Research Article Open Access
Diagnosing Levels of Distress in Specialist Palliative Care
Ana Draper* and Becky HermanConsultant Systemic Psychotherapist, Hertfordshire Community NHS Trust, Palliative and End of Life Care Network, UK
- Corresponding Author:
- Ana Draper
Consultant Systemic Psychotherapist
Hertfordshire Community NHS Trust
Palliative and End of Life Care Network, Apsley One
Brindle Way, Hemel Hempstead, HP3 9BF, UK
Tel: 07808934406
E-mail: Ana.Draper@hchs.nhs.uk
Received Date: March 09, 2015; Accepted Date: May 14, 2015; Published Date: May 18, 2015
Citation: Draper A, Herman B (2015) Diagnosing Levels of Distress in Specialist Palliative Care. J Palliat Care Med 5:220. doi:10.4172/2165-7386.1000220
Copyright: © 2015 Draper A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Visit for more related articles at Journal of Palliative Care & Medicine
Abstract
This paper makes the case for the use of the Distress Thermometer (DT) as a standardised diagnostic tool in End of Life Care. It explores the current situation in palliative care health services, building an argument that there is an under-diagnosis of depression and mental distress in the fields of palliative care due to a lack of standardisation and screening. The paper sets out its hypothesis and follows this with an account of repeat audit cycles and action research interventions in the implementation and use of the DT within a National Health Service and voluntary sector context.
Keywords
End of life care; Palliative care; Distress thermometer
Introduction
The field of palliative care continues to grow at an expeditious rate, as do the plethora of holistic, spiritual, and psychological services that comprise it. Each year in the United Kingdom approximately a quarter of a million people are cared for by the National Health Service (NHS) in addition to voluntary services. Caring may occur in both home-based and in-patient settings [1]. One favoured setting for patients to receive palliative care is in the comfort and privacy of their own home by a team of highly specialized, multi-disciplinary health care professionals [2].
As palliative care services swiftly expand to meet the increasing demands of society with its ageing population and the advances in medicine that prolong life, so does the need for the development and use of practical, accurate, and standardised assessment tools. We would assert that one of the most complex challenges facing health care professionals working in palliative care is the identification and implementation of best-practice methods in the diagnosis of depression in their patients. Depression is the most studied mental health disorder in palliative care [3]. However, no consensus exists on precisely which of the 106 identified tools designed to diagnosis depression should be implemented [3]. Without clearly identified means for best practice it is left to the individual health care professional to sift through the available literature which contains a high concentration of polarising contradictions. Recommendations in the literature are often not approved for patients receiving palliative care, or are limited to studies undertaken in specific care settings that are not applicable to a broader spectrum of care environments. When best-practice methods are not implemented in daily routines, it results in lowering the quality and efficacy of the care being given to patients.
Depression in palliative care
To effectively lessen the uncertainty and variability surrounding depression in palliative care, strides towards clarification and standardisation are necessary wherever possible. At the heart of the confusion lies the ambiguity in the term “depression” itself. As The National Institute of Health defines it, ‘True clinical depression is a mood disorder in which feelings of sadness, loss, anger, or frustration interfere with everyday life for weeks or longer’,What is Depression? NIMH [4]. Comparatively, the American Psychiatric Association states that a depressive episode may be occurring when symptoms are present for two continual weeks or more [5]. Aside from its clinical context, “depression” may be used synonymously with terms like “low mood”, “distress”, or to describe varying degrees of sadness. In the context of palliative care some of the characteristics of depression are likely to be present and yet not signify clinical depression.
To further complicate matters, patients enrolled in palliative care services are likely to be experiencing a vast array of both chronic and acute physical symptoms which can mask or result in false positives in the diagnosis of depression. The highest prevalence of diagnosed depression and the lowest levels of physical health are presented in patients with late-stage cancer [6].
