Burkitt’s Lymphoma of the Head and Neck in the Pediatric Population: 10 Years’ Experience in ENT Department of the Teaching Hospital in Dakar (Retrospective Study)
Received: 22-Jan-2019 / Accepted Date: 13-Feb-2019 / Published Date: 20-Feb-2019 DOI: 10.4172/2161-119X.1000362
Abstract
Objectives: Clarify the incidence of Burkitt’s lymphoma (BL) during the last 10 years in Senegal.
Design, setting and participants: This descriptive study covering a 10 year period saves cases admitted in the ENT department of the academic hospital of Dakar between 1994 and 2004. It reports the characteristics and difficulties of the management.
Main outcome measure, results: This retrospective study involved 11 patients. The mean age was 9 years. The clinical characteristics were as follows: the majority of patients presented a tumor of the facial bones (10 cases) and only 2 had dental signs. The wolof ethnic group was the most affected. In 6 cases (54%), the maxilla was the site of the tumor. Half of the patients had a of hypochromic microcytic anemia; 8 patients received chemotherapy with cyclophosphamide and 50% had a complete remission.
Conclusion: This is a series relating the frequency and other characteristics of Burkitt’s lymphoma (LB) in the academic ENT department of Dakar in Senegal. There is a gradual disappearance. This retrospective series shows a marked decrease of the LB‘s incidence in Senegal. Senegal could be ranked today among the countries where LB is not endemic. This is the witness of the efforts made in the field of public health by government.
Keywords: Burkitt’s lymphoma; Children; Prevalence; African belt
Introduction
This is a hematological malignancy characterized by monoclonal B cell proliferation, it is a non-Hodgkins lymphoma (NHL) high degree of malignancy. Its former name is the Lymphatic Reticulo-Sarcoma. This retrospective study is descriptive and aims to report data from 10 years of experience in Senegal. The purpose of the study is mainly to show the decrease of cases of LB in maxillofacial location in Senegal. This retrospective study cannot point to etiologies or discoveries that have clinical and therapeutic implications. It tries to find an explanation for the progressive disappearance of maxillofacial localization.
Patients and Methods
The study is retrospective covering a period 10 years (1994 to 2004), during which all patients with LB files (20 files) were investigated and 11 were selected. Epidemiological, clinical, paraclinical, therapeutic and evolutionary are presented. Ethical considerations were done with informed consent.
Results
Epidemiological aspects
The series consisted of 11 cases over a period of 10 years so a frequency of 1 case per year. The average age was 9 years old. Sex ratio was 1. The average time of consultation was 4 and half months.
In terms of geographical origin, the wolof ethnic group was the most affected with 6 cases.
The remaining was: (Mandingo: 1 case, Diola: 1 case, Serere: 1 case, Peul: 1 case, Tukulor: 1 case)
Past history
We observed tooth extraction (1 case), facial trauma (1 case), inbreeding (2 cases) were recognized.
Clinical aspects
Reasons for consultation: The majority of patients consulted for a facial mass in 10 cases either (90%), dental signs in 2 cases (18.2%), impaired general condition in 1 case (9%) and neck lymphadenopathy in 1 case (9%).
Distribution of LB’s site: Facial and extra facial location.
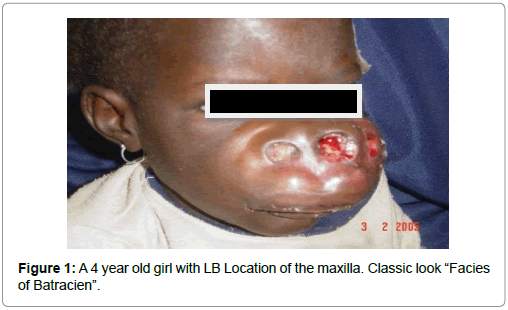
Maxilla was preferred initial tumor location of Burkitt lymphoma: 6 cases or 54%; then it touched the mandible in 3 cases or 27.2% and finally the two bones (maxilla and mandible) in 2 cases or 18.8%. (Figures 1 and 2). Extra-facial sites were in 2 cases the spleen, liver and skeleton in 1 case.
Distribution of nodal sites: Cervical lymph nodes enlargement was found in 3 children: 27% and in one case (9%) it was a extra cervical lymphadenopathy.
Clinical investigations
Hypochromic anemia was found in 6 patients (54.5%).
Panoramic radiography objectified images of osteolysis 1 times.
