Research Article Open Access
CAD-CAM Ceramic Crown Retention of Resin Cements
Kojic DD*, Singhal S and Shah SUniversity of Alabama at Birmingham, Birmingham, AL, USA
- Corresponding Author:
- Kojic DD
University of Alabama at Birmingham
Birmingham, AL, USA
Tel: +1205-934-4011
E-mail: darko@uab.edu
Received date: February 07, 2014; Accepted date: April 27, 2014; Published date: May 05, 2014
Citation: Kojic DD, Singhal S, Shah S (2014) CAD-CAM Ceramic Crown Retention of Resin Cements. J Biotechnol Biomater 4:164. doi:10.4172/2155-952X.1000164
Copyright: © 2014 Kojic DD, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Biotechnology & Biomaterials
Abstract
Objectives: To measure the retention of CAD-CAM e.max (Ivoclar Vivadent) and Lava (3M-ESPE) crowns using three resin luting agents with and without surface priming. Methods: The extracted molars (n=10) were embedded in PVC cylinders with acrylic resin and placed into a lathe to produce a uniform crown preparation (20°taper). Following the orientation groove placement (69L bur), the preparations were scanned using CEREC 3D/Sirona (e.max crowns) and LAVA COS/3M ESPE (LAVA crowns).A CAD-CAM Milling Machine produced the crowns. The preparations were imaged with a digital microscope (Keyence/ VHX-600) at 20X magnification and the surface area of each preparation was calculated. The bonding area was used to calculate the bond strength by dividing the failure load with the bonded surface area. The crowns were cemented using temporary cement (RelyXTempE/3M ESPE), stored (distilled water/37°C/7days), cleaned, sandblasted (Al2O3/50 μ/35 psi/10 sec), primed and cemented. The specimens were stored (distilled water/37°C/24 h) before debonding in tension at a cross-head speed of 5mm/min (INSTRON Model/5565). The data was compared with a 2-way ANOVA and Tukey-Kramer post-hoc test (p=0.05). Results: IPS e.max: Groups bonded with primer produced higher retention compared groups bonded with no primer (p<.05). Zirconia (LAVA). Load Failure: No significant difference (p>0.05) was observed among groups except Brush and Bond/Hyperfil/ (No Primer and Metal Primer), Brush and Bond/(Hyperfil/No Primer and Secure/Metal Primer), Brush and Bond/ (Hyperfil/No Primer and Secure/Primer). Stress: No significant difference (p>0.05) was observed among groups except CandBMetabond/(No Primer; Primer) and Brush and Bond/Hyperfil/No primer, Brush and Bond/Hyperfil/(No Primer and Primer), Brush and Bond/ (Hyperfil and Secure)/(No Primer and Primer) showed significance.
Keywords
Adhesion; Biomaterials; CAD/CAM; Cements; Ceramics
Introduction
Esthetic dentistry, driven by a high demand for esthetically appealing and naturally looking restorations (especially all-ceramic restorations) has become a segment of dentistry which has experienced tremendous improvements in recent years [1,2]. In the meantime, demand for metal-ceramic restorations has dropped significantly, mostly due to lower esthetics, allergic reactions, or sensitivity to various metals [3-5]. These drawbacks, along with the high material and labor costs associated with the metal substrate fabrication (particularly noble metals), have prompted the development of new all-ceramic systems that do not require metal, yet have the high strength, precision fit, superior esthetics and optical properties not seen in metal-ceramics systems [6-8].One successful story was Ivoclar Vivadent’s patented lithium disilicate material, which exhibits superior esthetics and durability combined with satisfactory physical properties. When fabricated to full-contour, the monolithic structure is the most robust ceramic system tested to date [9]. The opalescence, translucency and light diffusion properties of IPS e.max lithium disilicate were all designed to replicate natural tooth structure for aesthetically pleasing and undetectable restorations. The blocks are produced by a massive casting on a continuous manufacturing process that is based on glass technology. This new technology uses optimized processing parameters, which prevent the formation of defects (pores, accumulation of pigments, etc.) in the bulk of the ingot [10]. Partial crystallization ensures that the blocks can be processed in a crystalline intermediate phase, which enables fast machining with CAD/CAM systems (blue, translucent state) [11]. The partial crystallization process leads to a formation of lithium metasilicate crystals Li2SiO3, which are responsible for the material’s good processing properties, relatively high strength and good edge stability [12]. Following the milling procedure, the restorations are tempered and thus reach the fully crystallized state. In the course of this process, lithium disilicate crystals (Li2Si2O5) are formed, which impart the ceramic object with the desired high strength [10]. Furthermore, due to a demand for posterior segment all-ceramic restorations, 3M ESPE has developed their patented version of Yttrium Tetragonal Zirconia Polycrystal(Y-TZP)- based systems, which are a recent addition to the high-strength, allceramic systems used for crowns and fixed partial dentures [13]. CAD/ CAM-produced, Y-TZP-based systems are in considerable demand in esthetic and stress-bearing regions [14]. The esthetic nature of zirconia, coupled with its superior physical properties and biocompatibility have resulted in restorative systems that meet the demands of today’s patients. Undoubtedly, these all-ceramics systems are considered to be prospective replacements for metal-ceramic restorations [15]. Allceramic restorations also benefit from technologies that automate aspects of their fabrication [16]. Automation implies less reliance on the skill of the individual ceramist, as well as greater homogeneity and lower probability of defects within the material itself [17]. Additionally, all-ceramic, adhesively retained restorations have been shown to demonstrate superior optical properties over porcelain metal