This makes it difficult to incorporate classically used assessment tools. For example, four of the nine DSM-IV criteria [5] required for a diagnosis of clinical depression are somatically-based. The criteria also explicitly states, “Do not include symptoms that are clearly due to a general medical condition” [5]. In order to avoid a somatic cross-over of signs of depression, Endicott [7] as well as Noorani and Montagnini [8] among others have recommended the removal of somatic-based signs for diagnosis. In their place, Endicott [7] suggests the substitution of typical somatic diagnostic criteria with the following observable signs including, “Tearfulness, depressed appearance, social withdrawal, brooding, and lessened talkativeness”. By focusing not only on the somatic experience of the patient but also the emotional, accuracy of diagnosis may be improved.
Above all, undiagnosed depression has the potential to not only affect the psychological and physical well-being of the patient, but their careers as well. With regards to the predictive relationship between depressed mood and quality of life (QOL), QOL has been identified to be a stronger association than that of the presence of fatigue [9]. Depression has also been found to have the ability to exacerbate pain and other physical symptoms, which may limit the patient’s ability to emotionally connect and interact with family members [10]. It also dramatically increases the risk of suicide and hastened death [11].
When a patient experiences depression, the likelihood their partner will also face emotional challenges significantly rises [9]. Emotional disconnectedness with family members and acquaintances has the potential to lessen the occurrence of a “good death”, a term applied by health care professionals that describes the incorporation of a “positive coping strategy and acceptance on the part of the patient” [2]. Therapeutic work with people near the end of their lives is uniquely challenging, in that the outcome is unchanging. Kellehear [12] asserts that for the patient, a “good death” may include feeling they are psychologically equipped for death with control in how the death occurs and a voice that informs the multidisciplinary team to create a bespoke care package. Therapists are faced with upholding the emotional components surrounding a “good death” by maintaining and improving familial connectedness.
Connectedness is often explored through therapeutic dialogues focusing on the hope that is immediately present, rather than placing emphasis in the future. Hope is essential to the psychological well-being of the patient, as it allows the patient to maintain a higher amount of autonomy and control over the dying process through the incorporation of advanced care planning. To increase the likelihood of a “good death” occurring, crucial steps must be taken. Health care professionals can help increase the likelihood of a good death occurring, by ensuring the use of evaluated best practice methods when assessing a patient’s mental health. What follows is an account of the effective use of the DT within a sample group in the Hertfordshire Palliative Care Services. This research took place between July 2011 and March 2013.
Methodology
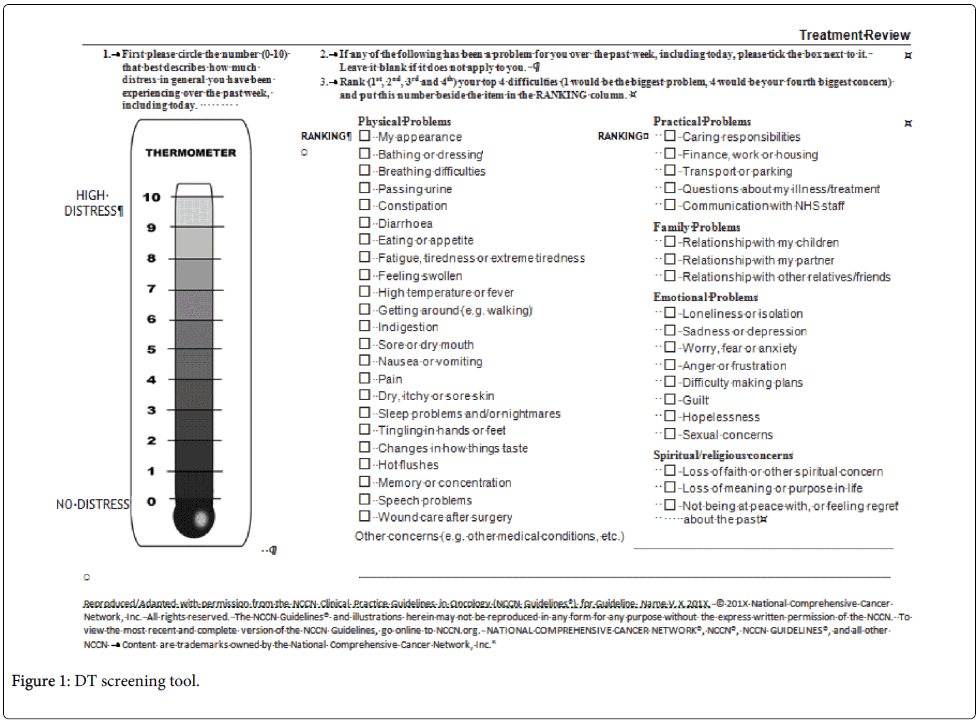
The DT used in our pilot study is attached to this paper. The DT is the only validated tool for use in oncology and end of life care due to the complexity associated with this patient group and great deal of research has explored the use of the DT in oncology and end of life care. It has been trialled in an array of clinical setting including primary care, across a broad population of differing patient groups and has shown a high level of sensitivity which is comparable to other screening tools Peryiakoil and Hallenbeck [13], Mitchel [14], Gesller et al. [15], Roth et al. [16], Zwahlen et al. [17] and Wasteson et al. [3].
