Research Article Open Access
Dentofacial Abnormalities and Oral Health Status in Children with Cerebral Palsy
Mohamed A Jaber1* and Taha Allouch2
1BDS, MSc, PhD, FDSRCS, FDSRCSE,FDSRCPS, Professor/ Department of Oral Surgery/Dubai College of Dental Medicine, United Arab Emirates
2DDS, Resident/College of Dentistry, Ajman University of Science & Technology, United Arab Emirates
- Corresponding Author:
- Dr Mohamed A Jaber
Professor, Oral Surgery Department
Dubai College of Dental Medicine, Dubai
P O Box 505097, United Arab Emirates
Tel: +971-04 4248630
Mobile: +971-050 5178
E-mail: mohamed.jaber@dcdm.ac.ae, mjaber4@hotmail.com
Received Date: November 18, 2014; Accepted Date: December 22, 2014; Published Date: December 26, 2014
Citation: Mohamed A Jaber, Taha Allouch (2015) Dentofacial Abnormalities and Oral Health Status in Children with Cerebral Palsy. J Interdiscipl Med Dent Sci 3:164. doi: 10.4172/2376-032X.1000164
Copyright: © 2015 Jaber MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at JBR Journal of Interdisciplinary Medicine and Dental Science
Abstract
Objectives: The aim of the study was to evaluate the oral health conditions and treatment need of children with Cerebral Palsy (CP) aged 4–17 years in United Arab Emirates (UAE) and provides baseline data to enable comparison and future planning of dental services.
Subjects and methods: The study included 52 patients with CP and 52 matched healthy control subjects. Each patient received a complete oral and periodontal examination using codes and criteria as described by WHO. Data analyzed using Fisher's exact test, Chi-square test and t-test.
Results: The prevalence of dental caries among children with CP was 90.0% (47/52) where as for the healthy controls was 54.0% (28/52). The overall means DMFT/dmft was 6.5. The restorative index (RI) and Met Need Index (MNI) for the CP children were 0.03 and 0.08 respectively. Children, 4-12 years old with CP had higher percentage of untreated caries, but lower percentage of filled teeth. The mean plaque index (2.35 ± 0.7); the probing depth (2.96 ± 0.8) and the average periodontal attachment loss 4.18 ± 1.3, all significantly greater in patients with CP than controls. And significantly high proportion of patients with CP (p<0.05) requiring complex periodontal treatment.
Conclusion: Results of this study indicate that the overall health of children with CP could be improved with earlier intervention and planned dental care.
Keywords
Cerebral palsy; Caries prevalence; Periodontal status; Treatment need
Introduction
Cerebral palsy (CP) is an umbrella term encompassing a group of non-progressive [1], motor [2], non-contagious conditions that cause physical disability in human development [3].
CP is caused by damage to the motor control centers of the developing brain and can occur during pregnancy, during childbirth or after birth up to about age three [2,4]. The incidence of CP is about 2 per 1000 live births. The incidence is higher in males than in females [5]. Variances in reported rates of incidence across different geographical areas are thought to be caused primarily by discrepancies in the criteria used for inclusion and exclusion. CP is classified according to the type of mobility alteration presented by the affected child: spastic, athetoid, ataxic and mixed. Spastic is the most common type of CP, accounting for nearly 80% of all CP cases. Children with this type of CP have one or more tight muscle groups which limit movement [6]. All forms of CP may have associated problems, such as mental retardation, strabismus, epilepsy or seizures, and disorders of vision or hearing. All these symptoms may complicate dental care for the affected children.
In the dental office, children with CP have difficulties in cooperating, due to their high sensitivity to physical contact and neuromotor response to unusual stimulus such as noise, artificial light and position at the dental chair [7].
Patients with disabilities appear to have poorer oral health compared with non-disabled counterparts, this is due to limited access to dental care, inadequate oral hygiene and disability-related factors [8-10]. Children with intellectual and developmental disabilities were significantly more likely to have delayed first dental visit, suggesting access problem [11]. Patients with CP present a reduced self-cleansing function of the oral cavity; due to account of drooling and abnormal movements of the tongue and facial muscles in addition their caregivers may have difficulties in complying with an appropriate oral hygiene [8-10]. Likewise patients with CP frequently suffer a reduced function of speech, mastication, and swallowing, which increases their risk of caries and rehabilitation process [8].