restorations [18]. The evolution of digital technology and computeraided design/computer-aided manufacture (CAD/CAM) systems now offers the opportunity to avoid traditional, analog impressions, including the materials, timeand handling limitations associated with usual impressions [19]. Intraoral scanners have the potential to offer excellent accuracy, with a more comfortable experience for the patient, as well as a more efficient workflow for the office [20,21]. The bonding of ceramic to dental tissue is based on the adhesion of luting cement to the ceramic substrate, together with the adhesion of luting cement to enamel and/or dentin. Although adhesive cementation is recommended for all-ceramic restorations [22,23] especially for the posterior quadrant restoration, a long-term durable bond to the ceramics is imperative for long-term successful restoration [24,25]. Bonding to silica-free oxide ceramics requires other methods than those traditionally used for silica-based ceramics, such as hydrofluoric acid etching and silane application [26,27]. Recommended methods include the use of phosphate monomer-containing (MDP) composite resins, or silica coating and silane application [28]. Short term laboratory results on bonding to zirconia ceramic showed that silica coating and silane application improved the bond strength significantly [29]. Failure analysis of debonded crowns and dentin surfaces identified the need for a reliable conditioning method to strengthen this critical area [30]. Data on the long-term durability of bonding to zirconia ceramics with newly developed primers is consistent [31]. Retention of the single-unit crowns is also dominated by the taper angle-the angle of convergence between the opposing axial walls. The retention of bonded crowns has been shown to depend on the taper angle: the smaller the taper angle, the higher the retention [32]. The maximum retention is obtained between 60 and 120 taper [32]. In practice, ideal axial wall convergence may not be routinely obtained. Studies have reported mean taper angles ranging from 30 to 260 respectfully [33]. However, a recent study confirmed that neither the surface conditioning type, nor the taper angle affected the retentive strength of IPS e.maxpress single-unit crowns when cemented adhesively [34]. Dental adhesives and cements are a complex mixture of ingredients designed to provide retention for a variety of materials to tooth structure. These materials must interact with enamel, dentin and the restorative material. The development of 4-META (included in Parkell’s C and B Metabond system) has led to a wide variety of adhesives and cements over the past few decades-all of which have consisted of the same essential ingredients and have provided outstanding consistency and predictability of boding to dentin [35,36]. The purpose of this study was to evaluate the relative retention of bonded zirconia and lithium disilicate CAD-CAM copings using three different resin cements, with and without surface priming. The hypothesis was that conditioning intaglio surfaces of all-ceramic copings would positively influence relative retention of bonded Lava or IPS e.max CAD/CAM copings.
Materials and Methods
The materials utilized and their characteristics are listed in Table 1. Specimens were assigned to the A) IPS e.max (CAD/CAM monolithic Lithium Disilicate) with8 subgroups, consisting of 10 specimens per subgroup and 80 specimens in the total group and B) LAVA (CAD/ CAM monolithic Zirconia) with 12 subgroups, consisting of 10 specimens per subgroup, with 120 specimens in total per group. However, due to initial problems with the C and B Metabond material, specimens in that subgroup were repeated and data was combined in the final analysis. Therefore, the total specimen number that was tested in both groups was 210. All intaglio surfaces of all-ceramic copings were sandblasted and assigned to subgroups with or without surface priming. Specimens were treated according to the specific protocol for each subgroup group (n=10), for three variables: Luting Cement, Dentin Conditioning and Ceramic Conditioning as listed in Tables 2 and 3.
| Material | Manufacturer | LotNo. | Exp. Date |
|---|---|---|---|
| MTL-V Primer | Parkell | VG1 | 2013-02 |
| E.F Silane Primer | Parkell | TV1 | 2012-09 |
| C&B Enamel Etchant | Parkell | VT2 | 2013-08 |
| C&B Dentin Activator | Parkell | TT-10348 | 2013-12 |
| C&B Base | Parkell | VV1 | 2013-09 |
| C&B Catalyst | Parkell | VX1 | 2013-11 |
| C&B Base | Parkell | VS1 | 2013-07 |
| SEcure Resin Cement | Parkell | VV3 | 2012-09 |
| SEcure Dental Primer | Parkell | VS1 | 2012-07 |
| Brush & Bond Liquid | Parkell | TV3 | 2012-09 |
| Brush & Bond Micro Brush | Parkell | TS22 | 2012-07 |
| Hyperfil Resin Cement | Parkell | HE11094/11094-UN | 2012-05 |
| RelyX Temp NEBase | 3M ESPE | 438714 | 2013-03 |
| RelyX Temp NE Catalyst | 3M ESPE | 439689 | 2013-03 |
Table 1: IPS e.max (CAD/CAM monolithic Lithium Disilicate).