Our research was conducted in several planned stages, and our actions investigated through the implementation of an audit cycle. In observing the effect of our actions at each stage of the cycle, we were building a scaffolding of knowledge which allowed us to continuously incorporate findings into subsequent stages of the investigation.
Planned cycles
The planned action research [18] cycles from which we acted and fond understanding were as follows:
Audit looking at current practice within the service and literature review.
Review of findings and actions agreed for future investigation.
2nd audit looking at the result of our actions,
Review of findings and actions agreed for future investigation.
3rd audit looking at the result of our actions,
Review of findings and actions agreed for future investigation.
4th audit looking at the result of our actions,
Review of findings and actions agreed for future investigation.
1) Audit looking at current practice within the service and literature review.
In order to identify and incorporate the best methods for assessing distress in a community palliative care setting, a two part audit was initially conducted. An audit involves comparing current practices of an institution with those most empirically and professionally supported to ensure the presence of evidence-based practice [19]. Audits are used frequently in health care as a method of clinical governance to improve current practices and ensure the highest level of care quality, “Healthcare Improvement Scotland” [19]. With such low levels of standardisation available empirically, it was predicted that the clinical practices of the specialist palliative care team would mirror the inconsistencies present in the existing literature. Therefore, the hypothesis was that depression occurring within patients receiving palliative care in the community will be under diagnosed.
The first audit conducted consisted of two phases, and occurred between April and August 2011. The first phase was a systematically-based literature review used to identify available assessment tools, and establish evidence-based methods for evaluating mood in a population receiving specialist palliative care. During the second phase, a retrospective case note review was carried out, containing a stratified selection of case notes maintained by a specialist palliative nursing team.
Potential psychometric tools were screened through the incorporation of a systematic literature review. This consisted of empirical articles being screened for relevance, quality, and the use of strict inclusion and exclusion criteria. Terms incorporated into the literature search were as follows: depression/low mood, palliative care/end of life care/terminal care, quality of life, and assessment.
PubMed and Psych Info databases were searched up to the 1 July 2011. No starting year limit was deemed necessary due to the high level of specificity of the terms included in the search. Grey literature and primary data were not collected and no ethical implications were present in the search process. The medical subject heading known as “MeSh” terms were permitted in the searches. MeSh draws from a 25,000-word vocabulary to expand searches by including synonyms for keywords. MeSh terms were allowed in order to ensure the search was comprehensive in nature. The Critical Appraisal Skills Programme (CASP) [20] was consulted to analyse the quality of articles.
After eliminating repeated papers and those that were irrelevant or of inadequate quality, 23 of the original 253 were selected for a comprehensive review. Within the 23 studies selected, 11 were designed to assess depression and 12 for QOL. After careful analysis, three tools were selected as being the strongest based upon empirical support for evidence-based practice methods, strength of the studies, and sensitivity to a community and palliative care setting. The tools selected to create a coding system in order to analyse the case notes were the WHOQOL-100 (The World Health Organisation), the Brief Edinburgh Depression Scale [21], and the DSM-IV criteria for depression, with the removal of somatic symptoms [5,13].
The second phase of the audit consisted of case notes which were analysed to determine how depression was being assessed and recorded by the nurses. The sample consisted of twenty patients, representing 10% of the registered patients in that time frame. Case notes were stratified by age, gender, and diagnosis. Based upon the results of the literature review, content analysis of the case notes was applied using a coding scheme developed from the psychometric tools identified as being empirically-supported, as well as most fitting and applicable for palliative patients in a community setting.
