Research Article Open Access
Defining the Threshold at which Health Care Professionals Consider Withdrawing Life Sustaining Ventilation in Neonatology
Sandesh Shivananda1*, Kyong-Soon Lee2, Krishelle Marc-Aurele3, Jonathan Hellmann2, Susan Braid3 and Jae H Kim3
1Division of Neonatology, Department of Pediatrics, McMaster Children’s Hospital, Canada
2Division of Neonatology, Department of Pediatrics, The Hospital for Sick Children, Toronto, Canada
3Division of Neonatology, Department of Pediatrics, University of California San Diego, San Diego, California, United States
- *Corresponding Author:
- Sandesh Shivananda
McMaster University Medical Center Division of Neonatology Department of Pediatrics
4F1D 1200 Main Street
West Hamilton
ON L8N 3Z5, Canada
Tel: 905-521-2100 ext. 73489
Fax: 905-521-5007
E-mail: sandesh@mcmaster.ca
Received date: March 21, 2013; Accepted date: April 12, 2013; Published date: April 15, 2013
Citation: Shivananda S, Lee KS, Marc-Aurele K, Hellmann J, Braid S, et al. (2013) Defining the Threshold at which Health Care Professionals Consider Withdrawing Life Sustaining Ventilation in Neonatology. J Palliative Care Med S4:001. doi:10.4172/2165-7386.S4-001
Copyright: © 2013 Shivananda S, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
Objective: To determine the variation inhealthcare provider perspectives regarding Withdrawing Life Sustaining Ventilation (WLSV) in Neonatology. Methods: We surveyed physicians, nurses, respiratory therapists, social workers, occupational and physical therapists, and neonatal pharmacists at two North American neonatal intensive care units to assess how neonatal healthcare providers use numerical risk to assist decision-making in Withdrawing Life Sustaining Ventilation. The survey presented nine scenarios depicting varying projected disabilities (single and multiple) at 3 years of age. Participants were asked to choose a predicted risk for the proposed disabilities (threshold) at which they would consider offering the WLSV option to parents. Ten additional questions regarding demographic information, attitudes, beliefs, and personal experiences were included. Results: The response rate was 59% (332/562). Respondents were primarily female nurses. For all respondents, the choice of WLSV was offered at statistically increasing frequency for the following disabilities: deafness, blindness, cerebral palsy, and mental retardation. The risk of severe mental retardation was the strongest influencing variable. The median choice for risk of severe mental retardation alone (61-70% risk) showed no significant difference from the median choice for risk of multiple disabilities (two or more). Median responses were not significantly different with respect to age, number of children, ethnic origin, occupation, religion, strength of religious belief, or knowledge of a friend/relative with impairments. Conclusions: Poor cognitive outcome is the principal determinant in WLSV decision-making among health care providers.
Keywords
Palliative care; End-of-life care; Hypoxic-ischemic encephalopathy
Abbreviations
CP: Cerebral Palsy; HCP: Health Care Provider; HIE: Hypoxic Ischemic Encephalopathy; MRI: Magnetic Resonance Imaging; NICU: Neonatal Intensive Care Unit; WLSV: Withdrawal of Life Sustaining Ventilation
Introduction
Withdrawal of life sustaining ventilation (WLSV) is an important and increasingly publicized issue in the Neonatal Intensive Care Unit (NICU) [1-4]. WLSV has been considered in two distinct settings: 1) Infants who will die imminently despite continued invasive medical technology on the grounds that death is inevitable; 2) Infants who can potentially survive but the projected quality of life after the intensive care period is poor [1-7]. For many neonatal cases, a high risk of poor outcome is determined and physicians are required to make decisions regarding treatment options [8-10]. The decision of WLSV for a neonate is affected by an interaction by an interaction of multiple factors such as the neonate’s clinical condition, social factors, as well as family and healthcare provider values [11,12].
Considering WLSV is an unexpected and unimagined event for most families [13]. Some of the factors found to be responsible for increasing parents’ distress include difficulty in getting information, failure to understand how the information provided by physicians impacts in making meaningful decisions, involvement of multiple staff members and differences of opinion, conflict between staff members regarding WLSV decision-making, and uncertainty in integrating the input of consultants [13]. A crucial factor in minimizing the stress and anxiety of parents faced with WLSV option is a consistent approach by Health Care Providers (HCP). Reaching a consensus on a threshold for consideration of WLSV among health care providers would be of significant benefit in this difficult process.