No specific oral pathology is associated with CP; the same diseases that affect the overall population can affect these children, although with a higher prevalence or severity due to their impaired motor skills [12]. In special cases, dental caries, gingival alterations, malocclusion, bruxism, dental erosion and enamel hypoplasia have been reported as more frequent or severe [12,13]. Dental management of patients with CP is challenging and requires special knowledge and skill, for example anesthesia, either local or general may require special facilities and care. Frassica and Miller reported that some anesthetic agents such as ketamine and enflurane have been found to induce seizures and are therefore contraindicated in CP [14]. Many studies have reported that dental care is the most common unmet health care need of disabled children [9-13,15].
In UAE there are limited data available relating to dental health of patients with CP, thus, we conducted this study to evaluate the oral health conditions, dental caries status and treatment need of children with CP aged 4–17 years in UAE and to establish various dentofacial changes in a group of patients with CP in UAE, and compared it with matched control individuals.
Material and Methods
Subjects’ selection
At the time of the study, there were 52 CP patients aged 4-17 years attending Sharjah School for Humanitarian Services (SSHS). This number represents all number of patients diagnosed with this syndrome and living at Emirates of Sharjah. The centers offer an intensive rehabilitation program for children diagnosed with CP. All the children had been previously examined and diagnosed medically as patients with CP according to the center’s medical records. Prior to the study (SSHS) was contacted and agreed to the protocol of the study.
Ethical clearance for the study was obtained from the Ethical Committee for Research of the College of Dentistry, Ajman University, UAE. Consent for examining of the children was obtained from the parents and SSHS head master.
The inclusion criteria involved were: diagnosis of CP, consent and age between 4 and 17 years. Exclusion criteria were: dental prophylaxes in the last 6 months, suffering from other diseases known to influence dental caries or the severity of periodontal diseases.
Fifty-two patients with CP were referred to our clinics for dental examination and met our inclusion criteria, therefore were included in the study.
Control selection
The healthy controls who met the above mentioned criteria were chosen from relatives or friends of patients with CP in an attempt to have matched age, sex, socioeconomic status and general dental care background. 52 healthy age and sex-matched controls (31 males and 21 females, mean age 9 + 1.1) were selected for the study. All controls were medically fit and none were undergoing antibiotic or anti-inflammatory therapy or had undergone such therapy in the previous 6 months. The controls were free from CP.
Examination
Following complete medical history, all subjects were examined according to the international criteria standardized by the World Health Organization [16] for oral health surveys. Patients were examined at the dental clinics of the College of Dentistry, Ajman University and an oral examination was conducted for both patients and controls.
World Health Organization (WHO) examination criteria dictate that only dental caries at cavitations level should be recorded. That is, it must be possible to confirm cavitations to dentine by placing a probe in the cavity. An overhead natural light, a mouth mirror and a ball tipped Community Periodontal Index (CPI) probe was used to remove plaque and to help confirm diagnosis of cavitations. A specially designed lightweight CPI probe with a 0.5-mm ball tip is used, with a black band between 3.5 and 5.5 mm and rings at 8.5 and 11.5 mm from the ball tip. Dental probes with blunt or rounded tips are used along with dental mirrors to confirm or reject dubious carious lesions into dentine by having a tactile feeling of softness at the base of the cavity or in some proximal wall of the carious tooth. Dental probes are also instrumental in removing any food debris that may mask the presence of a carious lesion on the tooth surface.
A single examiner who was trained and calibrated for the study examined all children. Teeth were examined in a clockwise direction, taking a start from the last tooth in the right upper quadrant of the oral cavity and ending with the last one in the right lower quadrant. The mesial surface of every tooth was examined first followed by occlusal/incisal, distal, labial/buccal and finally lingual/palatal.