The instruments incorporated in the examination of case notes were the WHOQOL-100 [22], the Brief Edinburgh Depression Scale [21], and the DSM-IV [5] diagnostic criteria with the removal of somatic signs. The three instruments were coalesced to create two individual coding schemes. The first was used to determine which factors of quality of life were most commonly affected in the sample, and how often psychological mood was recorded by the specialist nurses. It emphasized the 24 facets of quality of life identified in the WHOQOL-100 [22].
A second coding scheme was also created to enable occurrences of depression and mood disturbances to be derived from the data. Two pre-existing instruments for the diagnosis of depression were culled. It incorporated the DSM-IV [5] criteria for depression with removal of any somatic criteria, and replaced with cognitive and observable signs of depression [8]. Question-derived content from the Brief Edinburgh Depression Scale [21] was gathered to evaluate the depression on an immediate basis. Some of the criteria between the two tools overlapped, and repetitive content was eliminated. Direct content analysis was then carried out to assess the data.
2) Review of findings and actions agreed for future investigation.
The findings were reviewed and the next step of action agreed with the whole clinical team. The action being the use of a measurement tool to identify distress.
3) 2nd audit looking at the result of our actions
The additional steps were taken forward as Actions towards on-going knowledge and subsequent audit cycles:
(4-8) In seeking to increase standardisation and accuracy in assessing psychological distress within patients being managed by the specialist palliative care team, a further audit cycle was conducted. Building upon the findings of the initial audit, an opportunity was identified to implement greater use of evidence-based practice methods in the assessment of psychological well-being of the patients.
The audit consisted of three additional phases, prompted by the findings from the initial study which evaluated the assessment process to identify depression in patients receiving palliative care. The study implemented the use of the Distress Thermometer (DT) which is a validated and recognised tool to assess for distress with patients and family members in palliative care [14-17] The DT used was established by the National Comprehensive Network Guidelines® [23], for use with cancer patients.
The DT was also validated for use by the psychology group at the Mount Vernon Cancer Network [24], and therefore the tool of choice in respect to distress screening were the specialist palliative care service is based. In 2006, the MVCN published the “Framework for the Assessment and Management of the Psychological Well-Being of Adults with a Cancer or Palliative Diagnosis” [24] which was drawn from NICE Guidance.
It sought to improve care by providing means for evidence-based practice to occur. Mitchell [14] found that ultra-short methods as a screening process are best at ruling out depression, anxiety or distress with an accuracy of 85-95%. Mitchell et al. [14] also found that clinicians prefer distress management measurement tools and that only a third of cancer clinicians would be prepared to use identifying instruments in routine care.
Participants
All new referrals in a given time period were initially eligible as participants in the audit. At the time the second cycle of the audit was conducted, there were 137 new referrals. Twenty-three DT were completed, despite the fact that all new referrals were in the inclusion criteria. The inclusion criteria also consisted of the patient’s cognitive ability to complete a DT, and willingness to answer questions on the DT as part of their care plan. Exclusion from participation in the audit was based upon mental and psychical capacity, such as dementia and physical symptoms at the end of life.
Ethical considerations
According to NHS Governance policies, all individuals pre-consent to their information being used for potential research when registering with the NHS (NHS Department of Health, 2011). The NHS upholds strict standards in data management that ensure patient anonymity is guarded and maintained.
These standards were upheld by the team members collecting and processing the data, by use of data encryption and exclusion of individual identifiable details. The goal of the audit centres on improvement in assessment and appropriate referral, rather than the individual health information of the patient. Therefore, Information was analysed en masse, and not on an individual case-by-case basis. The gathered data did not give information about the patient or their locality and the patient was not identifiable to the clinician analysing the data.
Permission was obtained from the National Comprehensive Cancer Network® for the reproduction of the DT Screening Tool Figure 1 (DIS-A) for use of the DT according to their NCCN Clinical Practice Guidelines in Oncology for Distress Management V.2.20
To address the findings of the original audit, a pilot was agreed that had a dual purpose in which a geographical placed specialist palliative care team would undertake to do the DT on new referrals to the given geographical area for one month.