The range in risk of major handicap at which the health care provider would consider WLSV has been implied, but has not been quantified. The explicit quantification of this threshold for WLSV, derived from a large group of healthcare team members, may be useful for physicians as decision makers by providing objective and consistent guidelines for when to consider WLSV for a sick neonate. With this in mind, we developed a survey to describe how neonatal health care providers use numerical risks to assist decision-making in Withdrawing Life Sustaining Ventilation.
Methods
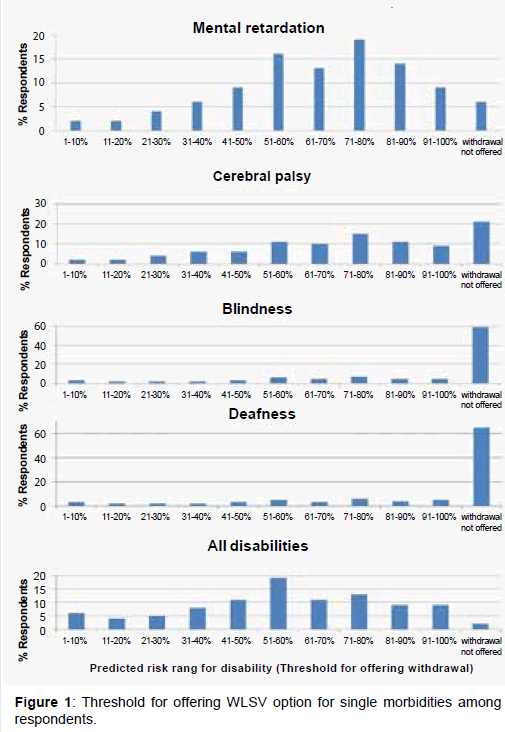
In 2007, we surveyed health care providers at two different NICU’s in North America: Sick Kids in Toronto, Canada and University of California San Diego Medical Center, USA. Surveys were collected from September 2007 to December 2007 via Survey Monkey (http://www.surveymonkey.com/). All registered staff received an email invitation to complete a web-based survey including: physicians, nurses, respiratory therapists, social workers, occupational and physical therapists, and neonatal pharmacists. A paper copy was available as an alternative format. Morbidities were classified in one of four categories as follows: 1) Severe Mental Retardation (IQ<70); 2) Significant Cerebral Palsy (unable to walk without assistance e.g. cane, walker); 3) Blindness (legally blind); 4) Severe Hearing Loss (deafness despite hearing aids). The survey presented nine scenarios depicting varying projected disabilities (single or combined morbidities) at 3 years of age for an infant requiring neonatal intensive care (Figure 1).
For each scenario, we asked the HCP to designate at what 10% risk of interval (i.e. 1-10%, 11-20%, 21-30%) would he or she offer the option to withdraw life support ventilation. The “threshold for offering WLSV” for each disability was defined as the median response of those who offered WLSV at some point. Respondents were allowed to choose, “WLSV option not offered.” Ten additional questions regarding demographic information, attitudes, beliefs, and personal experiences were included (Appendix 1).
Data was downloaded and recoded into STATA (Stata v10) for analysis. Descriptive statistics were used to determine the frequency, median, and mode for each scenario. The purpose of this analysis was to determine the “threshold for offering WLSV” for each projected disability. Since the data was nonparametric, the Kruskal-Wallis rank sum test was used to compare median responses across demographic categories (i.e. age, gender, occupation).
Results
A total of 562 health care providers were asked to participate from both sites with a total of 332 responses (59%) returned. Seventy percent (n=232) of the respondents were from Canada. The HCP demographic information is shown on table 1. The HCP respondents were predominantly female, under 40 years, and married. The most prevalent occupation was nursing. A total of 30% of the respondents were physicians. More than half of the respondents had been involved in a WLSV case within the last 3 months.