DMFT/dmft index and criteria for detection of dental caries
The DMFT index for permanent and dmft index for deciduous teeth were used to record dental caries in both types of dentitions. The various codes which were entered into the boxes of a specially designed recording form included: tooth with no decay (N), decayed tooth (D/d), filled tooth (F/f), tooth missing because of caries (M), tooth missing because of any other reason (O), broken tooth (B), crowned tooth (C) and excluded tooth (E). A filled tooth having a carious lesion, irrespective of whether the lesion was in physical association with the filling or not, was included in the category of 'decayed tooth'. In primary and mixed dentitions, missing deciduous teeth were not recorded.
Met Need Index (MNI), an indication of treatment received by an individual is determined using the ratio of the mean missing (M) plus filled (F) teeth to mean decayed, missing and filled teeth (DMF) that is M+F/DMF. While Restorative Index (RI) that describes the restorative care of those who have suffered the disease is measured by the ratio of filled (F) to filled plus decayed teeth (F+D) percent that is F/F+D percent [17]. This methodology was used systematically for all CP and healthy control children examined.
Periodontal and gingival health status was recorded according to the Community Periodontal Index of Treatment Needs CPITN as recommended by Ainamo et al. [18].
The highest reading in a sextant was recorded. Three indicators of periodontal status were used for the assessment: 1) presence or absence of gingival bleeding, 2) supra-and sub-gingival calculus, 3) periodontal pockets-subdivided into 4-5 mm and > 6 mm. As the majority of the subjects were under the age of 20 years, only six index teeth - 16, 11, 26, 36, 31 and 46 - were examined to avoid scoring the deepened sulci associated with eruption as periodontal pockets. When children under the age of 15 were examined, pockets were not recorded; only bleeding and calculus were considered. Calibration of the investigator for CPITN was carried and the Kappa value was 0.87. Oral hygiene was evaluated by examining the dental plaque present on the lingual and buccal surfaces of the six index teeth, using the criteria of the plaque index of Silness and Loe [19].
Malocclusion was identified in accordance with WHO criteria [20] and was recorded as: no malocclusion=0, slight malocclusion=1, and severe malocclusion=2. Two levels of anomaly were registered: slight malocclusion - such as one or more rotated or twisted teeth, crowding or spacing and severe malocclusion - anomalies that cause an unacceptable effect on facial appearance, significant reduction in masticatory function, impairment of speech, or one or more of the following conditions of the four anterior incisors: maxillary overjet 9 mm, mandibular overjet one full tooth depth, open bite, midline shift 4 mm, crowding or spacing 4 mm.
Data analysis
The data were summarized and described using relative frequencies and percentages for categorical variables (such as the presence of decayed teeth) and means for the interval scaled variables (such as the DMFT/dmft score). When the outcome variables were categorical, chi-squared and t-test was used to examine differences by gender, and age group for statistical significance. Data were analyzed using SPSS software, version 12•0 (SPSS Inc., Chicago, IL, USA) for Windows. Statistical significance was set at P < 0•05.
Results
Prevalence
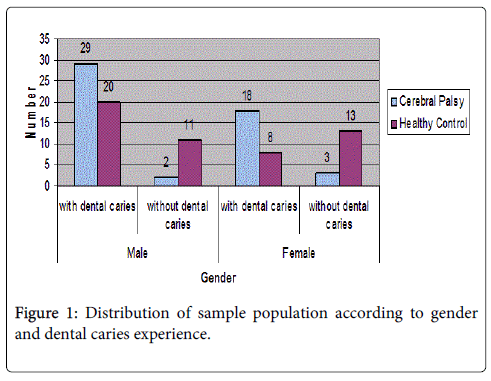
Fifty-two healthy patients were compared with the 52 CP patients. Patients with CP (cases) and the control group were recruited from the same population. The age range of the study group was 4-17 years (mean, 9 ± 1.07); there were 31 males (60%) and 21 females (40%). The control group consisted of 52 healthy non- institutionalized children (31 males and 21 females, mean age 9+ 1.1) were selected for the study. The overall prevalence of dental caries among children with CP was 90.0% (47/52) where as for the healthy controls was 54.0% (28/52) (Figure 1).
