Assessment of Bariatric Surgery Patients in Lebanon: A Cross-Sectional Observational Study
Received: 12-Feb-2018 / Accepted Date: 16-Feb-2018 / Published Date: 23-Feb-2018 DOI: 10.4172/2165-7904.1000367
Abstract
Introduction: Obesity is considered a global epidemic disease with detrimental consequences. Bariatric surgery is a viable option for weight loss for patients with morbid obesity. This study sought to assess weight variation and supplements and medication use among bariatric surgery patients in Lebanon.
Methods: A total of 300 bariatric patients' ≥ 18 years of age were randomly enrolled to fill a questionnaire in English or Arabic, from all over Lebanese districts. Statistical analysis was performed by SPSS software (Version 23.0)
Results: Most patients were in the age category of less than 30 years of age (43.3%). Hypertension was the most reported comorbidity (15%), followed by Diabetes Mellitus (11.3%) and anaemia (11%). Three types of surgeries were reported with sleeve gastrectomy being the most performed (57.7%), followed by roux-en-y gastric bypass (27%) and gastric banding (15.3%). Weight loss was more common among sleeve gastrectomy patients for all ranges of weight variation except for >50 kg weight loss category where roux-en-Y bypass was associated with more weight loss (p<0.0001). Those with higher socio-economical levels (expβ=7.319, 95% CI 1.477-36.265, P=0.015), higher educational levels (expβ=5.967, 95% CI 1.386-25.683, P=0.016), smokers (expβ=5.772, 95% CI 1.471-22.650, P=0.012) and sleeve gastrectomy patients (expβ=8.229, 95% CI 2.101-32.229, P=0.002) were significantly more likely to have more weight loss. Among the mineral and vitamin supplements iron (42.3%) was the most commonly used, whereas PPIs ranked first (42.3%) among the used medications.
Conclusion: Sleeve gastrectomy was the most common bariatric surgery done in Lebanon and associated with the most postoperative weight loss. Vitamin and mineral supplements and PPIs were consumed by almost half of the patients. Despite these issues, larger scale follow-up studies are needed to assess these patients in order to establish further areas of improvements.
Keywords: Bariatric surgery; Gastric band; Sleeve gastrectomy; Bypass surgery; Weight variation; PPIs; Supplements
Introduction
Obesity is considered a global epidemic, according to the World Health Organization, with detrimental consequences [1]. Along the psychosocial disorders, patients with obesity are likely to have associated comorbidities such as hypertension, cardiovascular disorders, hyperlipidemia, diabetes, sleep apnea, degenerative arthritis and different cancer types [2].
Different clinical treatment modalities are considered ineffective for the management of patients with morbid obesity [3]. Hence, current guidelines consider adults failing behavioural and pharmacologic treatment with a body mass index (BMI) >40 kg/ m2 or >35 kg/ m2 with related comorbid conditions as candidates for bariatric surgery [4]. As a consequence, the number of bariatric surgeries performed increased dramatically in the last two decades by almost 70% [5].
Among the different types of bariatric surgeries, gastric banding, sleeve gastrectomy and Roux-en-Y gastric bypass are the most commonly performed [6-8]. Many positive outcomes have been linked to such surgeries. In addition to being a viable option for weight loss and weight maintenance in patients with morbid obesity [3], bariatric surgeries significantly improved comorbidities and even their regression [9]. Such improvements are reflected in the diminished or discontinued drug use during the post-operative period and consequently reduced expenditure on drug use and other healthcare services [10,11]. Furthermore, bariatric surgeries are associated with reduced overall mortality, mortality due to cardiovascular diseases and the occurrence of cardiovascular events [12,13].
On the other hand, bariatric procedures pose a higher risk of vitamins and minerals deficiencies that necessitates proper monitoring and intake of these substances after surgery [14]. The absorption of orally administered drugs, minerals and vitamins is affected [15]. Different parameters such as drug solubility, surface area of absorption and blood flow are altered in bariatric surgeries, and in consequence, the drug dissolution and absorption processes are compromised [15]. Patients suffering from chronic vomiting should consider protonpump inhibitors (PPIs) use [14].