| Groups (n=10) | Luting Agent | Dentin Treatment | Ceramic Surface Treatment |
|---|---|---|---|
| 1. | C&B Metabond Adhesive Resin Cement | Mixed Metabond Liquid | Etch-Free Silane Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 2. | C&B Metabond Adhesive Resin Cement | Mixed Metabond Liquid | None Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 3. | SEcure Self-etching Primer and Resin Cement | SEcure Primer | Etch-Free Silane Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec |
| 4. | SEcure Self-etching Primer and Resin Cement | SEcure Primer | None Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 5. | SEcure Self-etching Primer and Resin Cement | Brush & Bond | Etch-Free Silane Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec |
| 6. | SEcure Self-etching Primer and Resin Cement | Brush & Bond | None Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 7. | HyperFILNanofilled Restorative | Brush & Bond | Etch-Free Silane Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec |
| 8. | HyperFILNanofilled Restorative | Brush & Bond | None Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
Table 2: LAVA (CAD/CAM monolithic Zirconia).
| Groups (n=10) | Luting Agent | Dentin Treatment | Ceramic Surface Treatment |
|---|---|---|---|
| 1. | C&B Metabond Adhesive Resin Cement | Mixed Metabond Liquid | Etch-Free Silane Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 2. | C&B Metabond Adhesive Resin Cement | Mixed Metabond Liquid | MTL-V Metal Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 3. | C&B Metabond Adhesive Resin Cement | Mixed Metabond Liquid | None Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 4. | SEcure Self-etching Primer and Resin Cement | SEcure Primer | Etch-Free Silane Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 5. | SEcure Self-etching Primer and Resin Cement | SEcure Primer | MTL-V Metal Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 6. | SEcure Self-etching Primer and Resin Cement | SEcure Primer | None Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 7. | SEcure Self-etching Primer and Resin Cement | Brush & Bond | Etch-Free Silane Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 8. | SEcure Self-etching Primer and Resin Cement | Brush & Bond | MTL-V Metal Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 9. | SEcure Self-etching Primer and Resin Cement | Brush & Bond | None Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 10. | HyperFILNanofilled Restorative | Brush & Bond | Etch-Free Silane Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 11. | HyperFILNanofilled Restorative | Brush & Bond | MTL-V Metal Primer Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
| 12. | HyperFILNanofilled Restorative | Brush & Bond | None Sandblasted (Al2O3/50 µ/35 psi/10 sec) |
Table 3: Luting Cement, Dentin Conditioning and Ceramic Conditioning.
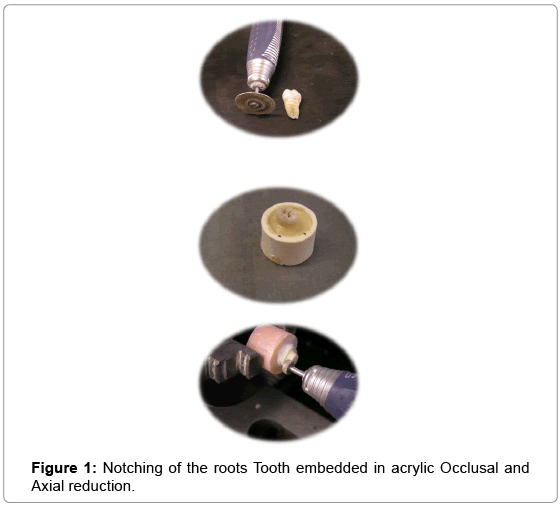
Recently extracted molar teeth were selected with diverging roots to additionally support resist removal from the embedded acrylic during test procedures. The teeth with minor carious lesions in the enamel were included only so that they could be removed during tooth preparation. The teeth were sprayed with a liquid sterilant (0.5% sodium hypochlorite), cleaned of organic debris and then further cleaned with prophy pumice and stored in a jar with tap water to prevent dehydration. Selected molars (n=10) were notched with Straight hand piece and Diamond disk Grit-Medium (Brasseler USA 918B.11.180) below the CEJ up to the tip of the root. They were approximately 1 mm deep, with 3 to 6 transverse notches that were parallel to one another. Following the notching of the roots, selected molars were embedded in PVC cylinders filled with acrylic resin. After the polymerization of the acrylic, the molars were taken out of the PVC cylinders, cleaned with alcohol wipes and then placed into a lathe. Specimens were centered into the beak of the lathe through the use of immobilized hand pieces. The uniform occlusal reduction was performed with Diamond wheel Grit-Medium (Brasseler USA 820.11.060) with 0° angulations for the entire batch of 10 specimens. After the straight hand piece angulation change, a uniform crown preparation with 20° taper, diameter and fit was produced by the Diamond flat end cylinder Grit-Medium (Brasseler USA 840.11.55).The preparations were prepared in dentin, with a mean height of 2.74 mm. All prepared crowns were kept in a jar with tap water. A unilateral orientation groove with 1mm depth was placed on the axial surface of the crown preparation using 69L bur (SS White). Figurea 1,2 and 3 depict tooth notching, embedding with acrylic and occlusal and axial reduction.