Mean DMFT/dmft values
The mean DMF index in patients with CP of 6.5 was significantly greater than in controls (Table 1). In this group of children and adolescents with CP, the caries prevalence in relation to age group and type of dentition is detailed in (Table 2). There is high dmft score among the 8-12 years old children with CP while in the permanent dentition the highest score was among the 13 to 17 years age group. As for the treatment (filling) of the carious teeth, more treatment had been performed in the permanent dentition than in the primary teeth. Significant number of children with caries in the primary dentition had had no dental treatment at all; a significantly higher proportion than the corresponding figure for patients with caries in the permanent dentition.
| Cerebral Palsy n= 52 (mean +-s.d.) |
Control n=52 (mean +-s.d.) |
P value* | |
|---|---|---|---|
| DMF index | 6.5 ± 0.84 | 5.0 ± 3.15 | 0.021 |
| Carious teeth | 6.0 ± 0.61 | 3.0 ± 2.90 | 0.001 |
| Missing teeth | 0.3 ± 1.65 | 0.3 ± 1.64 | 0.17 |
| Filled teeth | 0.2 ± 2.02 | 1.71 ± 2.44 | 0.03 |
Table 1: Dental caries experience of patients with CP and control subjects. (*P value for t-test)
| Primary dentition | Age group | |||
| 4–7years old (n=10) | 8–12years old (n=12) | |||
| Decayed teeth | 0.3 | 1.1 | ||
| Missing teeth | 0.1 | 0.1 | ||
| Filled teeth | 0.0 | 0.0 | ||
| dmft index | 0.4 | 1.2 | ||
| Permanent dentition | Age group | |||
| 4–7years old (n=10) | 8–12years old (n=12) | 13–17years old (n=8) | ||
| Decayed teeth | 1.3 | 1.5 | 1.8 | |
| Missing teeth | 0.0 | 0.0 | 0.1 | |
| Filled teeth | 0.0 | 0.1 | 0.1 | |
| DMFT index | 1.3 | 1.6 | 2.0 | |
Table 2: Proportion of patients free of caries, and dmft and DMFT averages among children and adolescents with CP, by age groups and type of dentition.
Met Need Index (MNI) and Restorative Index (RI)
The treatment received and restorative care of children with CP who have suffered the disease is presented in (Table 3). The RI for the patients with CP was 0.03 and MNI was 0.08. For the healthy control group RI of 0.3 was found and MNI was 0.4.
| Group | No | D | M | F | DMFT/dmft | Mean DMFT/dmft | RI | MNI |
|---|---|---|---|---|---|---|---|---|
| CP | 47 | 281 | 16 | 11 | 308 | 6.5 | 0.03 | 0.08 |
| Control | 28 | 84 | 9 | 48 | 141 | 5.0 | 0.3 | 0.4 |
| Total | 75 | 365 | 25 | 59 | 449 | 6.0 | 0.13 | 0.18 |
Table 3: Mean DMFT/dmft, Restorative Index (RI) and Met Need Index (MNI) for the two groups. (RI) Restorative Index =F/F+D, (MNI) Met Need Index =M+F/DMF
Periodontal status and treatment need
In children with CP, the mean plaque index was 2.35 ± 0.7; the probing depth 2.96 ± 0.8, and the average periodontal attachment loss was 4.18 ± 1.3, all significantly greater than controls (Table 4). The assessment of the periodontal treatment needs of the children with CP revealed that only 10.0% of the children had healthy gingiva compared with 36.5% among the healthy controls (Table 5). And significantly high proportion of patients with CP (p<0.05) requiring complex periodontal treatment.