The primary purpose was to screen for distress and the secondary purpose was to investigate the reticence of staff to use a diagnostic tool in their general clinical assessment of patients.
There are obviously potential limitations and concerns with regards having a nurse who does not have specific mental health expertise making a primary diagnosis of depression. However, the nature of the DT itself partly allays some of these, by providing a clear diagnostic tool. In addition, a competency framework is also in use within this study which ensured the nurses are trained in the use of the DT and also receive additional training in advanced communication. The nurses are also receiving clinical supervision of the work they are doing with patients to ensure quality of care.
In the 3rd audit 27 Clinical Nurse Specialist (CNS) were requested to complete a DT with a patient within two clinical sessions, in which the holistic assessment was made. All patients who scored between a 6 and 10 were to be discussed with a level IV clinician1. As described in the MVCN framework, health care professionals are divided by levels I-IV, based on their training and experience. Each level holds specific responsibilities, competencies, assessment methods, and interventions in regards to treatment [24] The levels grow in complexity as the number increases, with each level building upon the preceding level’s requirements [24].
Materials
Materials used obtain the data during clinical visits consisted of a Distress Thermometer (DT) and a writing utensil to record the results in the case notes. The DT data collected was recorded and encrypted computer using System1 (NHS) [25]. The data was displayed to clinical staff participating in the audit through the use of Microsoft Office PowerPoint (Microsoft, 2013).
Procedure
Team members agreed to complete a DT within two clinical visits. Timing of DT administration was based on their professional judgement and individual patient needs. No guidance was given as to when to use the DT with patients. The patient was asked for consent to use the DT as part of their care package. The results were recorded in the case notes, and information collected was dispersed to the team’s psychotherapist. The psychotherapist analysed the data, and organised it using Microsoft Excel and PowerPoint [26]. The results of patients scoring a 6 or above were consulted by level IV personnel, and then discussed a strategy of psychological support.
The second phase of the audit occurred between 1 February 2012 and 1 March 2012. At that time, there were 137 new referrals to the service. Staff worked towards completion of a DT within two clinical sessions at the time of assessment.
The third audit cycle took place between 1 May 2012 and 31 June 2012. It included the Heart Failure team, in addition to two specialist palliative care localities.
The fourth audit cycle took place between the 1 March and the 31 March 2013. It included all the previous services, as well as a local Hospice.
Results
1st Cycle
The findings of the piloted audit cycle identified that though 55% of patients were displaying signs of possible depression, only 25% were referred on for further psychological support. Of the initial reason for referrals made to the team, 35% of those referred were with the intention of acquiring psychological support services. This seems to be indicative of a general under-referral. The hypothesis that patients were being under referred for psychological support was confirmed, due in part to a lack of standardisation in assessment methods.
In seeking to remedy the issue and move forward, assessment was standardised though the inclusion of the DT in the secondary audit cycle. The DT ranks general distress on a scale of 1-10, with 10 being the greatest level of distress. In addition, it asks the participant to rank their top four issues of 23 Physical Problems, 5 Practical Problems, 3 Family Problems, 8 Emotional Problems, and 3 Spiritual/Religious concerns. Clinical Nurse Specialists used the DT and were trained in its use, as well as having advanced communications training.
2nd Cycle
The secondary audit cycle incorporated the use of the DT. Staff were advised to discuss all DT scoring a six or above with the psychotherapist. Of the 137 referrals received by the service, 23 DT were attempted to be completed, with 17% of patients having a DT score. Of those that were completed, thirteen scored between 0-5 on the scale, with the remaining 4 scoring in the range of 6-10 on the DT. 6 of the 23 DT attempted were not completed in their entirety.
3rd Cycle
The third audit cycle incorporated two specialist palliative care localities and the Heart Failure team, with the goal that all staff completed distress screening two clinical sessions, at the point of assessment with a patient. Feedback and expansion to the original DT training was provided by the team’s lead psychotherapist. At that time, there were 182 total accepted referrals to the teams. 81 DT were attempted, with 76 being completed fully. In the distress range of 1-5, 29 patients were scored. On the upper end of the scale between 6 -10, 13 patients scored. The 5 DT not completed were due to limitations of the patients capacity. Overall, 44.5% of patient assessments resulted in a DT being completed. That is an increase of 27.5% from the initial 17% in the second cycle. Due to the incorporation of the DT, 11 patients were referred on for psychological intervention. Of those patients, one refused further support.