In the absence of assessment data of bariatric surgery patients in Lebanon and since these surgeries are considered one of the fastest growing operative procedures worldwide [5], we conducted this study. The main objective of this study is to assess weight variation and supplements and medication use post bariatric surgeries and the factors that may affect such variation among the Lebanese patients.
Materials and Methods
Study design and setting
This is a descriptive, prospective, cross-sectional observational study conducted all over Lebanon between February and May 2017. The sample was drawn randomly from all the districts of Lebanon that includes the capital Beirut and four other districts (Mount Lebanon, North, Beqaa, and the South). Out of 341 patients approached, 300 participants were eventually enrolled in the study with a refusal rate of 12%. The study was approved by the ethical committee at the Lebanese International University. Informed consents were obtained from all participants prior to enrolment. However, data were stripped of any personal identified information.
Data collection
A data collection sheet to obtain the needed information was established. This sheet retrieved information regarding patient demographics (gender, age, residence, educational level, socioeconomic status and physical activity), type of bariatric surgery performed, comorbidities, weight variation and medications and supplements used post-surgery.
Inclusion and exclusion criteria
Adult Lebanese patients 18 years of age and older who had undergone previously a bariatric surgery were considered eligible for study enrolment. Excluded patients were those younger than 18 years of age and non-Lebanese residents.
Study outcomes
The primary outcome of this study assesses the weight variation and supplements and medication use among the three most common types of bariatric surgeries including gastric banding, sleeve gastrectomy and roux-en-y gastric bypass. The secondary outcome determines the factors that may be associated with such weight variation and medication use.
Statistical analysis
Statistical analysis was performed using the statistical package for the social science software (SPSS version 22.0). Descriptive statistics were used to describe patient characteristics with frequencies and percentages for categorical variables. Univariate associations were assessed for statistically significant differences using Chi-square or Fisher’s exact tests for categorical variables, as appropriate. Logistic regression was used to test for significant associations between different variables and weight variation and medication use. All reported p-values were two-sided with the alpha set at a significance of 0.05.
Results
Patient’s demographic characteristics
A total of 300 participants were enrolled and interviewed in this study. (Table 1) summarizes the patient's characteristics. Most patients were in the age category of less than 30 years of age (43.3%). As age increases the percentage of involved bariatric patients' decreases with the lowest proportion for those above 60 years of age (0.7%).
| Variable | N Percentage (%) |
|---|---|
| Age (in years) | |
| 18-29 | 130 (43.4%) |
| 30-39 | 88 (29.3%) |
| 40-49 | 61 (20.3%) |
| 50-59 | 19 (6.3%) |
| > 60 | 2 (0.7%) |
| Gender | |
| Male | 103 (34.3%) |
| Female | 197 (65.7%) |
| District | |
| Beirut | 149 (49.7%) |
| South | 56 (18.7%) |
| North | 14 (4.7%) |
| Beqaa | 26 (8.7%) |
| Mount Lebanon | 55 (18.3%) |
| Educational level | |
| Primary and complementary | 50 (16.7%) |
| Secondary | 92 (30.7%) |
| University | 158 (52.7%) |
| Socioeconomic level | |
| Low | 14 (4.7%) |
| Intermediate | 173 (57.7%) |
| High | 113 (37.7%) |
| Moderate-vigorous physical activity | |
| No | 207 (69%) |
| 2-4 times/weekly | 63 (21%) |
| Daily | 30 (10%) |
| Smoker (yes) | 168 (56%) |
| Alcohol (yes) | 42 (14%) |
Table 1: Sociodemographic and socioeconomic characteristics of the participants.
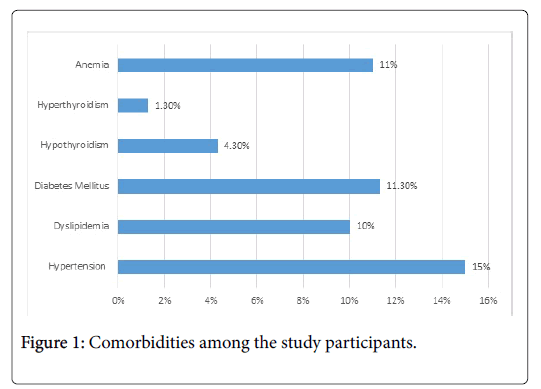
The majority of the participants were females (65.7%) and almost half of the patients were from the capital Beirut (49.7%). More than half of the subjects (52.7%) hold university degrees and live within intermediate socio-economical levels (57.7%). More than two-third of the participants (69%) reported the absence of moderate to vigorous physical activity with 56% being smokers and 14% alcohol consumers. Figure 1 demonstrates the most common comorbidities among the participants with hypertension being the most prevalent (15%), followed by Diabetes Mellitus (11.3%) and anaemia (11%).