| Cerebral Palsy n= 52 (mean +-s.d.) | Control n=52 (mean +-s.d.) | t | P value | |
|---|---|---|---|---|
| Plaque index | 2.35±0.77 | 1.06±0.63 | 4.68 | 0.03* |
| Probing depth | 2.96±0.82 | 2.01±0.57 | 5.65 | 0.04* |
| Attachment loss | 4.18±1.26 | 3.21±0.82 | 5.59 | 0.03* |
Table 4: Periodontal health in cerebral palsy patients and control groups. [*Significant]
| CPITN | Cerebral Palsy n= 52 no % | Control n=52 no % | P value | ||
|---|---|---|---|---|---|
| Healthy gingival (code 0) | 5 | 10.0 | 19 | 36.5 | 0.01* |
| Bleeding on gentle probing (code 1) | 6 | 11.5 | 13 | 25.0 | 0.13 |
| Calculus during probing (code 2) | 13 | 25.0 | 11 | 21.1 | 0.71 |
| Pocket depth 4-5mm (code 3) | 13 | 25.0 | 4 | 7.6 | 0.04* |
| Pocket depth 6mm or more (code 4) | 15 | 28.8 | 5 | 9.6 | 0.04* |
| Total | 52 | 52 | |||
Table 5: Periodontal treatment needs status of the subjects. [*Significant]
Dentofacial abnormalities
CP patients have shown significantly higher proportion of malocclusion and high arch palate (p<0.01), compared with non CP subjects. The prevalence of other dentofacial abnormalities revealed amongst patients with CP is presented in (Table 6). Of note however, palpable lymph nodes is a significant findings among patients with CP.
| Abnormalities | Cerebral Palsy No n= 52% | Control No n=52% | P value |
|---|---|---|---|
| Fissure tongue | 13 (25.0) | 11 (21.0) | 0.71 |
| High arched palate | 34 (65.3) | 7 (13.4) | 0.021* |
| Malocclusion | 44 (85.0) | 5 (9.6) | 0.002* |
| Microdontia | 13 (25.0) | 1 (2.0) | 0.001* |
| Fractured maxillary teeth | 16 (31.0) | 1 (2.0) | 0.001* |
| Hypertelorism | 7 (13.4) | 1 (2.0) | 0.04* |
| Delayed eruption | 11 (21.1) | 2 (3.8) | 0.01* |
| Lymphadenopathy | 30 (61.5) | 5 (9.6) | 0.0031* |
Table 6: Dentofacial abnormalities amongst cerebral palsy individuals. [*Significant]
Discussion
It is difficult to estimate the percentages of CP in the UAE since there is no central data collection agency. Evidence would suggest that the percentage of people with disabilities in the UAE is similar to the worldwide average, i.e. 8-10 percent of the population [21].
The studied group showed more males than females, with a ratio of 1.4:1, this might reflect the higher prevalence of CP in males as it was reported in other part of the world [5,8,10].
People with CP experience a somewhat higher degree of dental decay, primarily due to poor oral hygiene. This poor oral hygiene is the direct result of the inability of many with CP to physically cope with brushing and flossing activities [8-10].
In this study the overall prevalence of dental caries among the children with CP was 90.0%. The high dental caries prevalence among children with CP confirms the findings of previous observations [9,10] and the proportion of children suffering from CP with caries that never received dental restorative treatment was higher in younger children with a primary dentition than in older children with a permanent dentition, thus agreeing with previous findings suggesting that the severity of caries attack is essentially higher in CP than normal children but that the rate of treatment is frequently lower in the CP group, this emphasizes the fact that children with CP are receiving less dental care than their normal counter-parts.
When the individual components of the mean DMF values were examined, disparities were apparent when children with CP were compared to normal children, The trends in this study are similar to those found in other studies, and the results are of clinical importance. The most important differences were found in the mean numbers of filled teeth. Children with CP had considerably fewer filled teeth than normal children and significant number of children with caries in the primary dentition had had no dental treatment at all; a significantly higher proportion than the corresponding figure for patients with caries in the permanent dentition. This observation warrants further study; this is may be a consequence of the practical difficulties in providing dental care for severely affected children.