Notching of the roots Tooth embedded in acrylic Occlusal and Axial reduction Crown preparations were imaged with a digital microscope (Keyence/VHX-600) at 20X magnification and the surface area for each preparation was calculated using Keyence software over the previously captured stamp image. In order to accurately calculate the bonding area, crown preparation stamps were measured with a Digital Caliper (Neiko 6” Digital Caliper/0.001”accuracy) to obtain the surface of the stamp, which was included in the formula to calculate values for the bonded surface area. The bonding area was used to calculate bond strength by dividing the failure load with the bonded surface area. The previously described method of the preparation of 10 specimens was repeated until all 210 crown preparations were completed. Crown preparation assigned to the IPS e.max group was scanned by a Cerec 3 CAD/CAM scanner utilizing Cerec V. 2.8 software, which in turn produced the desired 3D images. The goal was to create copings with no occlusal anatomy, in order to maximize the height of the copings as much as the height of the e.max blocks would allow it. The computer images of the copings were transmitted to the milling machine, which then produced desired copings out of C-14 e.max blocks. Milled copings were tried in on the preparation stamps and checked for marginal integrity and lack of visible surface defects. A perforation was cut through-out the middle height of the copings, perpendicular to the long axis of the copings, with a high speed headpiece and notorious water spaying with a Diamond bur (SS White/Piranha 847KR-018C). The perforation that was cut was necessary for the engagement of the metal rod during the crown debonding procedure. It was easier to cut the hole in this stage of blue e.max coping (semi-sintered), rather than on fully sintered coping. After the inspection of the hole diameter (by placing a metal rod into the preparation to verify patency and proper projection of the hole in terms of the perpendicular pathway compared to the crown axis) these e.max copings were put into the furnace (Programat P300/ Ivoclar-Vivadent) for the final ceramic crystallization. After the cooling of the fully sintered e.max copings, they were matched with crown preparations and were numbered and randomly assigned to 8 e.max experimental sub-groups. However, crown preparations assigned to Lava groups were numbered and scanned with a Lava COS scanner. After the creation of the desired 3D copings images on the Lava COS computer, the files were sent to a commercial lab for the CAD-CAM milling and Lava copings production, a design which would include a central hole for a metal rod which would be engaged during the debonding process. When these Lava copings arrived from the lab, they were paired with the corresponding matching crown preparations, checked for the margin fit and absence of any visual structural voids and then were ready to be assigned to the appropriate Lava experimental groups. All copings and their matching crown preparations (e.max or Lava) were cemented using temporary cement (RelyXTempNE/3M ESPE) that was stored (in distilled water/37°C/7days). After 7 days of storage in an incubator at 37°C, the copings were removed from the preparations, cement was removed mechanically from both surfaces using a scalpe land the prepared teeth and copings were cleaned with pumice flour and alcohol for 30 seconds. Prior to bonding, all ceramic copings were ultrasonically cleaned and sandblasted (Al2O3/50 μ/35 psi/10 sec), followed by a meticulous water washing and air drying. The copings were individually fitted on the tooth and margins were checked for opening and fit (explorer does not catch). Teeth preparations and copings were primed as per the above section entitled “Experimental Groups”. The copings were bonded following the manufacturer’s instructions for each product. A 6 lb. weight was placed on the cemented copings during setting and excess cement was carefully removed with glycerin-soaked gaze. The margins were light cured for 20 sec. (HyperFIL and SEcure experimental groups only) from four directions (mesial, distal, buccal and lingual) using an Elipar S10 (3M ESPE) dental curing light with the Intensity of 1,100 mW/cm². The cemented copings were allowed to further set in tap water at 37°C for 24 hours before loading and debonding. The manufacturer’s instructions for the coping cementations are listed in Table 4.