4th Cycle
The final audit cycle incorporated the Hertfordshire Specialist Palliative Care Service, the Heart Failure Service and a Hospice. There were a total of 133 accepted referrals, with 109 referrals attempted to be completed. Of those attempted 41 were not scored because of capacity issues for the patient. Overall, 82% DT’s were attempted to be completed and 55% were fully completed. Of the services that took part in the 3rd audit cycle, 67% of DT’s were completed and 86% were attempted. Of the team that took part in all of the audit cycles, 91% of DT’s were attempted to be completed and 70% fully completed.
Resulted referrals of those that had a completed DT for psychological support was 21%. This was apportioned to 6% level 3 intervention and 47% level 4 intervention. Also 47% of DT’s in the west specialist palliative care team went on to have level 4 consultation and level 2 interventions planned and agreed. The 6% level 3 patients were also discussed at an internal Multi-disciplinary Team meeting to explore interventions. Because access to psychological support is commissioned within each individual agency, there was no ability to manage referrals according to identified scoring and clinical requirement (Table 1).
| Cycle | Findings | Recommendations |
|---|---|---|
| 1 | 55% of patients display depression characteristics. 25% were referred for psychological support. 35% of referrals to the team were for psychological support. 0% of patients were scored on a relevant tool to discern psychological distress. |
Identify a tool for assessment of depression. Record supervision and consultation in case notes and S1 as a form of MDT working re psychological care. |
| 2 | 17% of patients had a Distress Thermometer scoring. | Re-run audit All staff to complete a Distress Thermometer to identify psychological needs within two clinical sessions. Re-train all staff in the use of the Distress Thermometer. All patients who score 6-10 on the DT to be discussed with a level 4 clinician. The Heart Failure Service joined the use of the Distress Thermometer and audit process. |
| 3 | 44.4% of patients had a Distress Thermometer score completed. Some patients were assessed as being inappropriate to the service and therefore discharged without formal assessment. 42% of referrals from the West side of the team were referred for psychological support. 0% referrals were made to psychology in the North side of the team. Some patients were offered a referral to psychology services but refused. |
Implement the use of the Distress Thermometer and look to gain 100% compliance. All staff work to complete a Distress Thermometer within two clinical sessions as a mandatory action. All patients who score 6 or above to be discussed with a level 3/4 clinician present. Patients scoring 4 or 5 are to be discussed in clinical supervision. Develop a referral pathway for the Heart Failure Service. |
| 4 | 82% of DT’s were attempted and that 55% of DT’s were fully completed. Resulted referrals of those who had a DT completed for further psychological assessment was 17 (21%). 6% were referred to a level 3 worker at the Peace Hospice 12% were referred to the level 4 worker in the north 35% were referred to the level 4 worker in the west. Because of the DT score: 47% were consultations with a level 4 and level two interventions agreed. All 6 DT’s from IPU were taken to the clinical meeting at the Peace Hospice |
Continue to promote the use and look to gain 100% compliance. To continue to integrate the DT completion within two clinical sessions with a patient as part of the holistic assessment and this continue to be mandatory. Review and audit the DT in 6 months. To continue to use the framework in which: All DT’s scored at 6-10 are discussed at an MDT, supervision or consultation with a level 3/4 clinician. Pts scoring 4-5 is discussed in Supervision. Continue to use referral pathway for HFS and agree clinical Psychological input, via MDT for all patients. Promote and facilitate the use of the DT in other agencies to Ensure patient safety, equal access and identification of Psychological needs and commonality in practice to aid coordination. |
Table 1: summarizes the findings and recommendations for each cycle of the audit.
Discussion
The findings of the 1st audit identified that clinicians did not hold accurate beliefs about their ability to identify psychological distress. This enabled conversations to emerge where the introduction of a tool was seen as something that needed to be explored.
