Research Article Open Access
Awareness to Implementation on Select Quality and Patient Safety Indicators Among Nursing Staff
Ali Yawar Alam1* and Mohammad Khalid Alabdulaali21Strategy Management Department, Health Affairs Al Ahsa, Ministry of Health, Kingdom of Saudi Arabia
2Health Affairs Al Ahsa, Ministry of Health, Kingdom of Saudi Arabia
- *Corresponding Author:
- Ali Yawar Alam
Director Project Management Office (PMO)
Strategy Management Department, Directorate of Health Affairs Al Ahsa
Ministry of Health, Kingdom of Saudi Arabia
Tel: 00966542318776
E-mail: aliyawaralam@gmail.com
Received date: January 22, 2016; Accepted date: February 11, 2016; Published date: February 18, 2016
Citation: Alam AY, Alabdulaali AK (2016) Awareness to Implementation on Select Quality and Patient Safety Indicators Among Nursing Staff. J Comm Pub Health Nursing 1:111. doi:10.4172/2471-9846.1000111
Copyright: © 2016 Alam AY, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Community & Public Health Nursing
Abstract
Objective: This study aimed to determine the awareness level of the nursing staff for policies and procedures related to quality of care, patient safety and general safety and assess the congruence of knowledge with implementation.
Methods: Key informant interviews were conducted on 85 Nurses (Front line nurses) in a tertiary health care facility in April 2012 and implementation statistics on select quality and patient safety indicators were obtained from clinical audit programme (CAP) for the same month.
Results: The awareness level of the nurses on quality, patient safety and general safety was found to be good. The compliance on quality and patient safety policies was lower than the knowledge level. A conceptual framework has been devised addressing the knowledge-implementation gap.
Conclusion: The awareness level of the nurses on quality, patient safety and general safety was found to be good. The compliance on quality and patient safety indicators was lower than the knowledge level. The challenge of transforming knowledge to patient care practices needs to take account of work environment determinants (such as; strong general and departmental orientation of nurses, patient/nurse ratio, clinicians involving nurses in clinical decision making process and tracking outcomes of care, mutual trust among team members, teams of physicians and nurses learning together by doing rather than traditional teaching, effective supervision of nurses, and presence of enabling champions in the unit).
Introduction
Doctors and nurses are the front line staff in the hospital that deliver patient care. It is the nurses however, who provide the majority of direct patient care. As such it is imperative to assess the nurses competency in general and on quality and patient safety in particular, for several reasons. A major health care provider to the people of the Eastern province, Kingdom of Saudi Arabia, our study hospital gives top priority to quality and patient safety. The mission of this hospital; “Providing safe, effective, efficient and high quality preventive and curative health care services delivered by a highly professional and motivated team for the community, in accordance with local and International quality standards. Our prime focus is the patient.” The need for quality, patient safety and general safety has been clearly defined by the leaders, in the study hospital. Uplifting quality, patient safety and general safety standards in the hospital boosts staff confidence in the work environment and subsequently the patient’s confidence on the hospital. However, one of the greatest challenges in quality is to meet and exceed the expectations of the patients. We are committed to excellence and are continuously striving to raise the bar and meet and exceed the patients and their families expectations. As a recognition to these efforts the Central Board For Accreditation of Health Care Institutions (CBAHI), Kingdom of Saudi Arabia, granted accreditation to this Hospital three years ago. For the last two years, the study hospital has been intensively preparing for Joint Commission International Accreditation (JCIA). A lot of time and effort with ongoing professional training of hospital staff in general and nurses more specifically has occurred in the study hospital during the CBAHI accreditation process and more recently for JCIA. These training sessions involved nurses in morning meetings, Lectures, seminars, symposia, workshops and ward round teaching/learning. The trainings sessions included detailing policies and procedures related to International patient safety goals, quality of care, general safety, performance improvement, incident reporting and learning from near miss and sentinel events. A nursing challenge is to keep a balance between their personal and clinical responsibilities, thus learning the new policies and procedures while applying them to practice, accepting and absorbing accreditation pressures and adopting system thinking [1].
This study aims to determine the awareness of the nursing staff in terms of quality of care, patient safety and general safety in the hospital. The other aim of this study is to assess the congruence of the awareness level of the nurses with select quality and patient safety indicators in the hospital, at the same point in time.