| Material | Directions |
|---|---|
| MTL-V Primer (Parkell) | Clean crown surface with alcohol gauze. Rinse and air dry. Ultrasonically clean crown in water. Air dry.Sandblast crown interface (Al2O3/50 µ/35 psi/10 sec)Using a micro brush, apply 2 coats ofMTL-V Primer.Allow surface to dry for 60 sec. Cement as per experimental group requirements (LAVA crowns only) |
| Etch-Free Silane Primer (Parkell) | Clean crown surface with alcohol gauze. Rinse and air dry. Ultrasonically clean crown in water. Air dry.Sandblast crown interface (Al2O3/50 µ/35 psi/10 sec) Mix a drop of each Etch-Free bottle A+B in a 1:1 ratio for 15 sec. Apply a thin layer of the primer to the crown interface. Air dry for 10 sec. Apply a second layer of the primer and air dry for 10 sec. Cement as per experimental group requirements . |
| C& B Metabond Adhesive Cement (Parkell) | Clean the crown preparation with alcohol gauze. Rinse and air dry. Ultrasonically clean the preparation in water. Air dry. Etch enamel surfaces for 30 seconds with a micro brush saturated with the orange Enamel Etchant. Dab the enamel surface with the brush. Do not scrub it. Avoid overruns onto the dentin. Rinse off the Enamel Etchant and air dry. Apply the green Dentin-Activator (either gel or liquid) to dentin for 10 seconds. Thoroughly rinse off the activator and dry the tooth with a gentle burst of air. Avoid over drying and desiccation. Remove the ceramic mixing dish from the freezer. Holding the bottle vertically, dispense 4 drops of C&B-Metabond Quick base (blue cap) into one well of the chilled ceramic mixing dish. Holding the syringe vertically, add one drop of catalyst to the base liquid and stir gently for several seconds (no more than 5 seconds). Paint both tooth and casting with the mixed liquid. Add 2 level scoops powder to the mixed liquid (4 drops of base and 1 drop of catalyst).Gently stir powder and liquid for 5 seconds to create creamy cement. Apply the cement to the restoration, and seat it as quickly as possible. Apply a drop of base only (blue cap) to a cotton pellet and wipe away excess cement. Apply weight and hold ceramic crown until the material has completely set. (5-6 minutes). |
| SEcureDental Primer (Parkell) | Clean the crown preparation with alcohol gaze. Rinse and air dry. Ultrasonically clean a preparation. Air dry. Dispense several drops of SEcure Self-Etching Primer into the well, and brush one generous coat onto the preparation. Leave for 10-20 seconds and then gently air dry the liquid for 5 seconds. Do not light cure. |
| SEcure Resin Cement (Parkell) | After the priming of the tooth surface, remove the cap or previous mixing tip from the SEcure Adhesive Resin Cement syringe and bleed enough out to assure that the cement in both barrels is flush with the front edge of the orifices of the syringe. Attach a 4:1 mixing tip, bleed a small amount of cement onto pad, and dispense directly into restoration. Fully seat restoration onto the preparation and allow excess to extrude from all margins. Place weight and hold restoration in place, and remove gross excess cement while it is soft using glycerin-soaked cotton pellets. Wait 5 minutes for a complete self-cure before the final cleanup and occlusal adjustment. The final cure time can be shortened for translucent restorations with a 20 second exposure from four directions (mesial, distal, buccal and lingual) with any dental curing light. |
| Brush & Bond Bonding System (Parkell) | Clean crown preparation with alcohol gauze. Rinse and air dry. Ultrasonically clean the preparation in water. Air dry. Dispense 1-3 drops of BRUSH&BOND Liquid into the mixing well and stir for 2 seconds with an “Activator Microbrush” Activated B & B liquid. The mixing well should be covered and used within 3 minutes. Apply activated liquid onto prepared tooth surfaces and keep moist with liquid for 20 seconds. Evaporate the B & B solvents with a gentle air stream for 10 seconds. Light-cure the remaining B & B resin with LED curing light for 10 sec. |
| HyperFIL DC Resin Cement (Parkell) | After priming the tooth and crown surface, place the HyperFIL cartridge into the dispensing gun. Bleed a small amount of material onto a pad to assure that material is flowing from both orifices. Place the intraoral tip into the bottom of the preparation to avoidtrapping air and slowly express the composite as you withdraw the tip. Keep the tip immersed in the HyperFIL until the prep is adequately filled to eliminate air entrapment. Fully seat restoration onto the preparation and allow excess to extrude from all margins, remove the excess. Light cure the surface for at least 40 seconds with an LED light. |
| RelyXTemp NE TemporaryCement (3M ESPE) | Clean the crown preparation and the intaglio surface of the crown with alcohol gaze. Rinse and air dry. Ultrasonically clean the preparation and the crown. Air dry. Dispense two equal lengths of base paste and catalyst on a mixing pad. Use a plastic spatula to thoroughly mix the paste for 30 seconds until a homogeneous consistency is created. By overdosing the catalyst, the bonding strength is increased and the working time is prolonged. Apply a thin layer of cement on the surface to be cemented, and place the dental restoration with slight pressure. Apply weight, remove excess and wait 4 minutes to set. |
Table 4: Manufacturer’s instructions for the coping cementations.
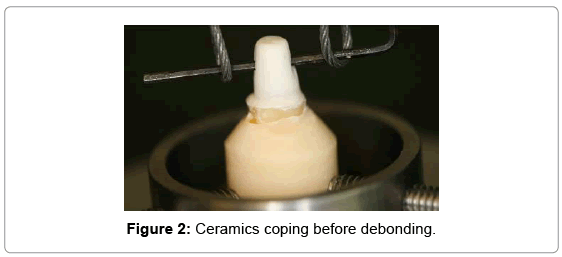
Figures 2 and 3 depict ceramic coping secured with the acrylic base in the clampduring tensile testing in an Instron testing machine (Instron u Model/5565). The upper part of the ceramic coping, with the hole, metal rod and interconnecting wire, is engaged with an upper clamp and ready for debonding testing.