The second audit found that there was still reticence surrounding the use of a tool and the team agreed to implement screening that were mandatory. The next audit cycle showed that the team who had most used the tool had a higher level of completed screening and this was amplified in the 4th audit. This meant that nurses who had participated in all the audit cycles were more likely to complete the DT with patients than those who had just started using the DT. From this we can conclude that longitude of use and familiarity with the tools meant that patients were more likely to be screened. A further implication of this is that staff reticence was diminishing and their understanding of the use of such a tool was changing and that discussion informed practice and lead to further investigation. This finding was replicated in further audit cycles, amplifying the fact that an action research methodology supports change in the involvement of clinicians as part of the learning process. It also supports the evidencing through participation of best practice.
Following each audit cycle the team explored the implementation of a tool that identified distress for patients. This was in response to the base line audit that showed that they could not rely on their intuition to identify the distress of patients. The process clarified the psychotherapeutic role within the team and allowed for changes to occur in the use of clinical supervision. A major change was that they started to bring their case load to each session and we were able to identify strategies for those scoring below 6 and referral ideas for those above. This function also enabled a pathway to be created that functioned to provide a central referral point for team members and an identification process from which clinicians could act and a common language that fitted across services and organisations. Despite this and due to the disparity between commissioning and availability of psychotherapeutic clinicians, the right level of support was not always available according to identified need.
The result from this work is the potential for consistent and better distributed services, which are being explored in the continuum of on-going action research process. In seeking to implement the recommendations by the MVCN and its original findings from the 1st audit, it was established that psychometric tools and criteria would be implemented uniformly across the practices. A pattern of increased usage of the DT as part of the assessment process was established in each cycle, and this is likely to steadily increase as the tool continues to be introduced across practices.
By including the DT in our standard assessments, we hope to not only improve patient care and quality of life, but to aid in improving relationships with carers by enabling them to create a dialogue around a “good death”. This is yet to be quantified through a patient experience inquiry which will facilitate the on-going development of understanding, as we thicken the descriptions and take steps to further understand the effect of our actions.
This research is never ending. We are currently taking further steps to support other organisations, who work in a diverse way to implement the use of this tool to identify distress. These organisations are diverse and include a hospice at home team, a GP practice and a nursing home. All are engaged in delivering palliative care and are keen to find ways in which they can not only identify the distress level being experienced, but to be able to access psychological support and supervision as required.
Conclusion
The management of change is a complex process, which often falters because of power differentials which are constraining to the inherent knowledge held by each professional group.
Action research is not only a way of conducting an investigation, but a clinical tool that values difference, enters into dialogue and uses a feedback process from which actions taken can be evaluated and modified. It increases the supporting evidence that shapes the basis of practice and it reduces the likelihood of slavish adherence to certainty in practice and forms a canopy of safety from which new understanding and practice can emerge.
This research has found that in the action of discovery change in clinical and diagnostic practice takes place. This in turn has an impact on the identification of distress and the access to appropriate psychological support for patients and their families.
1Although a score of 6 would not normally be seen by a level IV clinician, the team did not have access to a level III clinician to support this work.
References
- http://www.nhs.uk/CarersDirect/guide/bereavement/Pages/Accessingpalliativecare.aspx
- Johnston B, Smith LN (2006) Nurses' and patients' perceptions of expert palliative nursing care. Journal of Advanced Nursing 54(6): 700-709.
- Wasteson B, Brenne E, Hotopf M, Lloyd-Williams M, Kaasa S, et al. (2009) Depression assessment and classification in palliative cancer patients: A systematic literature review. Palliative Medicine 23(8): 739-753.
- http://www.nimh.nih.gov/health/topics/depression/index.shtml
- Diagnostic and statistical manual of mental disorders: DSM-IV (1994) Washington, DC: American Psychiatric Association.
- Massie M, Holland J (1990) Depression and the cancer patient. Journal of Clinical Psychiatry 75: 12-17.
- Endicott J (1984). Measurement of Depression in Patients with Cancer. Cancer 53(10): 2243-2249.
- Noorani NH, Montagnini M (2007) Recognizing Depression in Palliative Care Patients. Journal of Palliative Medicine 10: 458-464.