In the present investigation the decayed index was much higher than the missing and filled indices in both dentitions and needed some kind of dental treatment. The percentage of the dmft score represented by untreated decay in 4 - 12 year-olds was higher in children with CP than the normal children. The average number of missing (M) teeth was similar in both groups, except in the older children where children with CP had on average more missing teeth than normal healthy controls. This difference could be explained by the inability of these patients to follow home care regimens. It has also been shown that the parents of disabled children often become pre-occupied with the medical and social problems they have to face and disregard the need for dental care.
An analysis of caries prevalence of children living in Emirate of Sharjah, UAE showed that a low level of restorative dental treatment in the primary dentition [22]. The lower provision of restorative dental treatment for children with primary dentition is widespread and has been attributed to cultural factors involving both dental caregivers and parents. A dental survey in the UAE found the prevalence of dental caries among 5-6 years old healthy school children was high 76.1% and the average dmfs score was 10.2 [23]. This is in contrast to other study which reported mean deciduous caries experience to be 0.9 for 4 to 5 years old and the mean permanent caries experience (DMFT) for 12-17 years old was 2.0 [24]. The mean dmfs/DMFS values were 2.5 and 3.4 respectively.
In this study the caries indices in primary and permanent dentition increased markedly with age in patients with CP. This is in agreement with several previous studies in different countries [25-27].
Met Need Index (MNI) which is an indication of treatment received by an individual and Restorative Index (RI) which reflects the restorative care of those who have suffered the disease [17] among the studied children with CP were low compared with healthy control subjects. These results indicate that the preventive and restorative treatment needs of many children with CP in the present study were unsatisfactory, as only 23.0% (11/47) of them received restorative treatment compared with healthy control patients. Possible contributory factors may include insufficient trained dental practitioners to deal with patients with disabilities, and the complex treatment needs requiring special care or general anesthesia [28].
Periodontal disease and oral hygiene represent a significant problem for the handicapped children. The findings from this study showed a high level of gingivitis and periodontal disease in this age group of children with CP compared with the control group, and this could well explain the gingivitis and recession, probably a consequence of poor oral hygiene because of manual dexterity, masticatory defects, gingival sensitivity problems and altered tongue and masticatory muscles.
The percentage of patients with periodontal problems is 90.0 percent and only 10.0 percent were having healthy gingiva. Also a significant percentage of these children had pockets and will need complex periodontal care. This is contrary to the findings of other studies [29,30] for this age group in normal children. These investigators found negligible severe or destructive periodontitis in their studies. Kumar and Sharma [31] associated medical diagnosis, IQ level, parent level of education and economic status as elements that apparently contributed to impairment of periodontal health and to increased treatment needs among handicapped children. These factors could not be assessed on the children in the present study due to their very low number.
Using a different periodontal index Brown [32] found poor periodontal health of handicapped children and he equated this to their lack of adequate oral hygiene measures and consequently abundant calculus formation.
With the majority of children in this study needing scaling, polishing and oral hygiene instructions there is an increasing need for comprehensive preventive dental program to promote better oral hygiene and prevent the development and progression of periodontal diseases since the hallmark of management of these children is prevention.
Mentally and physically handicapped children may present with Oral and dental anomalies that affect the function of stomatognathic complex. In present study, most of the individuals with CP had high arched palate (65.3%) and malocclusion (85.0%) these results are consistent with the findings of other studies [33,34]. But in contrast to the reports of other studies [35,36] which showed 37.0% and 60.0% malocclusion in mentally retarded children, respectively. The primary cause of malocclusion may be disharmonious relation between intra oral and peri-oral movements [37].
Other reported problems among children with CP include drooling or sialorrhea. This may occur as a result of hypersecretion of saliva, inability to recognize salivary spill, and dental malocclusion. Dehydration, dental enamel erosion, and odor can occur as a result, as well as social stigmatization, which can be significant for both the family and the child [38,39].
In conclusion, the findings of this study revealed that the rate of caries, periodontal disease and malocclusion in children with CP exceeds that of children without disabilities. Preventive, restorative and periodontal treatment needs are unmet in children with CP.
Acknowledgment
I would like to thank The Sharjah City for Humanitarian Services, children and their parents for giving us access to conduct this study. Also like to acknowledge the help and contribution of the other doctors and assisting staff.