Two (2) patients had an abdominal ultrasound: 18.2%.
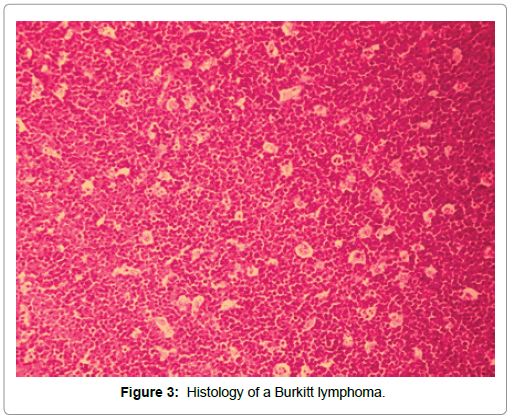
Anatomical pathology results were obtained through a needle aspiration biopsy in 2 patients (18.2%) and tumor biopsy in 9 patients (81.8%). Cytology found the “cell Burkitt” and in biopsy specimens: A “starry sky” look (Figure 3).
Distribution Murphy classification: Therapeutic data
A chemotherapy was instituted in 8 children cyclophosphamide, oncovin, Natulan and others). Adjuvant 2 where TS. An emergency tracheotomy was done in 2 children (Table 1).
| Stages | Number of cases | Percentage % |
|---|---|---|
| I | 4 | 36,3 % |
| II | 3 | 27,2 % |
| III | 4 | 36,3 % |
| IV | 0 | 0 |
Table 1: Distribution of cases of Burkitt lymphoma of the series as Murphy classification.
Scalable data or follow data: In the short term, 1 Death has been reported. Survival has been reported in 4 children (36%). 4 Four patients had a transfer in Pediatrics. The long-term complete remission was reported in 4 patients 4 cases (36%) and 2 patients were lost to follow (18%) (Table 3).
| Etiology aspect | Authors | |
|---|---|---|
| Rainy saison predisposing/ hight EBV transmission | Muwazi et al. [11] | |
| Malnutrition | Ajayi et al. [1] | |
| Parasitic infections | Ajayi et al. [1] | |
| Repeated immune stimulation in fragile patient | Rafaramino et al. [8] | |
Table 3: Etiology aspect evoked in litterature.
Discussion
Epidemiology
The geographical distribution of LB is well known. There are three areas:
• High incidence area (endemic forms LB): African belt
• Low incidence area (sporadic) (Europe, USA)
• Intermediate impact area (North Africa, South America).
In Africa, in “Burkitt tumor belt,” There are areas where the LB rampant than in others like Nigeria where Ajayi et al. [1] reported a rate of 38.3% of LB on a set of 47 orofacia l malignancies in children and in Papua New Guinea 64% of LB are reported of 67 tumors [2]. In Libya, the incidence seems to be lower [3].
Burkitt and O’Conor [4] reported in the 1960s that LB was 40 to 70% of childhood cancer in Africa. The Senegal belongs to the “Burkitt tumor belt” between Southern Africa and North Africa and occasionally a work devoted to head and neck cancers of the child, Diop [5] was estimated at 100% LB over 5 years.
Comparisons with others studies
Most retrospective series in black Africa range from 1990 to 2000 and reported that the LB is the most common tumor in children (Table 2).
| COUNTRY /period of study | Cameroon 1988-1992 [6] |
Burkina-Faso 10 years [7] |
Gabon 10 years [7] | Gabon 1980-1986 six years [7] |
Ivory coast 10 years [8] | Togo, 10 years [9] | Senegal 1977-1958 years [5] |
Senegal 10 years 1994-2004 Notre série |
Uganda [10] 1969-2006 |
|---|---|---|---|---|---|---|---|---|---|
| Number of cases | 39 | 39 | 21 | 66 | 195 | 28 | 33 | 11 | 2497 |
| Number of cases per year | 10 | 4 | 2 | 11 | 20 | 3 | 4 | 1 | 67 |
Table 2: LB series in some African countries.
To believe the numbers, there was a marked decrease in cases, two decades after in Senegal, in fact, the current series (1994-2004) found 11 cases in 10 years: 1 case per year; compared to the DIOP series [5]. Then, since 2004 until 2015, the ENT department of Dakar recorded only 2 cases of LB in Head and Neck. Locations were exceptional at the mastoid and in the nasopharyngeal space. In Senegal, LBs with maxillofacial location were the subject of very few publications before 1990. M DIOP reporting 33 cases in 8 years [5] it is the most important work published in Senegal. After a review of the more recent literature, there are 15 cases of maxillofacial LB followed by haematoclinics diagnosed before 1998 [6,7]. The report is also made by the onco-pediatricians of the important center of Aristide Le Dantec, the abdominal forms take over. Unfortunately no comparative study is published at home.
