Difference in Blood Pressure between Arms of Normotensive Female Farmers in the Semi-arid Midlands of Kenya
Received: 10-Feb-2015 / Accepted Date: 28-Mar-2015 / Published Date: 02-Apr-2015 DOI: 10.4172/2161-1165.S1-002
Abstract
Introduction: Hypertension has been identified as the leading risk factor for mortality worldwide. The common clinical practice of one arm blood pressure measure and the presence of a difference between arm measurements is likely to lead to delayed diagnosis of hypertension and is associated with a higher prevalence of poor control of hypertension.
Objective: To examine inter-arm differences that could give rise to undetected hypertension. Methods: A household cross-sectional survey was undertaken amongst 293 females who were participating in agricultural farm activities in lower Eastern Kenya. Six alternating arm blood pressure readings were taken, three on each arm with 3 minutes rest between each session.
Results: Marginal but statistically significant inter-arm differences were observed in mean systolic blood pressure (right-arm 124.4 ± 12.5 mmHg; left-arm 123.3 ± 13.2 mmHg) and diastolic blood pressure (right-arm 75.4 ± 8.9 mmHg; left-arm 76.2 ± 9.1 mmHg). Right arm blood pressure readings indicated a higher prevalence of prehypertension and hypertension (51.2% and 12.3%) than left-arm (47.8 and 10.6%; p=0.001) readings. Statistically significant intra-arm differences (p=0.001) were observed between the 1st vs. 2nd and the 1st vs. 3rd right and left arm systolic blood pressure and diastolic blood pressure readings respectively.
Conclusion and recommendation: Repeated blood pressure readings when measured on both arms can assist in more accurate identification of elevated blood pressure and timely diagnosis of hypertension. Population-wide studies are needed to examine the long term significance of blood pressure differences between arms.
Keywords: Blood Pressure; Inter arm blood pressure difference; Repeat blood pressure readings
166923Introduction
Blood pressure (BP) is a measure of the force that the circulating blood exerts on the walls of the main arteries. The pressure wave transmitted along the arteries with each heartbeat is easily felt as the pulse—the highest (systolic) pressure is created by the heart contracting and the lowest (diastolic) pressure is measured as the heart fills [1]. BP serves as a biomarker for the disease hypertension [2]. Hypertension or High blood pressure (HBP) has been identified as the leading global risk for mortality worldwide, and is ranked third as a cause of disability-adjusted life-years [3] and responsible for 13% of deaths globally [4]. Hypertension affects approximately 20% of adults worldwide and is a major, but modifiable, contributory factor to cardiovascular disease such as coronary heart disease and stroke [5].
It confers a substantial risk of cardiovascular disease [6] particularly in the presence of concomitant risk factors, much of which is at least partially reversible with treatment [7]. Measurement of BP is the investigation most frequently undertaken in primary care settings and patients often have different BP measurements in their arms [8]. The presence of a difference between arm measurements has been implicated in a delayed diagnosis of hypertension. It is associated with a higher prevalence of poor control of hypertension, as the failure to standardise measurement to the arm with the highest reading can delay decisions about management [9]. Incorrectly classifying a hypertensive patient as normotensive fails to identify their increased risk for vascular events and kidney disease. Incorrectly classifying a patient with normal blood pressure as hypertensive can result in unnecessary worry, time costs, medical costs and exposure to treatment-related harm [10].
Ideally, BP should initially be measured in both arms and the arm with the higher readings should be used for subsequent measurements. A difference in readings between the arms can be expected in 20% of patients [10,11]. If this difference amounts to >20 mmHg for systolic or >10 mmHg for diastolic on three consecutive readings, further investigation is indicated [12,13]. Current clinical guidelines recognise the need to measure BP in both arms [9]. Part of the assessment of raised BP should include measurement in both arms, as around 6% of the adult population has at least a 10 mmHg difference between arms. This proportion increases with cardiovascular risk factors such as age and diabetes [5]. For more than 25 years, hypertension guidelines have recommended measuring BP in both arms, but acceptance among general practitioners is low [5]. Appreciation of the presence of an Inter Arm Differences (IAD) clearly is vital for the accurate diagnosis and consistent management of hypertension [8]. Suffice to say that the relationship between inter-arm systolic blood pressure difference and risk of future cardiovascular disease is uncertain [14].
Ethical consideration
Prior to undertaking the study, ethical clearance was granted by Kenya Medical Research Institute/National Ethics Review Committee and signed informed consents obtained from all the respondents.
Sample size and sampling
This was a descriptive cross-sectional study of blood pressure in women participating in agricultural activities in the semi-arid Lower Midland agro-ecological zones (AEZ) in Makueni and Machakos counties of Kenya. Farming in these areas is predominantly small scale, combining both crop production and animal production [15]. The farmers organize themselves in designated ‘farmer groups’. The principle behind these units is to leverage available support from various institutions and/or organizations and share farming experiences and lessons learned from closer collaboration. Acknowledging these networks, we choose to construct a sampling frame using farmer groups as the primary sampling unit. From the full list in the two counties, 72 farmer groups were randomly selected and a quick household count was undertaken to establish the number, age and sex of members in each household belonging to the selected farmer groups. Simple random sampling was used to alternately select 4 or 5 households from each farmer group for enrolment in the survey. From the 324 households in the sampling frame, 293 women of ages 15 to 46 year (response rate 90%) were successfully recruited and assessed. All nonresponses were due to absence at the time of the household visits.