- Harrison J (1995). The impact of cancer on key relatives: A comparison of relative and patient concerns. European Journal of Cancer 31(11): 1736-1740.
- Massie M (1992) The cancer patient with pain: Psychiatric complications and their management. Journal of Pain and Symptom Management 75: 99-109.
- Chochinov H, Wilson K, Enns M, Mowchun N, Lander S, et al. (1995) Desire for death in the terminally ill. American Journal of Psychiatry 152: 1185-1191.
- Currie S (1992) Book Reviews: Dying of Cancer: The Final Year of Life. Allan Kellehear. Melbourne. Harwood Academic Publishers, Journal of Sociology 28(2): 243-245.
- Peryiakoil V, Hallenbeck J (2002) Identifying and Managing Preparatory Grief and Depression at the End of Life. American Family Physician 1(65): 883-891.
- Mitchell AJ (2007) Pooled Results From 38 Analyses of the Accuracy of Distress Thermometer and Other Ultra-Short Methods of Detecting Cancer-Related Mood Disorders. Journal of Clinical Oncology 25: 4670-4681.
- Gessler S, Low J, Daniells E, Williams R, Brough V, et al. (2008) Screening for distress in cancer patients: Is the distress thermometer a valid measure in the UK and does it measure change over time? A prospective validation study. Psycho-Oncology 17(6): 538-547.
- Roth AJ, Kornblith AB, Batel-Copel L, Peabody E, Scher HI, et al. (1998) Rapid screening for psychological distress in men with prostate carcinoma. Cancer 82: 1904-1908.
- Zwahlen D, Hagenbuch N, Carley MI, Recklitis CJ, Buchi S (2008) Screening cancer patients' families with the distress thermometer (DT): A validation study. Psycho-Oncology 17: 959-966.
- Adelman C (1993) Kurt Lewin and the Origins of Action Research. Educational Action Research 1(1): 7-24.
- http://www.healthcareimprovementscotland.org/welcome_to_healthcare_improvem.aspx
- http://www.casp-uk.net/
- Lloydwilliams M, Shiels C, Dowrick C (2007) The development of the Brief Edinburgh Depression Scale (BEDS) to screen for depression in patients with advanced cancer. Journal of Affective Disorders. 99: 259-264.
- http://www.who.int/mental_health/publications/whoqol/en/
- http://www.nccn.org/patients/resources/life_with_cancer/pdf/nccn_distress_thermometer.pdf
- http://pro.mountvernoncancernetwork.nhs.uk/
- http://www.connectingforhealth.nhs.uk/
- http://office.microsoft.com/en-us/powerpoint/
Relevant Topics
- Caregiver Support Programs
- End of Life Care
- End-of-Life Communication
- Ethics in Palliative
- Euthanasia
- Family Caregiver
- Geriatric Care
- Holistic Care
- Home Care
- Hospice Care
- Hospice Palliative Care
- Old Age Care
- Palliative Care
- Palliative Care and Euthanasia
- Palliative Care Drugs
- Palliative Care in Oncology
- Palliative Care Medications
- Palliative Care Nursing
- Palliative Medicare
- Palliative Neurology
- Palliative Oncology
- Palliative Psychology
- Palliative Sedation
- Palliative Surgery
- Palliative Treatment
- Pediatric Palliative Care
- Volunteer Palliative Care
Recommended Journals
- Journal of Cardiac and Pulmonary Rehabilitation
- Journal of Community & Public Health Nursing
- Journal of Community & Public Health Nursing
- Journal of Health Care and Prevention
- Journal of Health Care and Prevention
- Journal of Paediatric Medicine & Surgery
- Journal of Paediatric Medicine & Surgery
- Journal of Pain & Relief
- Palliative Care & Medicine
- Journal of Pain & Relief
- Journal of Pediatric Neurological Disorders
- Neonatal and Pediatric Medicine
- Neonatal and Pediatric Medicine
- Neuroscience and Psychiatry: Open Access
- OMICS Journal of Radiology
- The Psychiatrist: Clinical and Therapeutic Journal
Article Tools
Article Usage
- Total views: 16353
- [From(publication date):
May-2015 - Aug 18, 2025] - Breakdown by view type
- HTML page views : 11663
- PDF downloads : 4690