Methods
Key informant interviews were conducted on 85 Nurses (Front line nurses) in a tertiary health care facility in April 2012. The study hospital is a 502 bed tertiary health care facility (Adult care General hospital with General Medicine, General Surgery and Orthopedics inpatients) in the Eastern province of the Kingdom of Saudi Arabia. Approval to conduct the interviews were obtained from the Institutional Review board (Approval #: 5/REC/3/2012) and the hospital and nursing administrations. Informed verbal consent was obtained from the participating nurses. Interviewer administered questionnaire was used. The hospital quality and patient safety indicators were obtained from clinical audit programme (CAP) of the hospital for the same month. SPSS v 20 was used for data entry and analysis.
This interviewer administered questionnaire did not record the names of the nurses to ensure confidentiality. The response rate of the participants was 100%. Stratified random sampling was done. The strata were the various units of general medicine, general surgery and Orthopedics. The sample size was proportionally divided among the 10 units of the hospital in-patients based on the nursing population size of the unit. Identification number of nurses with experience of working six months or more in this hospital was obtained from the concerned head nurse. For each of the 10 sampling frame, computer generated random sampling was done. Stratification ensured representativeness of all units of the hospital and random sampling ensured generalizability of the results.
The sample size was calculated using WHO software. Expected awareness level of the nurses in terms of quality and safety was 70%. The sample size was estimated for a precision of ± 10%. For 95% confidence interval sample size came to 81. The sample size was inflated to 85 for contingencies such as incomplete survey form. Since this was a key informant interview a sample size of 85 was deemed large enough.
Data collection tool was ‘Quality and patient safety awareness tool,’ specifically developed by the quality department of this hospital for the survey. This tool could be shared with all the hospitals, who are in the process of preparing for CBAHI, JCIA or any other quality of care accreditation. It was an interviewer administered questionnaire, as many of the responses included giving examples, short explanations and so on. After listening to the participants response, the interviewer had to mark either ‘Yes,’ ‘No,’ or ‘Not applicable.’ The survey tool was pilot tested to assess the validity, language issues, length and understanding of the participants about the questions asked. Any discrepancy found was removed (Question on IPSG was removed which had the item as to how many IPSGs the interviewee knew. That was creating problems in analysis. We kept as to what IPSG stands for and if the staff could explain some of them. FMEA being new to the hospital, so it was removed) and the questionnaire was ready for the survey. The questionnaire was administered by the Principal investigator, quality coordinators and quality representatives of the hospital, specifically trained to handle this questionnaire.
The hospital quality and patient safety indicators were obtained by the principal investigator from clinical audit programme (CAP) of the hospital for the same month (April 2012). CAP team routinely collects data on monthly/quarterly basis from the hospital, enters it to it’s database and report the results graphically.
All data was entered and analyzed using SPSS version 20.0.
Results
Fifty five (65%) of the participants were female. The experience of the nursing staff ranged from one and half years to 17 years. 82 (96%) of the nursing staff were exposed to departmental orientation while 43 (50%) of them had attended a general orientation session in the hospital at the start of their job. 76 (89%) of the nurses were able to show departmental policies in one folder while 37 (43%) of the nurses were able to show hospital-wide policies in one folder in the floor where they were performing their duties. 76 (89%) of the nurses reported that the Chief of the nursing department told them to read the hospital policies, while 65 (76%) of the nurses said that they actually read those policies.
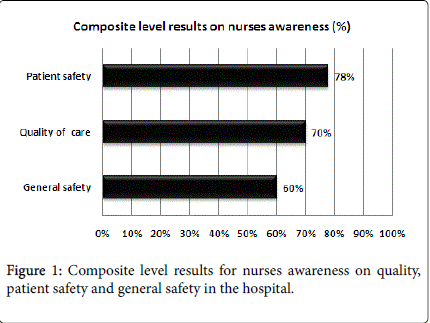
Composite level indicators on Quality of care, patient safety and general safety are presented in Figure 1. Over 60% of the staff was aware of the composite level of quality, patient safety and general safety.
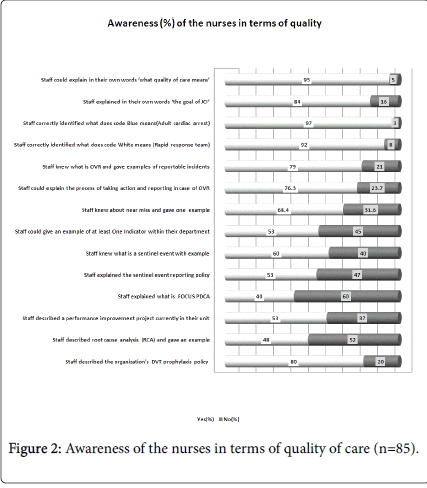
Figure 2 displays the awareness level of the nurses in terms of quality of care and related hospital policies/procedures. The highest awareness level (97%) was related to the nurses knowledge about code blue (cardiac arrest). Nurses knew very well as to ‘what does quality of care meant,’ goals of JCI, incident reporting system in the hospital and near miss with example. Whereas, only 40% of the staff could adequately explain the acronym FOCUS PDCA. Other lower areas of awareness included abilities to give an example indicator from their department (53%), staff were able to explain the sentinel event reporting policy (53%), staff was able to describe a performance improvement project in their unit (53%) and staff were able to describe root cause analysis and give one example (48%).