Subjects
The participants were women farmers participating in a Kenya, Canada collaborative 42 months Canadian International Food Security Research Fund (CIFSRF) funded project titled: “Innovations for resilient farming in semi-arid midlands of Kenya. The data reported here were collected in May and June 2012.
Data collection
Demographics and social economic statistics: We used structured, pre-tested questionnaires for recording general information on social and economic status, level of education, farming practices and demographic details.
Clinical Assessment: BP measurements were undertaken by registered and trained nurses using digital population Omron Digital Blood Pressure Machines (Omron M6 HEM-7211-E8 (v), Omron Healthcare UK Ltd) standard upper arm cuffs. Sequential BP measurements were taken after 10 minutes rest before the initial measurement and 3 minutes rest between each measurement with the respondent in sitting position, with arms supported. A total of six BP measurements were undertaken (3 measurements on each arm). The readings on each side were averaged to obtain the mean systolic and diastolic BP measurements for each woman. In addition, respondent characteristics, reported medical history and risk factors information was recorded as reported by the women.
Statistical methods
We used SPSS version 20.0 (SAS Institute) for data analysis to generate measures of location and spread for continuous variables and proportions for categorical variables. Differences between BP data were assessed with the Student t-test and agreement between BP data was computed with Altman-Bland plots (16) (“Bland, JM and Altman DG 1999). The X2 test was used for testing differences of proportions. Differences were considered statistically significant at p<0.05.
Results
The mean age and Body Mass Index was 29.6 ± 6.6 years and 21.9 ± 3.5 kg/m2 respectively. Table 1 shows further characteristics of women who participated in the study. All the women were engaged in various farming activities, using the resilient agricultural technologies introduced by the CIFSRF project. As shown in Table 1, Findings indicate that the overall SBP level was marginally above the WHO [6] (recommended optimal (SBP<120 mmHg) while DBP was within the normal range (DBP<80 mmHg). BP taken on the right arm identified a slightly higher proportion of women as pre-hypertensive (51.2%; SBP 120-139/DBP 80-89) and hypertensive (12.3%; >SBP 140/DBP 90) compared to BP taken on the left arm where pre-hypertension and hypertension was present in 47.8% and 10.6% (P=0.001) of the women respectively. 24.9% and 64.5% of the women reported abnormal menstrual cycle and use of contraceptives respectively. No significant differences were observed between blood pressure levels and abnormal menstrual cycle and use of contraceptives in these apparently healthy women farmers. A significant difference was found between nutritional status and right arm SBP (P=0.043) only. No significant difference was found between nutritional status and left arm SBP (P=0.122), right arm DBP (P=0.224) nor left arm DBP (P=0.281).
| Description | %Distribution |
|---|---|
| Age categories (yrs) | |
| 15-25 | 29.2 |
| 26-35 | 52.4 |
| 36-46 | 18.4 |
| Ever smoked or used drugs | 0 |
| Alcohol intake | 1.7 |
| Abnormal Menstrual cycles | 24.9 |
| Use of Contraceptives | 64.5 |
| Nutritional status | |
| Underweight | 14.3 |
| Normal | 67.9 |
| Overweight | 15.4 |
| Obese | 2.4 |
| BP measurements | |
| Right arm BP | |
| Pre-hypertensive | 51.2 |
| hypertensive | 12.3 |
| Left arm BP | |
| Pre-hypertensive | 47.8 |
| hypertensive | 10.6 |
Table 1: Characteristics of the respondents.
Inter-arm variability in blood pressure
A comparisons of the mean SBP and DBP on the right and left arms at subsequent measurements showed significant differences between right and left arm SBP and right and left arm DBP second and third readings. The SBP and DBP averages also demonstrated a significant difference between BP readings when taken on different arms. Mean right arm SBP was significantly higher than the mean left arm SBP (P=0.003) while the inverse was observed for the DBP where the mean left arm DBP was higher than the right arm DBP (P=0.010). on comparing mean differences in SBP and DBP readings between arms at different measurement time points, no significant mean differences in BP were observed between 1st sessions for both systolic (P=0.067) and diastolic (P=0.745) readings. However, all the subsequent readings, including the average, showed significant differences between BP measurements on each arm.
Systolic blood pressure
Tests of Within-Subjects Effects according to Mauchly's Test of Sphericity, using two way ANOVA showed a significant difference in variances within measurement. As our data violated the assumption of sphericity, we used the "Greenhouse-Geisser" estimates. The mean scores for right SBP measurements were statistically significantly different (F (1.814, 529.689)=26.358, P=0.001) and Left SBP (F(1.881, 549.376)=30.866, p<0.001).