| Age | COMBINED GROUP | |
| N=332 (%) | ||
| 21-30 | 91 | (27%) |
| 31-40 | 110 | (33%) |
| 41-50 | 81 | (25%) |
| 51-60 | 45 | (14%) |
| 61-70 | 7 | (2%) |
| Gender | ||
| Female | 276 | (83%) |
| Marital Status | ||
| Never Married | 80 | (24%) |
| Married | 206 | (62%) |
| Divorced | 17 | (5%) |
| Common Law | 20 (6% | |
| Widowed | 2 (<1%) | |
| Number of Children | ||
| Zero | 163 | (49%) |
| 1 | 46 | (14%) |
| 2 | 66 | (20%) |
| 3 | 37 | (11%) |
| >3 | 13 | (4%) |
| Ethnic Origin | ||
| Caucasian | 226 | (68%) |
| Asian | 53 | (16%) |
| Latin | 10 | (3%) |
| Other | 43 | (13%) |
| Occupation | ||
| Nurse | 186 | (56%) |
| Physician | 100 | (30%) |
| NNP | 10 | (3%) |
| RRT | 33 | (10%) |
| Other | 13 | (4%) |
| WLSV experience by # cases involved | ||
| None | 23 | (7%) |
| <5 | 100 | (30%) |
| 6-10 | 60 | (18%) |
| 11-15 | 37 | (11%) |
| >15 | 113 | (34%) |
| Length of NICU Experience | ||
| >20 years | 86 | (26%) |
| 11-20 years | 40 | (12%) |
| 7-10 years | 53 | (16%) |
| 4-6 years | 56 | (17%) |
| 1-3 years | 43 | (13%) |
| <1 year | 43 | (13%) |
| Religion | ||
| Catholic | 103 | (31%) |
| Christian | 111 | (33%) |
| Atheist, Agnostic, Humanist, | 46 | (14%) |
| No Religion | ||
| No answer | 27 | (8%) |
| Islam | 15 | (6%) |
| Buddhism | 4 | (1%) |
| Judaism | 13 | (5%) |
| Friend or Relative with: | ||
| CP | 71 | (21%) |
| MR | 94 | (28%) |
| Deafness | 70 | (21%) |
| Blindness | 39 | (11%) |
Table 1: Demographic data on combined Toronto and San Diego groups.
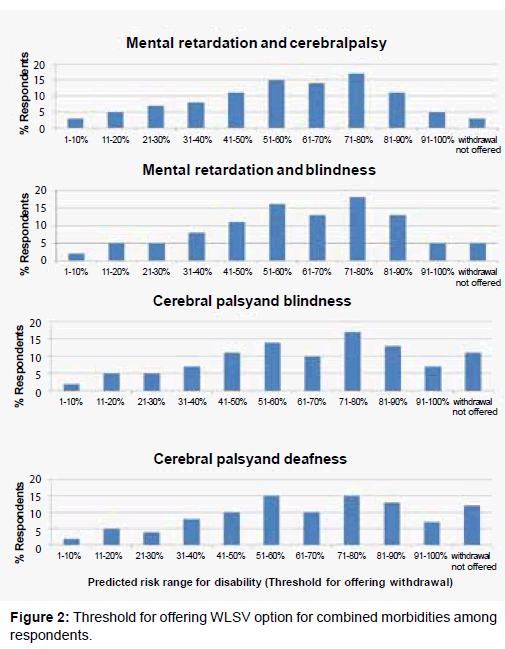
The threshold for offering WLSV did not vary significantly among single or combined disabilities (Figure 2). However, the number of those chose “WLSV option not offered,” did vary among the disabilities (Table 2). If a child had a risk of having all morbidities (mental retardation, cerebral palsy, blindness, and deafness), only 2.4% of the respondents did not offer WLSV compared to 65.7% for a child who had a risk of being deaf. Severe mental retardation was the strongest determinant for offering the withdrawal option followed by in order by cerebral palsy, blindness, and deafness.
| Percentage (n) persons | Median Threshold (n) | Mode threshold for | |
|---|---|---|---|
| Disability | who chose WLSV option | for those who offered | those who offered |
| not offered | WLSV at some risk | WLSV at some risk | |
| All 4 deficits (Mental | |||
| Retardation, Cerebral | 2.4% (8) | 61-70% (320) | 61-70% |
| Palsy, Blindness, and | |||
| Deafness) | |||
| Mental Retardation and | 3.3% (11) | 61-70% (317) | 61-70% |
| Cerebral Palsy | |||
| Mental Retardation and | 4.5% (35) | 71-80% (314) | 61-70% |
| Blindness | |||
| Mental Retardation | 6% (20) | 71-80% (309) | 61-70% |
| Cerebral Palsy and | 10.7% (35) | 61-70% (293) | 61-70% |
| Blindness | |||
| Cerebral Palsy and | 11.8% (39) | 71-80% (291) | 61-70% |
| Deafness | |||
| Cerebral Palsy | 21.2% (70) | 71-80% (259) | 81-90% |
| Blindness | 59.7% (197) | 71-80% (133) | 81-90% |
| Deafness | 65.7% (217) | 71-80% (13) | 81-90% |
Table 2: Summary of Thresholds for WLSV.