Type of bariatric surgery
Table 2 reveals the type of bariatric surgery the patients had performed.
| Variable | N Percentage (%) |
|---|---|
| Surgery | |
| Gastric banding | 46 (15.3%) |
| Sleeve gastrectomy | 173 (57.7%) |
| Roux en-y bypass | 81 (27%) |
Table 2: Surgery type among participants.
Three types of surgeries were reported with sleeve gastrectomy being the most performed (57.7%), followed by roux-en-y gastric bypass (27%) and gastric banding (15.3%).
Weight variation
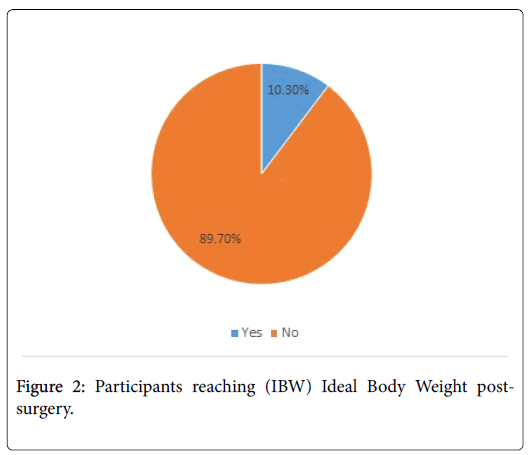
Among the studied participants, only 31 (10.3%) reached their ideal body weight (IBW) post-surgery (Figure 2).
However, weight loss was prominent among all participants with the most (27%) having weight variation between 31-40 kg post-surgery (Table 3). Weight variation was not consistent among the different bariatric surgeries. Weight loss was more common among sleeve gastrectomy patients for all ranges of weight variation except for >50 kg weight loss category where roux-en-Y bypass was associated with more weight loss (p<0.0001).
| Weight variation | Gastric binding N Percentage (%) | Sleeve gastrectomy N Percentage (%) | Roux-en by pass N Percentage (%) | Total N Percentage (%) | P-value |
|---|---|---|---|---|---|
| 0-10 kg | 3 (37.5) | 4 (50) | 1 (12.5) | 8 (2.7) | 0.0001 |
| 11-20 kg | 9 (33.3) | 13 (48.1) | 5 (18.5) | 27 (9) | |
| 21-30 kg | 11 (16.7) | 45 (68.2) | 10 (15.2) | 66 (22) | |
| 31-40 kg | 13 (16) | 53 (65.4) | 15 (18.5) | 81 (27) | |
| 41-50 kg | 3 (5.7) | 32 (60.4) | 18 (34) | 53 (17.7) | |
| >50 kg | 7 (10.8) | 26 (40) | 32 (49.2) | 65 (21.7) |
Table 3: Weight variation among the different bariatric surgeries.
Different factors were significantly associated with weight variation. Those with higher socio-economical levels (expβ=7.319, 95% CI 1.477-36.265, P=0.015), higher educational levels (expβ=5.967, 95% CI 1.386-25.683, P=0.016), smokers (expβ=5.772, 95% CI 1.471-22.650, P=0.012) and performed sleeve gastrectomy (expβ=8.229, 95% CI 2.101-32.229, P=0.002) were significantly more likely to have more weight loss.