What causes to the disappearance of the head and neck LB in our country? What are the factors affecting the epidemiology of childhood ENT cancer? Several studies showed that LB would be linked to the virus Ebstein Barr [8]. In Madagascar [8] and Uganda [9-11], seasonal predisposing factors were responsible. For South African series, Madagascar and Malawi, there would be more of LB during the rainy season, period of highest transmission (EBV vectors) [11]. While Nigerian [1] and Ugandan [11] studies show more than LB during the dry season. Thus, the explanation is the conjunction, at this age, of malnutrition, frequent parasitic infections and multiple and repeated immune stimulation in an immunologically immature and fragile terrain [8].
Senegal has known for 10 years more increased drought, -this would be one reason for the decline in the LB in our country. Among other causes, this decrease would it be a sign of:
• Better health coverage
• -Fight against malaria vectors
• Better life (given that it is children from disadvantaged social layer with low social economic level that are most affected)
• Climate change.
Table 2 shows that the distribution of LB within the “belt”, in the last decade for other African countries remains disparate. There is a singularity of the panorama of the pediatric head and neck oncology in Senegal with the resurgence of squamous cell carcinoma in children (cancers of the hypopharynx [12]), at the expense of lymphomas.
Clinical stages
The average age of onset of Burkitt lymphoma varies according to studies, it is 4 years in a Cameroonian study [7] and 8 years in Togo [10]. The predominance of clinical stages III of Murphy in our series is observed in other African series [7]. It is explained by the late period before the medical visit: 4½ months in our series and 15 days to 3 and a half months in Madagascar [8], allowing time for the disease to develop. All studies report a male predominance [7].
The African form is characterized by a maxillofacial swelling; our series reports a preferential involvement of the upper jaw. The overlying skin is stretched, shiny. There is almost never ulceration. Clinical manifestations depend on the location of LB with “swelling cheek and upper jaw involvement”. Sometimes nasal obstruction in a child may be the only first event [13,14]. Other unusual locations such as the tonsil or parapharyngeal space, parotid space or sphenoid sinuses are reported in the literature. Orbital Extensions (rarely primitive) and the nasal passages are also published [15-17].
Apart pathological anatomy, others common diagnostic tests are hemogram, renal balance sheet, uric acid and EBV serology and HIV. Imaging including: x-ray bone (bone, chest), lumbar puncture and finally a myelogram ultrasound (liver kidneys, spleen, ovaries, adrenal glands, testicles).
Treatment protocols vary: VMCA, CMA, CM, CM strengthened. Ivory coast teams were awarded with the CMA, 76% remission. [9] While Moroccan series received LMB89 protocol (high doses of cyclophosphamide, vincristine, doxorubicin and prednisone) 68% of remission [13].
In Senegal, the assessment of treatment outcomes is difficult because of the large number of lost to follow the cure of attack and the lack of feedback from patients transferred in pediatrics. For a long time, accessibility problems to treatment have lowered the prognosis, Senegal today have a pediatric oncology unit belonging to the Franco- African Pediatric Oncology Group using cyclophosphamide alone in LB of Children in Senegal [18].
Conclusion
Changing epidemiology of head and neck cancers of the child in Senegal is noted, the LB in head and neck presentation seems to disappear into tumors of the head and neck for ten years. The situation in other African countries LB would be interesting to know, to see if the differences in the incidence of LB linked to geographical distribution are still relevant.
Key points
• Epidemiology of neck cancer of the child in Senegal is changing.
• As this study demonstrates such decrease of the incidence of the Burkitt’s lymphoma comparing with previous studies and compared to other African countries.
• Reasons of this decline may have socioeconomic explanations.
References
- Ajayi OF, Adeyemo WL, Ladeinde AL, Ogunlewe MO, Omitola OG, et al. (2007) Malignant orofacial neoplasms in children and adolescent: A clinicopathologic review of cases in a Nigerian tertiary hospital. Int J Pediatr Otorhinolaryngol 71: 954-963.