References
- Krägeloh-Mann I, Cans C (2009) Cerebral palsy update. Brain Dev 31: 537-544.
- Jan MM1 (2006) Cerebral palsy: comprehensive review and update. Ann Saudi Med 26: 123-132.
- Beukelman D, Mirenda R (1999) Augmentative and Alternative Communication: Management of severe communication disorders in children and adults. 2nd edn. Paul H Brookes Publishing Co. Baltimore, USA. 246–249.
- Thorngren-Jerneck K, Herbst A (2006) Perinatal factors associated with cerebral palsy in children born in Sweden. ObstetGynecol 108: 1499-1505.
- Johnson A (2002) Prevalence and characteristics of children with cerebral palsy in Europe. Dev Med Child Neurol 44: 633-640.
- Bax M, Goldstein M, Rosenbaum P, Leviton A, Paneth N, et al. (2005) Proposed definition and classification of cerebral palsy, April 2005. Dev Med Child Neurol 47: 571-576.
- Weddell JA, Vash BW, Jones EJ, Lynch TR (2000) Dental problems of children with disabilities. In: McDonald RE, Avery DR, Dean JA (eds) Dentistry for the Child and Adolescent, 8th edn. MO: Mosby, St. Louis, USA. p628–634.
- Jones MW, Morgan E, Shelton JE (2007) Primary care of the child with cerebral palsy: a review of systems (part II). J Pediatr Health Care 21: 226-237.
- GuaréRde O, Ciamponi AL (2003) Dental caries prevalence in the primary dentition of cerebral-palsied children. J ClinPediatr Dent 27: 287-292.
- Rodrigues dos Santos MT, Masiero D, Novo NF, Simionato MR (2003) Oral conditions in children with cerebral palsy. J Dent Child (Chic) 70: 40-46.
- Chi DL, Momany ET, Jones MP, Damiano PC (2011) Timing of first dental visits for newly Medicaid-enrolled children with an intellectual or developmental disability in Iowa, 2005-2007. Am J Public Health 101: 922-929.
- Chu CH, Lo EC (2010) Oral health status of Chinese teenagers with cerebral palsy. Community Dent Health 27: 222-226.
- Alhammad NS, Wyne AH (2010) Caries experience and oral hygiene status of cerebral palsy children in Riyadh. Odontostomatol Trop 33: 5-9.
- Frassica JJ, Miller EC (1989) Anesthesia management in pediatric and special needs patients undergoing dental and oral surgery. IntAnesthesiolClin 27: 109-115.
- Nelson LP, Getzin A, Graham D, Zhou J, Wagle EM, et al. (2011) Unmet dental needs and barriers to care for children with significant special health care needs. Pediatr Dent 33: 29-36.
- Joharji RM, Adenubi JO (2001) Prevention of pit and fissure caries using an antimicrobial varnish: 9 month clinical evaluation. J Dent 29: 247-254.
- Jackson D (1973) Measuring restorative dental care in communities. Br Dent J 134: 385-388.
- Ainamo J, Barmes D, Beagrie G, Cutress T, Martin J, et al. (1982) Development of the World Health Organization (WHO) community periodontal index of treatment needs (CPITN). Int Dent J 32: 281-291.
- SILNESS J, LOE H (1964) PERIODONTAL DISEASE IN PREGNANCY. II. CORRELATION BETWEEN ORAL HYGIENE AND PERIODONTAL CONDTION. ActaOdontolScand 22: 121-135.
- World Health Organization (1987) Oral Health Surveys: Basic Methods, 3rd edn. World Health Organization. Geneva, Switzerland.
- Bradshaw K, Tennant L, Lydiatt S (2004) Special Education in the United Arab Emirates: Anxieties, Attitudes and Aspirations. Int J of Spec Educ 19: 49-55.
- Pine CM, Adair PM, Burnside G, Nicoll AD, Gillett A, et al. (2004) Barriers to the treatment of childhood caries perceived by dentists working in different countries. Community Dent Health 21: 112-120.