Supplements and medication use
Different medications and supplements were used by the participants post bariatric surgery. Among the mineral and vitamin supplements iron (42.3%) was the most commonly used, and among medications PPIs (42.3%) were the mostly used ones. Iron and calcium were used more among sleeve gastrectomy patients and roux-en-Y bypass patients (p=0.0001). While Vitamin B12 was more used among roux-en-Y bypass patients (p=0.0001), PPIs were more consumed by sleeve gastrectomy patients (p=0.009) (Table 4).
| Vitamin or supplement | Gastric binding N Percentage (%) | Sleeve gastrectomy N Percentage (%) | Roux-en by pass N Percentage (%) | Total N Percentage (%) | p-value |
|---|---|---|---|---|---|
| Iron | 21 (16.5) | 53 (41.7) | 53 (41.7) | 127 (42.3) | 0.0001 |
| Calcium | 11 (13.6) | 34 (42%) | 36 (44.4) | 81 (27) | 0.0001 |
| B12 | 10 (12.3) | 28 (34.6) | 43 (53.1) | 81 (27) | 0.0001 |
| B9 | 8 (20.5) | 20 (51.3) | 11 (28.2) | 39 (13) | 0.570 |
| B Complex | 5 (9.4) | 31 (58.5) | 17 (32.1) | 53 (17.7) | 0.353 |
| PPI | 11 (8.7) | 84 (66.1) | 32 (25.2) | 127 (42.3) | 0.009 |
| H2>Blockers | 3 (42.9) | 2 (28.6) | 2 (28.6) | 7 (2.3) | 0.100 |
| NSAIDs | 0 (0) | 11 (50) | 11 (50) | 22 (7.3) | 0.014 |
| Oral contraceptives | 0(0) | 3 (60%) | 2 (40) | 5 (1.7) | 0.576 |
Table 4: Supplements and medication use post bariatric surgery.
Discussion
Obesity stands out as one of the biggest public health issues with bariatric surgery being a viable and important option for management. It is estimated that more than 340,000 bariatric operations were done in 2011 [16]. This study aimed to assess Lebanese bariatric surgery patients in terms of weight variation, supplements and medication use.
Patients characteristics
More than two-third of the participants (69%) reported the absence of moderate to vigorous physical activity per day. Actually, Evans et al. compared weight loss in post-bariatric gastric bypass surgery patients divided into two groups- those that reported at least 150 minutes of moderate intensity per week and those that reported less than 150 minutes [17]. Weight loss was significantly greater in the first group and the difference between groups was about 6% greater excess weight loss at 6 and 12 months post-surgery [17]. Such results necessitate improving awareness among the participants regarding the importance of physical activity in enhancing weight loss.
About 14% of the participants reported alcohol consumption. An important notice to the psychological changes patients undergo after the surgery revealed an increase in their sensitivity to alcohol, where those patients experience higher concentrations of ethanol than a normal individual [18]. This is another domain at which health care providers should intervene to counsel properly post-bariatric patients to avoid any complications.
The most common comorbidities among our participants were hypertension (15%), followed by Diabetes Mellitus (11.3%) and anaemia (11%). The results are comparable to Backes et al study in 2016 which revealed that the most common comorbidities during the postoperative phase were hypertension (29.7%), followed by diabetes (6.3%) and dyslipidemia (6.3%) [19]. Unlikely, the percentage of those with hypertension were lower in our study as compared to Backes et al study but diabetes percentage was higher in the Lebanese bariatric population [19].
Type of surgery
In consistence with our results, the American Society for Metabolic and Bariatric Surgery (ASMBS) reported that the most common bariatric surgery procedures are gastric bypass, sleeve gastrectomy, and adjustable gastric band [20]. Sleeve gastrectomy was the most performed (57.7%) bariatric surgery in our study, followed by roux-eny gastric bypass (27%) and gastric banding (15.3%). Unlikely, in Backes et al study, the surgical technique most often used was gastric bypass (91.4%) [19].
Weight variation and associated factors
In this study weight loss was more common among sleeve gastrectomy patients except for >50 kg weight loss category where roux-en-Y bypass was associated with more weight loss (p<0.0001). Our results are not consistent with Maciejewski et al. study [21] where patients undergoing roux en-Y gastric bypass lost 16.9% (95% CI, 6.2%-27.6%) more of their baseline weight than patients undergoing gastric banding and 9.7% (95% CI, 0.8%-18.6%) more than patients undergoing sleeve gastrectomy. Further larger scale studies are needed in Lebanon to assess such differences.