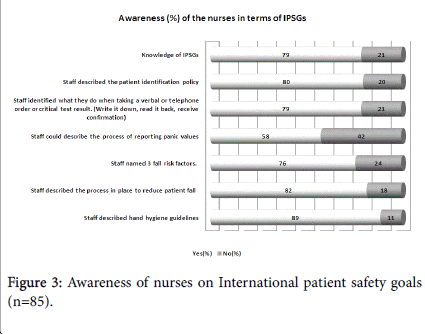
Figure 3 displays the awareness level of the nurses on International patient safety goals (IPSGs) and related hospital policies/procedures. Nurses depicted a good knowledge of the patient identification policy in the hospital (80%). Knowledge about panic value reporting policy in the hospital was the weakest (58%). Other patient safety indicators showed acceptable knowledge level (>70%) of the nurses.
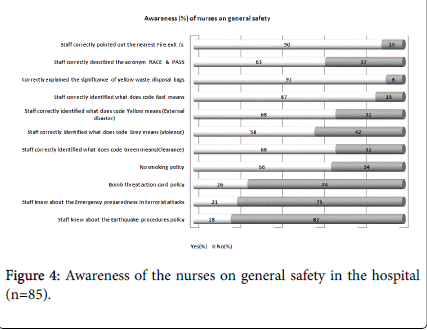
In terms of general safety in the hospital, awareness was highest (92%) for nurses correctly explained the significance of yellow waste disposal bags, while 90% correctly pointed out the nearest fire exit. Unacceptable low level of awareness was depicted by nurses in terms of earthquake procedure policy (18%), emergency preparedness in terrorist attack (21%) and bomb threat action card policy (26%).
Table 1 displays the relationship between awareness and compliance on select indicators in terms of quality and patient safety in the hospital. All the indicators reflect a lower compliance in comparison to awareness level of the nursing staff.
| Indicator | Level of Indicator | Awareness % | Compliance % | Compliance to Awareness difference |
|---|---|---|---|---|
| Compliance to patient identification in wards; for history, physical examination, before taking blood samples or giving medications | Process | 80 | 26 | -54% |
| Compliance to verbal and Telephone order policy (Write it down, read it back, receive confirmation) | Process | 79 | 57 | -22% |
| Compliance to panic value writing policy on patient files for Biochemistry lab results(Write it down, read it back, receive confirmation) | Process | 58 | 17 | -41% |
| Compliance to hand hygiene policy | Process | 89 | 20 | -69% |
| Compliance to assessment of patient fall policy | Process | 82 | 45 | -37% |
| %age of ICU patients who received DVT prophylaxis on admission | Process | 80 | 63 | -17% |
Table 1: Relationship between awareness and compliance on select indicators.
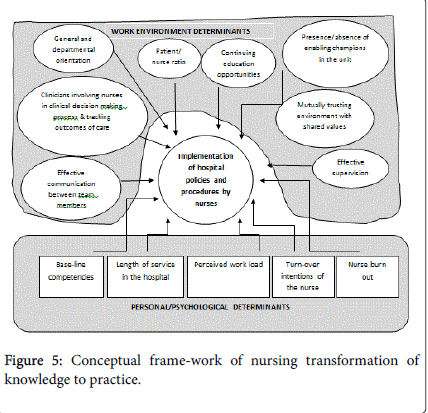
Nursing practices are affected by multiple factors; which can be broadly grouped as nurses personal determinants and work environment determinants, as depicted in Figure 5.
Discussion
The purpose of health care delivery is to provide holistic, patient centered, respectful, timely, safe, high quality, efficient and effective services to the patients addressing their individual health care needs in a safe environment. Integral to the success of this target is care coordination [2,3]. Along with the doctors, nurses are among the front line care providers. In contrast to doctors nurses spend the major bulk of their duty time with the patients, as such, their role in the care coordination across the continuum from illness to wellness is immense [3]. Nurses not only are diagnosing patient problems and risks that need attention and care interventions, but nurses are diagnosing needs for health enhancement and health promotion diagnoses as the patient progresses towards health and preparing for home.