The specimens were attached to the grips of the testing machine (Instron, Model 5565/Canton, MA) and loaded in tension at a crosshead speed of 0.5 mm/min until debonding occurred (Table 5). The peak force (N) to debond each crown was recorded. The surface area of the prepared teeth was measured and the bond strength was calculated from the peak failure load and bonding area. Examination of the failure site was examined optically with loops and imaged with a digital microscope (Keyence/VHX-600) at 20X magnification. The failure pattern was classified as cohesive, adhesive, mixed, or a tooth fracture. Means and standard deviations of the failure load were calculated. Data was analyzed statistically by a one-way analysis of variance (Super ANOVA, Abacus Concepts, Berkeley, CA). Intergroup differences were determined by Tukey-Kramer intervals calculated at the 0.05 level of significance. There was only one trained operator who completed all procedures, with the exception of the Lava copings production, which was outsourced in a commercial dental lab.
| Material | Composition |
|---|---|
| C&B Metabond
Catalyst Enamel Etchant Dentin Activator |
MMA, 4-META, PMMA), partially oxidized tri-N-butyl borane (TBB), radiopaque pigments, acetone, Metal Oxide TBB / partially oxidized (TBB-O), Hydrocarbon Phosphoric acid, Polyvinyl alcohol, Water 10% citric acid, 3% ferric chloride, vinyl alcohol, water |
| Etch Free Primer | (4-META),di(meth)acrylates, acetone |
| Brush & Bond | Nylon tuft, Aromatic Sodium Sulfinate proprietary, Aromatic amine 4-META Poly-functional (meth) acrylate HEMA, acetone |
| SEcure Resin Cement Self-etching Primer |
4-META, di(meth)acrylates, HEMA 4-META, di(meth)acrylates, acetone |
| HyperFIL DC ResinCement | Zirconia (ZrO2), silica (SiO2), TMPT filler, aromatic amine, HEMA, 4-META, di(meth) acrylates, benzoyperoxide |
| MTL-V Primer | 6-(4-vinylbenzyl-n-propyl)amino-1, 3,5-triazine-2,4-dithiol (VTD), acetone |
| 4-META, 4-methacryloxyethyl-trimellitate-anhydrid; HEMA, 2-hydroxyethyl methacrylate; TBB, tri-n-butylborane; PMMA, polymethylmethacrylate; MMA, methyl methacrylate; | |
Table 5: Basic chemical composition of testing agents, with their 4-META functional group.
Figures 2 and 3 depictceramic coping secured with the acrylic base in the clampduring tensile testing in an Instron testing machine (Instron u Model/5565). The upper part of the ceramic coping, with the hole, metal rod and interconnecting wire, is engaged with an upper clamp and ready for debonding testing.
Results
A general summary of research findings is provided, followed by a more detailed analysis of each experimental section. Within the e.max experimental group, copings bonded with primer produced significantly higher retention rates in comparison to coping groups bonded with no primer (p<0.05), as presented in Graph 1.
Data extracted from these graphs shows that ceramic substrate has predominant influence in the failure mode. Thus, in the IPS e.max experimental group, the failure mode was mostly adhesive, followed by tooth fractures. However, in the Lava experimental group, the cohesive failure was the most dominant mode of failure.
Discussion
In the present study, the four bonding systems investigated demonstrated different abilities with regards to the cementation to dentin and ceramic substrates. It was evident that priming ceramic surfaces in the IPS e.max experimental group did correlate with increased retention rates; therefore, the hypothesis that the priming of ceramic surfaces would increase the retention rate was partially accepted. However, the same hypothesis was rejected with non-conclusive results with the Lava experimental group. A failure type with IPS e.max group was mainly adhesive and the occurrence was primarily distributed with non-primed ceramic surfaces. As far as Lava experimental group is concerned, the most dominant failure pattern mode was cohesive and its distribution was evenly distributed according to Graph 6. There was only one bonding system that showed identical values regardless of the ceramic substrate and that was Brush and Bond with Hyper FIL on Etch Free primed ceramic surfaces (stress 4MPa). According to the Parkell product information, all tested bonding systems contain 4-META. Adhesive systems can be either phosphate or carboxylic acid resins [37]. C and B-Metabond is a carboxylic-based acid resin that utilizes an aqueous solution of 10% citric acid/3% ferric chloride [38,39] to eliminate the smear layer and demineralize the dentin. The adhesive monomer present in C and BMetabond penetrates the demineralized dentin and forms a hybrid layer. The ferric chloride plays a key role in this process, as the polymerization of Methyl Methacrylate (MMA) is accelerated by ferric ion on the dentin surface, which may aid in reducing cure shrinkage stresses [40]. The permeability of dentin that had been conditioned with a combination of 10% citric acid and 3% ferric chloride can be high and dry [41]. In addition, the ferric ion can possibly subdue the denaturing effect of dentin collagen that had been treated with a pretreatment acid [36]. The ferric chloride hindered the collapse of the demineralized dentin and 4-META, presented in both hydrophobic and hydrophilic groups, which enhances monomer impregnation. Usually collagen is exposed as a consequence of dentin demineralization and 4-META/MMA-TBB resin will provide protection for this network. However, any areas not protected may undergo hydrolysis. Furthermore, the tensile bond strength between 4-META/MMA-TBB resin and dentin will decrease gradually over time. When NaOCl in conjunction with phosphoric acid has been used to remove the inorganic and organic constituents of dentin, the problems associated with hydrolytic attack seem to decrease, possibly as a result of the eradication of collagen from the dentin surface [35]. Unfortunately, the use of NaOCl seems to impede the polymerization of 4-META/MMA-TBB resin. The use of 10% ascorbic acid (10% sodium ascorbate) reverses this detrimental effect. This is important because a 5% solution of NaOCl is routinely used in endodontic procedures. The ascorbic acid can be used for cleaning, etching and to increase the rate of polymerization and is comparable to Ethylene DiamineTetraacetic Acid (EDTA) as a cleansing solution [42]. C and B-Metabond, usually considered as very powerful adhesive cement, did not show astronomical bond strength data. However, unlike the other cements, C and B-Metabond did not fail abruptly during the tension test. Instead, it appeared to be stretching out. However, when it was stretched beyond its limit, the bond failure occurred. The micrographs could actually show the difference between C and B-Metabond and the other resin cements. In contrast to the brittle fracture of other cements, C and B Metabonded surfaces were still coated with the adhesive and that adhesive was stretched into strange stalactites, or fins of material [32]. There was one bonding agent that performed well, regardless of ceramic substrate and that was Brush and Bond. The film thickness of 9 μm seems to have influenced the results shown in Graphs 1 and 2. Combined with either SEcure or HyperFIL, it has shown consistent results in both ceramic substrates.