Median responses were not significantly different with respect to age, number of children, ethnic origin, occupation, religion, strength of religious belief, or knowledge of a friend/relative with impairments. Median responses were not significantly different between the two institutions.
Eighty one percent (n=269) of respondents, having a numeric risk of disability was helpful in making a decision to offer the WLSV option. Half of respondents disagreed with the statement, “Religion plays an important role in withdrawal of life sustaining care decisions.” The majority (89%) disagreed with the statement, “because human life is sacred, everything possible should be done to ensure a neonate’s survival, however severe the prognosis.”
Discussion
The grounds for offering a WLSV option to families are usually based on incomplete prognostic information, especially with regards to quality of life outcomes. Even when outcomes are known from large cohort databases, the ability to accurately predict individual outcomes remains uncertain. Our survey artificially created scenarios in which an outcome at 3 years of age was known for an infant in the NICU and respondents were asked to consider the risk for certain disabilities at which to offer WLSV to families. Our goal was to determine if a healthcare provider’s decision to offer a WLSV option could be distilled with respect to a numeric risk “threshold’ for a given disability.
Severe cognitive impairment was the single most important disability in deciding to offer WLSV for the neonate in our North American health care provider survey. Adding severe mental retardation to cerebral palsy was the only other outcome that lowered the risk threshold for respondents to offer the option to withdraw. Single sensory deficits, specifically Blindness and Severe Hearing Loss, were not reasons for most participants to consider WLSV. Surprisingly, some individuals (i.e. 40% of respondents for blindness alone and 35% respondents for deafness alone) indicated that these deficits provided sufficient grounds on which to offer the WLSV option to families. Since deafness generally does not preclude independent living, we speculated that some respondents have extreme risk aversion to any type of significant disability or some may have misinterpreted the questions asked. Dual morbidities of Severe Mental Retardation and Cerebral Palsy further shifted the “threshold for offering the WLSV” compared with Severe Mental Retardation alone, although cognitive morbidity remained the most dominant factor. The “threshold for offering WLSV” for these combined morbidities appeared to be a predicted risk greater than 50%. Sensory deficits did not impact the likelihood of offering WLSV above the mental and motor morbidities.
The finding that intellectual impairment skews the balance of benefits versus burdens against prolonging life is similar to that previously described by Wilkinson [14]. He explored three ways in which the best interests for an infant could be affected by the prediction of severe intellectual disability: 1) the disability is so severe that all concept of an infant’s best interest is meaningless; 2) the intellectual disability may impair the infant’s quality of life, causing suffering; 3) severe intellectual disability diminishes the benefits of life that will be enjoyed. If it were the case that intellectual disability rendered an infant’s best interest meaningless, then the proportion of respondents offering WLSV for infants with a predicted risk of severe mental retardation with or without other disabilities would be the same as that for infants with a predicted risk of disabilities without severe mental retardation. It appears that respondents to this survey believe that intellectual disability either impairs the infant’s quality of life or diminishes the benefits of life. Recent qualitative and quantitative studies support our finding of poor cognitive outcome being the principal determinant in offering WLSV among health care providers [1-4].
Responses were remarkably unaltered by potential biases, such as age, sex, occupation, NICU experience, religion, or institution. The NICU team appeared to be unified in deciding when to offer a WLSV option to families. Conflicts between individuals over specific cases invariably do arise in practice but the uniqueness of the close multidisciplinary environment in the NICU may contribute to agreement in most cases. The main difference between the Neonatal Intensive Care units is that UC San Diego is primarily inborn infants and Sick Kids in Toronto comprises all out born infants. However, the departments were similar in terms of the demographics and survey responses.