- Hashim R, Thomson WM, Ayers KM, Lewsey JD, Awad M (2006) Dental caries experience and use of dental services among preschool children in Ajman, UAE. Int J Paediatr Dent 16: 257-262.
- Nunn JH, Gordon PH, Carmichael CL (1993) Dental disease and current treatment needs in a group of physically handicapped children. Community Dent Health 10: 389-396.
- Alavi AA, Amirhakimi E, Karami B (2006) The prevalence of dental caries in 5 - 18-year-old insulin-dependent diabetics of Fars Province, southern Iran. Arch Iran Med 9: 254-260.
- Altun C, Guven G, Akgun OM, Akkurt MD, Basak F, et al. (2010) Oral health status of disabled individuals attending special schools. Eur J Dent 4: 361-366.
- Santos MT, Biancardi M, Guare RO, Jardim JR (2010) Caries prevalence in patients with cerebral palsy and the burden of caring for them. Spec Care Dentist 30: 206-210.
- Curzon ME, Toumba KJ (1998) The case for secondary and tertiary care by specialist dental services. Community Dent Health 15 Suppl 1: 312-315.
- Ainamo J, Sarkki L, Kuhalampi ML, Palolampi L, Piirto O (1984) The frequency of periodontal extractions in Finland. Community Dent Health 1: 165-172.
- Hargreaves JA, Thompson GW, Lizaire AL, Finnigan PD (1989) The periodontal status of 13-year-old children in western Canada using the CPITN index. Community Dent Health 6: 391-396.
- Kumar S, Sharma J, Duraiswamy P, Kulkarni S (2009) Determinants for oral hygiene and periodontal status among mentally disabled children and adolescents. J Indian SocPedodPrev Dent 27: 151-157.
- Brown JP (1980) The efficacy and economy of comprehensive dental care for handicapped children. Int Dent J 30: 14-27.
- Guerreiro PO, GarciasGde L (2009) [Oral health conditions diagnostic in cerebral palsy individuals of Pelotas, Rio Grande do Sul State, Brazil]. CienSaude Colet 14: 1939-1946.
- Oliveira AC, Paiva SM, Martins MT, Torres CS, Pordeus IA (2011) Prevalence and determinant factors of malocclusion in children with special needs. Eur J Orthod 33: 413-418.
- Ashok P, Boghani CP (1985) Dental manifestations of Down's syndrome. J Indian Dent Assoc 57: 97-99.
- Tandon P, Jha S, Tandon R, Sondhi D, Chandra M, et al. (1990) Oro-dental pattern in mentally retarded. Indian J Psychiatry 32: 185-187.
- Miamoto CB, Ramos-Jorge ML, Pereira LJ, Paiva SM, Pordeus IA, et al. (2010) Severity of malocclusion in patients with cerebral palsy: determinant factors. Am J OrthodDentofacialOrthop 138: 394.
- Hockstein NG, Samadi DS, Gendron K, Handler SD (2004) Sialorrhea: a management challenge. Am Fam Physician 69: 2628-2634.
- Lin X, Wu W, Zhang C, Lo EC, Chu CH, et al. (2011) Prevalence and distribution of developmental enamel defects in children with cerebral palsy in Beijing, China. Int J Paediatr Dent 21: 23-28.
Relevant Topics
- Cementogenesis
- Coronal Fractures
- Dental Debonding
- Dental Fear
- Dental Implant
- Dental Malocclusion
- Dental Pulp Capping
- Dental Radiography
- Dental Science
- Dental Surgery
- Dental Trauma
- Dentistry
- Emergency Dental Care
- Forensic Dentistry
- Laser Dentistry
- Leukoplakia
- Occlusion
- Oral Cancer
- Oral Precancer
- Osseointegration
- Pulpotomy
- Tooth Replantation
Recommended Journals
Article Tools
Article Usage
- Total views: 15526
- [From(publication date):
February-2015 - Aug 30, 2025] - Breakdown by view type
- HTML page views : 10726
- PDF downloads : 4800