Conclusion
Within the limitations of any in vitro study, the following conclusions can be drawn:
Primed IPS e.max ceramic surfaces provided significantly higher retention rates than non-primed surfaces. However, that was not the case with the Lava crowns.
The failure mode of debonded copings was mostly an adhesive type, followed by tooth fractures in the IPSe.max experimental group; however, a cohesive failure mode was the most dominant type in the Lava experimental groups.
Clinical trials are required to understand what the real performance of ceramics in the oral environment may be and what the role of luting agents and surface treatments on their performance may be.
References
- Donovan TE (2008) Factors essential for successful all-ceramic restorations. J Am Dent Assoc 139 Suppl: 14S-18S.
- Devigus A (2011) All-ceramic restorations in the esthetic zone-the problem of choice. SchweizMonatsschrZahnmed 121: 549-559.
- Benk I, Némethy M, Fábián TK (2011) [Restoration of profound tooth damage caused by intrinsic erosion, with porcelain crowns. A case report]. FogorvSz 104: 81-85.
- Thyssen JP, Menné T, Møller P, Jellesen MS, Johansen JD (2011) A cobalt spot test was useful in the diagnostic work-up of a cobalt allergic patient suffering from oral hypersensitivity to cobalt. J Am AcadDermatol 65: 659-660.
- Song H, Yin W, Ma Q (2011) Allergic palmoplantarpustulosis caused by cobalt in cast dental crowns: a case report. Oral Surg Oral Med Oral Pathol Oral RadiolEndod 111: e8-10.
- Barão VA, Gennari-Filho H, Goiato MC, dos Santos DM, Pesqueira AA (2010) Factors to achieve aesthetics in all-ceramic restorations. J CraniofacSurg 21: 2007-2012.
- Conrad HJ, Seong WJ, Pesun IJ (2007) Current ceramic materials and systems with clinical recommendations: a systematic review. J Prosthet Dent 98: 389-404.
- Bidra AS, Chapokas AR (2011) Treatment planning challenges in the maxillary anterior region consequent to severe loss of buccal bone. J EsthetRestor Dent 23: 354-360.
- Kern M. Clinical Outcome of All-ceramic Restorations. In: J-F Roulet and HF Kappert, editors Statements. Diagnostics and Therapy in Dental Medicine Today and in the Future. London: Quintessence, 2009:195-208
- Fasbinder DJ, Dennison JB, Heys D, Neiva G (2010) A clinical evaluation of chairside lithium disilicate CAD/CAM crowns: a two-year report. J Am Dent Assoc 141 Suppl 2: 10S-4S.
- Mörmann WH (2006) The evolution of the CEREC system. J Am Dent Assoc 137 Suppl: 7S-13S.
- Tsotsos S. A historical perspective of tooth preparation for CEREC technology. Oral Health. 2009;Mar:55-60.
- Piconi C, Maccauro G (1999) Zirconia as a ceramic biomaterial. Biomaterials 20: 1-25.
- Rekow D, Zhang Y, Thompson V (2007) Can material properties predict survival of all-ceramic posterior crowns? CompendContinEduc Dent 28: 362-368.
- Höland W, Schweiger M, Watzke R, Peschke A, Kappert H (2008) Ceramics as biomaterials for dental restoration. Expert Rev Med Devices 5: 729-745.
- Pieper R (2009) Digital impressions--easier than ever. Int J Comput Dent 12: 47-52.
- Henkel GL (2007) A comparison of fixed prostheses generated from conventional vs digitally scanned dental impressions. CompendContinEduc Dent 28: 422-424, 426-8, 430-1.
- Shiraishi T, Wood DJ, Shinozaki N, van Noort R (2011) Optical properties of base dentin ceramics for all-ceramic restorations. Dent Mater 27: 165-172.
