:680963.
- Isayama H, Yasuda I, Ryozawa S, Maguchi H, Igarashi Y, et al. (2011) Results of a Japanese multicenter, randomized trial of endoscopic stenting for non-resectable pancreatic head cancer (JM-test): Covered Wallstent versus DoubleLayer stent. Dig Endosc 23:310-315.
- Katsinelos P, Paroutoglou G, Chatzimavroudis G, Terzoudis S, Zavos C, et al. (2010) Prospective randomized study comparing double layer and Tannenbaum stents in distal malignant biliary stenosis. ActaGastroenterolBelg 73:445-450.
- Tringali A, Mutignani M, Perri V, Zuccalà G, Cipolletta L, et al. A prospective, randomized multicenter trial comparing DoubleLayer and polyethylene stents for malignant distal common bile duct strictures. Endoscopy 35:992-997.
- Brennan P, Silman A (1992) Statistical methods for assessing observer variability in clinical measures. BMJ 304: 1491-1494.
- Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ et al. (1996) Assessing the quality of reports of randomized clinical trials: Is blinding necessary? Controlled Clin Trials 17:1-12.
- Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, et al. (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis of observational studies in Epidemiology (MOOSE) group. JAMA 283:2008-2012.
- Stuart A, Ord JK (1994) Kendall's Advanced Theory of Statistics (6th edn.), London: Edward Arnold.
- DerSimonian R, Laird N (1986) Meta-analysis in Clinical Trials. Controlled Clinical Trials 7:177-188.
- Deeks JJ (2001) Systematic reviews of evaluations of diagnostic and screening tests. In Egger M, Smith GD, Altman DG (edn.), Systematic Reviews in Health Care. Meta-analysis in context. London: BMJ Books.
- Harbord RM, Egger M, Sterne JA (2005) A modified test for small-study effects in meta-analyses of controlled trials with binary endpoints. Statistics in Medicine 25:3443-3457.
- Begg CB, Mazumdar M (1994) Operating characteristics of a rank correlation test for publication bias. Biometrics 50:1088-1101.
- Sterne JA, Egger M, Smith GD (2001) Investigating and dealing with publication and other biases in meta-analysis. British Medical Journal 323:101-105.
- Sterne JAC, Egger M (2001) Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. Journal of Clinical Epidemiology 54:1046-1055.
- Katsinelos P, Paikos D, Kountouras J, Chatzimavroudis G, Paroutoglou G, et al. (2006)Tannenbaum and metal stents in the palliative treatment of malignant distal bile duct obstruction: a comparative study of patency and cost effectiveness. SurgEndosc 20:1587-1593.
- Liberato MJ, Canena JM (2012) Endoscopic stenting for hilarcholangiocarcinoma: efficacy of unilateral and bilateral placement of plastic and metal stents in a retrospective review of 480 patients. BMC Gastroenterol12:103.
- Donelli G, Guaglianone E, Di Rosa R, Fiocca F, Basoli A, et al. (2007) Plastic biliary stent occlusion: factors involved and possible preventive approaches. Clin Med Res 5:53-60.
- Jaganmohan S, Lee JH (2012) Self-expandable metal stents in malignant biliary obstruction. Expert Rev GastroenterolHepatol 6:105-114.
- van Berkel AM, van Marle J, Groen AK, Bruno MJ, et al. (2005) Mechanisms of biliary stent clogging: confocal laser scanning and scanning electron microscopy. Endoscopy 37:729-734.
Relevant Topics
- Constipation
- Digestive Enzymes
- Endoscopy
- Epigastric Pain
- Gall Bladder
- Gastric Cancer
- Gastrointestinal Bleeding
- Gastrointestinal Hormones
- Gastrointestinal Infections
- Gastrointestinal Inflammation
- Gastrointestinal Pathology
- Gastrointestinal Pharmacology
- Gastrointestinal Radiology
- Gastrointestinal Surgery
- Gastrointestinal Tuberculosis
- GIST Sarcoma
- Intestinal Blockage
- Pancreas
- Salivary Glands
- Stomach Bloating
- Stomach Cramps
- Stomach Disorders
- Stomach Ulcer
Recommended Journals
Article Tools
Article Usage
- Total views: 12574
- [From(publication date):
August-2016 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 11549
- PDF downloads : 1025