In reality, an infant’s risk for disability is not the sole determinant for offering WLSV. Limiting the information provided in the scenarios was deliberately artificial and simplistic. Many respondents (N=100) were not comfortable making a decision solely on a numeric risk. One respondent wrote, “Yes it is uncomfortable having to answer these questions, especially when they evoke such emotions-that change frequently…I can see myself answering these same survey questions differently, dependent upon what clinical and/or personal scenarios… also, putting a numerical value to predicted risk is sometimes not useful because certain emotional/personal/religious or philosophical factors are more qualitative than quantitative.”
In summary, our study provides a framework upon which numerical risks can be placed in the context of WLSV decision making. More data is emerging on the predictive power of early biomarkers and functional brain MRI on neurodevelopment disability. How health care providers might use these numbers to make decisions has not been adequately explored. As healthcare moves towards greater transparency in all its activities, such an ethical framework can assist in providing greater clarity to difficult healthcare decision-making. Future research will also involve distribution of this survey to more North American cities and various other countries around the world to explore cultural differences not found with this North American study.
References
- Verhagen AA, Janvier A, Leuthner SR, Andrews B, Lagatta J, Et Al. (2010) Categorizing Neonatal Deaths: A Cross-Cultural Study In The United States, Canada, And The Netherlands. J Pediatr 156: 33-37.
- Verhagen AA, Van Der Hoeven MA, Van Meerveld RC, Sauer PJ (2007) Physician Medical Decision-Making At The End Of Life In Newborns: Insight Into Implementation At 2 Dutch Centers. Pediatrics 120: E20-28.
- Verhagen AA, Dorscheidt JH, Engels B, Hubben JH, Sauer PJ (2009) End-Of-Life Decisions In Dutch Neonatal Intensive Care Units. Arch Pediatr Adolesc Med 163: 895-901.
- Moratti S (2011) Non Treatment Decisions On Grounds Of "Medical Futility" And "Quality Of Life": Interviews With Fourteen Dutch Neonatologists. 26 Issues L. & Med 3.
- Moratti S (2010) End-Of-Life Decisions In Dutch Neonatology. Med Law Rev 18: 471-496.
- Sauer PJ, Dorscheidt JH, Verhagen AA, Hubben JH, European Neonatal Eol Study Group 2010. Medical Practice And Legal Background Of Decisions For Severely Ill Newborn Infants: Viewpoints From Seven European Countries. Acta Paediatr 102: E57-E63.
- Griffiths J, Weyers H, Adams M (2008) Chapter 6-Termination Of Life In Neonatology. In: Euthanasia And Law In Europe. Hart Publishing 217-255.
- Van De Riet JE, Vandenbussche FP, Le Cessie S, Keirse MJ (1999) Newborn Assessment And Long-Term Adverse Outcome: A Systematic Review. Am J Obstet Gynecol 180: 1024-1029.
- Wood NS, Costeloe K, Gibson AT, Hennessy EM, Marlow N, Et Al. (2003) The Epicure Study: Growth And Associated Problems In Children Born At 25 Weeks Of Gestational Age Or Less. Arch Dis Child Fetal Neonatal Ed 88: F492-500.
- Wood NS, Marlow N, Costeloe K, Gibson AT, Wilkinson AR (2000) Neurologic And Developmental Disability After Extremely Preterm Birth. Epicure Study Group. N Engl J Med 343: 378-384.
- Sharman M, Meert KL, Sarnaik AP (2005) What Influences Parents' Decisions To Limit Or Withdraw Life Support? Pediatr Crit Care Med 6: 513-518.
- Rebagliato M, Cuttini M, Broggin L, Berbik I, De Vonderweid U, Et Al. (2000) Neonatal End-Of-Life Decision Making: Physicians' Attitudes And Relationship With Self-Reported Practices In 10 European Countries. JAMA 284: 2451-2459.
- Meyer EC, Ritholz MD, Burns JP, Truog RD (2006) Improving The Quality Of End-Of-Life Care In The Pediatric Intensive Care Unit: Parents' Priorities And Recommendations. Pediatrics 117: 649-657.
- Wilkinson D (2006) Is It In The Best Interests Of An Intellectually Disabled Infant To Die? J Med Ethics 32: 454-459.
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 13971
- [From(publication date):
specialissue-2013 - Aug 29, 2025] - Breakdown by view type
- HTML page views : 9384
- PDF downloads : 4587