- Dubey S, Sengupta SK, Kaleh LK, Morewaya T (1998) Paediatric head and neck lymphomas in papua new guinea: A review and analysis of 67 cases. Int J Pediatr Otorhinolaryngol 43: 235-240.
- Elarbi M, El-Gehani R, Subhashraj K, Orafi M (2009) Orofacial tumors in Libyan children and adolescents. A descriptive study of 213 cases. Int J Pediatr Otorhinolaryngol 73: 237-242.
- Burkitt D, O'Conor GT (1961) Malignant lymphoma in African children. I. A clinical syndrome. Cancer 14: 258-269.
- Diop EM, Ndiaye IC (1987) Burkitt's lymphoma in Senegal about 33 cases. Inter Fac Afrique 1: 11-12.
- Diop S, Deme A, Dangou JM, Ndiaye FS, Toure AO, et al. (2004) Non-Hodgkin's lymphoma in Dakar: Study of 107 cases diagnosed between 1986 and 1998. Bull Soc Pathol Exot 97: 109-112.
- Doumbé P, Mbakop A, Essomba Mboumi MT, Obama MT, Kago I, et al. (1997) Burkitt's lymphoma in children in Cameroon: Descriptive and anatomoclinical aspects. Bulletin du Cancer 84: 379-383.
- Rafaramino F, Maminirina RAM, Razafindrabe JAB, Rabarijaona L, Randriamampandry A, et al. (2001) Aspects épidémiologiques du lymphome de Burkitt de l’enfant à Madagascar. Bull Soc Pathol Exot, 94: 385-388.
- Koffi KG, Bosson NM, Aka-Adjo MA, Diop S, N’dhatz E, et al. (1997) Résultats du traitement du lymphome de burkitt africain expérience du service d’hématologie clinique du chu de yopougon. Médecine d'Afrique Noire 44: 635-639.
- Segbena AY, Kueviakue M, Vovor A, Tatagan-Agbi K, Assimadi K, et al. (1997) Le lymphome de burkitt au Togo aspects épidémiologique, clinique, thérapeutique et évolutif. Médecine d'Afrique Noire 44: 141-145.
- Muwazi L, Rwenyonyi C, Kutesa A, Kasangaki A, Kamulegeya A (2014) Seasonality of Burkitt's lymphoma in Uganda. J Oral Maxillofac Pathol 18: S6-6S10.
- Ndiaye IC, Diom ES, Diop F, Tall A, Ndiaye M, et al. (2009) Squamous carcinoma of the hypopharynx in children in Senegal: Between disarray and enigma. Int J Pediatr Otorhinolaryngol 73: 357-361.
- Madani A, Benhmiddoune L, Zafad S, Harif M, Quessar A, et al. (2005) Treatment of childhood Burkitt lymphoma according to LMB89 protocol in Casablanca. Bull Cancer 92: 193-198.
- Wu K, Majumbar S (2004) Blocked nose and snoring in a 6-year old boy. Int J Pediatr Otorhinolaryngol 68: 597-600.
- Starek I, Mihal V, Novak Z, Pospisilova D, Vomacka J, et al. (2004) Pediatric tumors in parapharyngeal space: Three case reports and a literature review. Int J Pediatr Otorhinolaryngol 68: 601-606.
- Lewis WB, Perlman PW, Ilasi J (2000) Pediatric American Burkitt's lymphoma of the sphenoid sinus. Otolaryngol Head Neck Surg 123: 642-644.
- Poulsen P (1982) Burkitt’s lymphoma in tonsil. Int J Pediatr Otorhinolaryngol 4: 349-335.
- Harif M, Barsaoui S, Benchekroun S, Bouhas R, Doumbé P, et al. (2008) Treatment of B-cell lymphoma with LMB modified protocols in Africa--report of the French-African Pediatric Oncology Group (GFAOP). Pediatr Blood Cancer 50: 1138-1142.
Citation: Diom ES, Ndiaye C, Ndiaye IC, Tall A, Ndiaye M, et al. (2019) Burkitt’s Lymphoma of the Head and Neck in the Pediatric Population: 10 Years’ Experience in ENT Department of the Teaching Hospital in Dakar (Retrospective Study). Otolaryngol (Sunnyvale) 9:362. DOI: 10.4172/2161-119X.1000362
Copyright: © 2019 Diom ES, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4342
- [From(publication date): 0-2019 - Dec 02, 2025]
- Breakdown by view type
- HTML page views: 3457
- PDF downloads: 885