Nursing practices related to hospital policies and procedures are affected by multiple factors which are broadly grouped under nurse personal determinants and work environment determinants, conceptual frame-work presented as Figure 5. The nurse personal determinants are described by base-line competencies, turn-over intentions and perceived work load are important factors worth consideration in hiring the nurses. Once the nurses have been hired, work environment determinants have a huge role to play in the day to day performance of the nurses and their compliance to hospital policies and procedures. Others have reported that in order to achieve favorable nursing outcomes, it is important for clinicians and leaders to consider how nurses are involved in decision-making about care processes and tracking outcomes of care and whether they are able to work with physicians, superiors, peers, and subordinates in a trusting environment based on shared values [4,5]. We believe this involvement in making decisions leads nurses to better understand and become aware of what is within the policies and procedures and helps in further development of shared values and building environment of trust with the physicians.
The awareness level of the nurses on quality, patient safety was found to be acceptable in this study. In contrast to awareness level, compliance on select hospital policies and procedures was lower. The transformation of the nurses awareness in to practice, regarding hospital policies and procedures and quality, patient safety and general safety, is indeed a nursing challenge. The real challenge is to comprehend the dynamics and interaction of factors that promote or inhibit the nurses to transform their knowledge into practices as per hospital policies and procedures.
A recent study suggested an innovative interprofessional education strategy in which teams of physicians and nurses were "learning by doing" [6]. The strength of this strategy is exemplified by the fact that fellows not only learned from each other's separate professional observations, but also observed the emergence of a shared interprofessional perspective through working together [5]. This approach could be utilized for implementation of those hospital policies and procedures which are difficult to implement. This would also improve team coordination and promote team work.
Work environment has a huge influence on effectiveness of the nursing practice. A study in China was conducted to investigate the influence of professional nursing practice environment and psychological empowerment on nurses' work engagement. The study involved random sample of 300 clinical nurses from two tertiary first class hospitals. The Utrecht Work Engagement Scale, the Practice Environment Scale of the Nursing Work Index and the Psychological Empowerment Scale were used to measure the study variables. The study found out that that both professional practice environment and psychological empowerment could positively influence work engagement directly, and professional practice environment could also indirectly influence work engagement through the mediation of psychological empowerment Psychological empowerment of the nurses in this way would result in increased nurse engagement with the patients and as a result better patient outcomes [7,8]. Work environment has several possible determinants as outlined in the conceptual frame-work in Figure 5. Each environmental factor is worthy of attention to achieve desired patient outcomes.
Higher registered nurse staffing has been associated with less hospital-related mortality and improved outcomes [9]. In this study the effect of increased registered nurse staffing on patients safety was strong and consistent in intensive care units and in surgical patients.
Hospitals with higher nurse staffing had 25 percent lower odds of being penalized for re-admissions compared to otherwise similar hospitals with lower staffing [10].
General and departmental orientation of the newly hired nursing staff is important to apprise orientees of the major hospital policies and procedures that are not immediately adopted early into practice. The orientation process needs to be constantly updated and refined after evaluation data [11]. Health care managers are in a crucial position to support the orientation process in practice and will value ‘orientation’ as a retention strategy [11].
Provision of safe and quality care is not equivalent to high tech care. Provision of safe care very often does not demand high tech care. For example directly asking the patient his/her complete name (usually three names) and father’s name (in case patient has only two names) each and every time; during taking history and physical examination, taking blood samples for lab testing, before undergoing radiological investigations, before giving medications to the patients, before invasive or non-invasive procedures, before transferring the patient to other unit or hospital and before sending the patient to the operation Room. The practice of identifying the patient just by bed number or room number is a potential cause of medical errors. The health care providers should always use two unique identifiers for the patient; patient full name and medical record number. This method of identifying he patients is ‘International Patient Safety Goal (IPSG 1); Identify patients correctly’ [12].
Nurses are well known and respected for championing practices that contribute to high standards of patient care, save lives, and help to influence other disciplines to do the same. Hand hygiene is one such practice [13].
One study involved ‘Crew resource management techniques,’ for improving patient safety and optimizing nursing teamwork [14]. One unit developed a novel application of the sterile cockpit rule to create protected time for certified nursing assistants (CNAs) while they collected vital signs and blood glucose data at the beginning of each shift. This process led to improvements in efficiency and communication among nurses, with the added benefit of increased staff morale. The study concluded that Crew resource management techniques can be used to improve efficiency, morale, and patient safety in the healthcare setting [13].