Different factors were significantly associated with more weight variation in this study including higher socio-economical levels, higher educational levels, smokers and sleeve gastrectomy. In Binda et al. study, Lower baseline body weight parameters, younger age, preoperative weight loss, starting physical activities and constant care of a dietician were conducive to achieving better results of sleeve gastrectomy surgery [22].
Supplements and medication use
Iron was the most commonly used mineral supplement, and PPIs were the mostly used medication. Backes et al. study also revealed a high use of vitamins and minerals by more than half of the participants (56.5%) [19]. As these surgeries pose a high risk of vitamins and minerals deficiencies, such supplements are of extreme importance especially in mal-absorptive procedures. PPI use is also vital where a significant incremental benefit of prophylactic PPI in reducing marginal ulcer after gastric bypass surgery was revealed by a metaanalysis done in 2014 [23]. Iron and calcium were used more among sleeve gastrectomy patients and roux-en-Y bypass patients. While Vitamin B12 was more used among roux-en-Y bypass patients, PPIs were more consumed by sleeve gastrectomy patients.
This study also demonstrated a very low use of oral contraceptives (1.7%). Mehri et al. study showed an increase in fertility, and pregnancy rates in bariatric surgery patients. However, the use of oral contraceptives in these patients is not reliable due to the lower absorption and bioavailability of these drugs after the surgical procedure [24]. Hence, alternative contraceptive methods should be considered which may explain such low use.
Limitations and strengths
This study had different limitations. One of these limitations is a need for more comprehensive studies with longer follow-up periods, with pharmacokinetic assessments before and after bariatric surgery. Moreover, these studies need to address other factors that may have influenced the weight loss process. Another limitation is the crosssectional study design that doesn’t make it possible to determine with certainty the direction of the identified associations. In addition, this study was based on self-reported data, which can be subject to inaccuracy due to recall bias, social desirability bias, and errors in selfobservation.
Despite these limitations, and to our knowledge, this was the first descriptive cross-sectional observational study covering all Lebanese areas that assessed weight variation and supplements and medications use among 300 bariatric surgery patients.
Conclusion
Based on the obtained data from this descriptive study, sleeve gastrectomy was the most common bariatric surgery done in Lebanon and associated with the most postoperative weight loss. Vitamin and mineral supplements and PPIs were consumed by almost half of the patients. Despite these issues, several areas of interventions were revealed for counselling and improvement of post-surgical weight loss and reduction of complications. Hence, larger scale follow-up studies are needed to assess these patients to establish further areas of improvements.
Conflicts of Interest
The authors have nothing to disclose.
Funding Sources
The authors received no funds for this study.
Contributions
Marwan Akel and Iqbal Fahs contributed equally to study design, data collection and analysis, drafting and revising the manuscript. Mohamad Rahal, Michelle Cherfan, Mariam Dabbous and Jihan Safwan revised the manuscript. All authors read and approved the final manuscript.
References
- Marcelino LF, Patricio ZM (2011) The complexity of obesity and life after bariatric surgery: A public health issue. Cien Saude Colet 16: 4767-4776.
- Guh DP, Zhang W, Bansback N, Amarsi Z, Birmingham CL, et al. (2009) The incidence of co-morbidities related to obesity and overweight: A systematic review and meta-analysis. BMC Public Health 9: 88.
- Wadden TA, Sternberg JA, Letizia KA, Stunkard AJ, Foster GD (1989) Treatment of obesity by very low calorie diet, behavior therapy, and their combination: A five-year perspective. Int J Obes 13: 39-46.
- Jensen MD, Ryan DH, Apovian CM, Loria CM, Ard JD, et al. (2014) AHA/ACC/TOS guideline for the management of overweight and obesity in adults: A report of the American College of Cardiology/American Heart Association task force on practice guidelines and the obesity society. J Am Coll Cardiol 63: 2985-3023.
- Padwal RS, Gabr RQ, Sharma AM, Langkaas LA, Birch DW, et al. (2011) Effect of gastric bypass surÂgery on the absorption and bioavailability of metfotmin. Diabetes Care 34: 1295-1300.
- Schauer PR, Burguera B, Ikramuddin S, Cottam D, Gourash W, et al. (2003) Effect of laparoscopic Roux-en Y gastric bypass on type 2 diabetes mellitus. Ann Surg 238: 467-484.