- Syrek A, Reich G, Ranftl D, Klein C, Cerny B, et al. (2010) Clinical evaluation of all-ceramic crowns fabricated from intraoral digital impressions based on the principle of active wavefront sampling. J Dent 38: 553-559.
- 3M ESPE. Lava Chairside Oral Scanner C.O.S. Technical Datasheet; 2009.
- Beuer F, Schweiger J, Edelhoff D (2008) Digital dentistry: an overview of recent developments for CAD/CAM generated restorations. Br Dent J 204: 505-511.
- Suttor D, Bunke K, Hoescheler S, Hauptmann H, Hertlein G (2001) LAVA--the system for all-ceramic ZrO2 crown and bridge frameworks. Int J Comput Dent 4: 195-206.
- Suttor D (2004) Lava zirconia crowns and bridges. Int J Comput Dent 7: 67-76.
- Burke FJ, Fleming GJ, Nathanson D, Marquis PM (2002) Are adhesive technologies needed to support ceramics? An assessment of the current evidence. J Adhes Dent 4: 7-22.
- Manso AP, Silva NR, Bonfante EA, Pegoraro TA, Dias RA, et al. (2011) Cements and adhesives for all-ceramic restorations. Dent Clin North Am 55: 311-332, ix.
- Wegner SM, Kern M (2000) Long-term resin bond strength to zirconia ceramic. J Adhes Dent 2: 139-147.
- Blatz MB, Sadan A, Kern M (2003) Resin-ceramic bonding: a review of the literature. J Prosthet Dent 89: 268-274.
- Atsu SS, Kilicarslan MA, Kucukesmen HC, Aka PS (2006) Effect of zirconium-oxide ceramic surface treatments on the bond strength to adhesive resin. J Prosthet Dent 95: 430-436.
- Piwowarczyk A, Lauer HC, Sorensen JA (2005) The shear bond strength between luting cements and zirconia ceramics after two pre-treatments. Oper Dent 30: 382-388.
- Dias de Souza GM, Thompson VP, Braga RR (2011) Effect of metal primers on microtensile bond strength between zirconia and resin cements. J Prosthet Dent 105: 296-303.
- Lehmann F, Kern M (2009) Durability of resin bonding to zirconia ceramic using different primers. J Adhes Dent 11: 479-483.
- Zidan O, Ferguson GC (2003) The retention of complete crowns prepared with three different tapers and luted with four different cements. J Prosthet Dent 89: 565-571.
- Dodge WW, Weed RM, Baez RJ, Buchanan RN (1985) The effect of convergence angle on retention and resistance form. Quintessence Int 16: 191-194.
- Madina MM, Ozcan M, Badawi MF (2010) Effect of surface conditioning and taper angle on the retention of IPS e.max Press crowns. J Prosthodont 19: 200-204.
- Soeno K, Taira Y, Jimbo R, Sawase T (2008) Surface treatment with ascorbic acid and ferric chloride improves the micro-tensile bond strength of 4-META/MMA-TBB resin to dentin. J Dent 36: 940-944.
- Chang JC, Hurst TL, Hart DA, Estey AW (2002) 4-META use in dentistry: a literature review. J Prosthet Dent 87: 216-224.
- Soeno K, Suzuki S, Taira Y, Atsuta M (2005) Improvement of the bond strength of 4-META/MMA-TBB resin to collagen-depleted dentin. J Biomed Mater Res B ApplBiomater 73: 104-108.
- Nakabayashi N, Watanabe A, Gendusa NJ (1992) Dentin adhesion of "modified" 4-META/MMA-TBB resin: function of HEMA. Dent Mater 8: 259-264.
- Nakabayashi N, Hiranuma K (2000) Effect of etchant variation on wet and dry dentin bonding primed with 4-META/acetone. Dent Mater 16: 274-279.
- Imai Y, Kadoma Y, Kojima K, Akimoto T, Ikakura K, et al. (1991) Importance of polymerization initiator systems and interfacial initiation of polymerization in adhesive bonding of resin to dentin. J Dent Res 70: 1088-1091.
- Nakabayashi N, Pashley DH (1998) Evolution of Dentin-Resin Bonding. In: Hybridization of Dental Hard Tissues. Tokyo, Japan: Quintessence Publishing Co:1-20.
- Sugaya T, Noguchi H, Hasegawa Y, Tanaka Y, Kawanami M (2002) Clinical evaluation of 4-META/MMA-TBB resin as a root-end sealant following apicoectomy. Jpn J Conserv Dent. 45:62–67.
Relevant Topics
- Agricultural biotechnology
- Animal biotechnology
- Applied Biotechnology
- Biocatalysis
- Biofabrication
- Biomaterial implants
- Biomaterial-Based Drug Delivery Systems
- Bioprinting of Tissue Constructs
- Biotechnology applications
- Cardiovascular biomaterials
- CRISPR-Cas9 in Biotechnology
- Nano biotechnology
- Smart Biomaterials
- White/industrial biotechnology
Recommended Journals
Article Tools
Article Usage
- Total views: 15717
- [From(publication date):
December-2014 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 11019
- PDF downloads : 4698