The overall purpose of all these measures is to improve the processes and systems, minimize human errors, improve patient safety, improve general safety, ensure quality of care, ensure continuity of care, minimize waste, improve patient outcomes and enhance patient satisfaction with the care provided to them.
Conclusion
The awareness level of the nurses on quality, patient safety and general safety was found to be good. The compliance on quality and patient safety indicators was lower than the knowledge level. A conceptual framework has been devised addressing the knowledge-implementation gap which would be of interest for health care leaders world-wide. The challenge of transforming knowledge to patient care practices needs to take account of work environment determinants(such as; strong general and departmental orientation of nurses, patient/nurse ratio, clinicians involving nurses in clinical decision making process and tracking outcomes of care, mutual trust among team members, teams of physicians and nurses learning together by doing rather than traditional teaching, effective supervision of nurses, and presence of enabling champions in the unit) in order to make the hospital compliant to it’s policies and procedures.
References
- Walrath JM, Muganlinskaya N, Shepherd M, Awad M, Reuland C, et al. (2006) Interdisciplinary medical, nursing, and administrator education in practice:the Johns Hopkins experience. Acad Med81:744-748.
- Rodgers D, Calmes B, Grotts J (2014) Creating national standards from the point of care. Nurs Adm Q 38:86-92.
- George VM, Shocksnider J (2014) Leaders: are you ready for change? The clinical nurse as care coordinator in the new health care system. Nurs Adm Q 38:78-85.
- Van Bogaert P, Kowalski C, Weeks SM, Van Heusden D, Clarke SP (2013) The relationship between nurse practice environment, nurse work characteristics, burnout and job outcome and quality of nursing care: a cross-sectional survey. Int J Nurs Stud 50:1667-77.
- Stimpfel AW, Rosen JE, McHugh MD (2014) Understanding the role of the professional practice environment on quality of care in magnet® and non-magnet hospitals. J Nurs Adm 44:10-6.
- Brennan CW, Olds DM, Dolansky M, Estrada CA, Patrician PA (2014) Learning by doing: observing an interprofessional process as an interprofessional team. J Interprof Care 28:249-51.
- Wang S, Liu Y (2013) Impact of professional nursing practice environment and psychological empowerment on nurses' work engagement: test of structural equation modelling. J NursManag 23: 287-296.
- Suhonen R, Stolt M, Gustafsson ML, Katajisto J, Charalambous A (2014) The associations among the ethical climate, the professional practice environment and individualized care in care settings for older people. J AdvNurs 70:1356-68.
- Kane RL, ShamliyanT, Mueller C, Duval S, Wilt TJ (2007) Nurse staffing and quality of patient care. Evid Rep Technol Assess (Full Rep) 151:1-115.
- McHugh MD, Berez J, Small DS (2013) Hospitals with higher nurse staffing had lower odds of readmissions penalties than hospitals with lower staffing. Health Aff(Millwood) 32:1740-1747.
- Peltokoski J, Vehviläinen-Julkunen K, Miettinen M (2013) Newly hired nurses' and physicians' perceptions of the comprehensive health care orientation process: a pilot study. J NursManag 23: 613-622.
- Joint Commission International.
- Hart T (2013) Promoting hand hygiene in clinical practice. Nurs Times 109:14-15.
- West P, Sculli G, Fore A, Okam N, Dunlap C, et al. (2012) Improving patient safety and optimizing nursing teamwork using crew resource management techniques. J Nurs Adm 42:15-20.
Relevant Topics
- Chronic Disease Management
- Community Based Nursing
- Community Health Assessment
- Community Health Nursing Care
- Community Nursing
- Community Nursing Care
- Community Nursing Diagnosis
- Community Nursing Intervention
- Core Functions Of Public Health Nursing
- Epidemiology
- Epidemiology in community nursing
- Health education
- Health Equity
- Health Promotion
- History Of Public Health Nursing
- Nursing Public Health
- Public Health Nursing
- Risk Factors And Burnout And Public Health Nursing
- Risk Factors and Burnout and Public Health Nursing
Recommended Journals
- Epidemiology journal
- Global Journal of Nursing & Forensic Studies
- Global Nursing & Forensic Studies Journal
- global journal of nursing & forensic studies
- journal of community medicine& health education
- journal of community medicine& health education
- Palliative Care & Medicine journal
- journal of pregnancy and child health
Article Tools
Article Usage
- Total views: 16851
- [From(publication date):
February-2016 - Jul 19, 2025] - Breakdown by view type
- HTML page views : 15492
- PDF downloads : 1359