- Buchwald H (2008) International symposium on gastric banding. Supplement to surgery for obesity and related diseases. Cambridge Els 4: 71.
- Himpens J, Dapri G, Cadiere GB (2006) A prospective randomized study between laparoscopic gastric banding and laparoscopic isolated sleeve gastrectomy: Results after 1 and 3 years. Obes Surg 16: 1450-1456.
- Piche ME, Auclair A, Harvey J, Marceau S, Poirier P (2015) How to choose and use bariatric surgery in 2015. Can J Cardiol 31: 153-66.
- Buchwald H, Avidor Y, Braunwald E, Jensen MD, Pories W, et al. (2004) Bariatric surgery: A systematic review and meta-analysis. JAMA 292: 1724-1737.
- Gould JC, Garren MJ, Starling JR (2004) Laparoscopic gastric bypass results in decreased prescription medication costs within 6 months. J Gastrointest Surg 8: 983-987.
- Kwok CS, Pradhan A, Khan MA, Anderson SG, Keavney BD, et al. (2014) Bariatric surgery and its impact on cardiovascular disease and mortality: A systematic review and meta-analysis. Int J Cardiol 173: 20-28.
- Sjostrom L, Peltonen M, Jacobson P, Karason K, Wedel H, et al. (2012) Bariatric surgery and long term cardiovascular events. JAMA 307: 56-65.
- Malone M, Alger-Mayer S, Lindstrom J, Bailie GR (2013) Management of iron deficiency and anemia after Roux-en-Y gastric bypass surgery: An observational study. Surg Obes Relat Dis 9: 969-974.
- Miller AD, Smith KM (2006) Medication and nutrient administration considerations after bariatric surgery. Am J Health Syst Pharm 63: 1852–1857.
- Nguyen NT, Masoomi H, Magno CP, Nguyen XM, Laugenour K, et al. (2011) Trends in use of bariatric surgery, 2003-2008. J Am Coll Surg 213: 261-266.
- Evans RK, Bond DS, Wolfe LG, Meador JG, Herrick JE, et al. (2007) Participation in 150 min/wk of moderate or higher intensity physical activity yields greater weight loss after gastric bypass surgery. Surg Obes Relat Dis 3: 526-530.
- Heinberg LJ, Ashton K, Coughlin J (2012) Alcohol and bariatric surgery: Review and suggested recommendations for assessment and management. Surg Obes Relat Dis 8: 3570-363.
- Backes C, Lopes E, Tetelbom A, Heineck I (2016) Medication and nutritional supplement use before and after bariatric surgery. Sao Paulo Med J 134: 491-500.
- American Society for Metabolic and Bariatric Surgery (2018) Bariatric surgery procedures.
- Maciejewski M, Arterburn D, Van Scoyoc l, Smith VA, Yancy WS Jr, et al. (2016) Bariatric surgery and long-term durability of weight loss. JAMA Surg 151: 1046.
- Binda A, Jaworski P, Kudlicka E, Ciesielski A, Cabaj H, et al. (2016) The impact of selected factors on parameters of weight loss after sleeve gastrectomy. Wideochir Inne Tech Maloinwazyjne 4: 288-294.
- Ying VW, Kim SH, Khan KJ, Farrokhyar F, D'Souza J, et al. (2014) Prophylactic PPI help reduce marginal ulcers after gastric bypass surgery: A systematic review and meta-analysis of cohort studies. Surg Endosc 29: 1018-1023.
- Yska JP, van der Linde S, Tapper VV, Apers JA, Emous M, et al. (2013) Influence of bariatric surgery on the use and pharmacokinetics of some major drug classes. Obes Surg 23: 819-25.
Citation: Akel M, Fahs I, Rahal M, Cherfan M, Dabbous M, et al. (2018) Assessment of Bariatric Surgery Patients in Lebanon: A Cross-Sectional Observational Study. J Obes Weight Loss Ther 8:367. DOI: 10.4172/2165-7904.1000367
Copyright: © 2018 Akel M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5521
- [From(publication date): 0-2018 - Jul 18, 2025]
- Breakdown by view type
- HTML page views: 4655
- PDF downloads: 866