Table 2 presents the results of pairwise Comparisons using Bonferroni post hoc test, which allows us to discover which specific means differed. There was a significant difference in marginal mean systolic BP measurements between Measurement 1 and Measurement 2 (p<0.001), and between Measurement 1 and Measurement 3 (p<0.001). Similarly there was a significant differences between Measurement 2 and Measurement 3 (p <0.001).
| Measurement time | Mean Difference (I-J) | Std. Error | p value | 95% Confidence Interval for Difference | ||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Marginal means for BP Left and Right Systolic | ||||||
| Measurement 1 | Measurement 2 | 2.613 | 0.325 | <0.001 | 1.833 | 3.39 |
| Measurement 3 | 3.667 | 0.566 | <0.001 | 2.174 | 4.621 | |
| Measurement 2 | Measurement 1 | -2.613 | 0.325 | <0.001 | 3.933 | -1.83 |
| Measurement 3 | 1.055 | 0.333 | 0.005 | 0.254 | 1.855 | |
| Measurement 3 | Measurement 1 | -3.667 | 0.397 | <0.001 | 4.621 | -2.174 |
| Measurement 2 | -1.055 | 0.333 | 0.005 | -1.855 | -0.354 | |
| Marginal means for BP Left and Right Diastolic | ||||||
| Measurement 1 | Measurement 2 | 0.922 | 0.282 | 0.003 | 0.245 | 1.598 |
| Measurement 3 | 2.275 | 0.301 | <0.001 | 1.552 | 2.997 | |
| Measurement 2 | Measurement 1 | 0.922 | 0.282 | 0.003 | -1.598 | -0.245 |
| Measurement 3 | 1.353 | 0.284 | <0.001 | 0.672 | 2.035 | |
| Measurement 3 | Measurement 1 | -2.275 | 0.301 | <0.001 | -2.997 | -1.552 |
| Measurement 2 | -1.353 | 0.284 | <0.001 | -2.035 | -0.672 | |
Table 2: Pairwise Comparisons for DBP using Bonferroni post hoc test.
Diastolic blood pressure
For the diastolic BP, the Tests of Within-Subjects Effects according to Mauchly's Test of Sphericity, showed no significant difference in variances within measurement. Since the diastolic BP data did not violate the assumption of sphericity, we used the "Sphericity-Assumed" estimates. The mean scores for Diastolic BP measurements were statistically significantly different (F(2.000, 1168.000) =31.348, p<0.001).
Pairwise Comparisons for DBP using Bonferroni post hoc test, are also presented in table 5. There was a significant difference in marginal mean diastolic BP measurements between Measurement 1 and Measurement 2 (p=0.003), and between Measurement 1 and Measurement 3 (p<0.001). Similarly there was a significant differences between Measurement 2 and Measurement 3 (p <0.001).
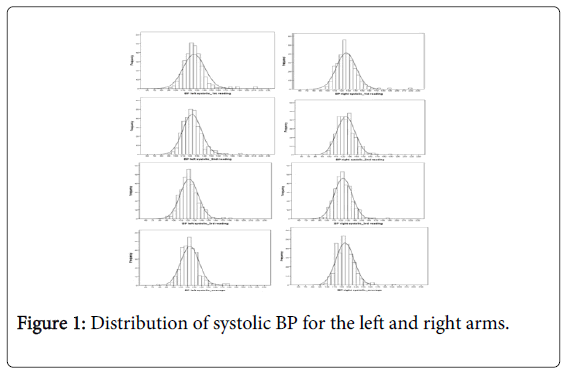
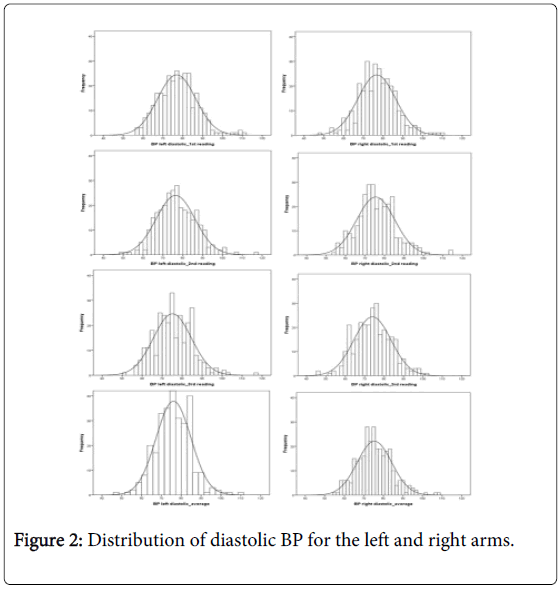
In Figures 1, 2 and Table 3 we demonstrate the distribution of DBP and SBP measurements in the right and left arms for all the reading sessions and the average distributions for each case. Although some differences between right and left arm SBP and DBP readings for all the 1st, 2nd and 3rd readings were significant on statistical testing, the figures illustrate that the group measurements have meaningful biological agreement.
| Left arm Systolic readings | Right arm Systolic readings | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| BP (mmHg) | 1st | 2nd | P | 3rd | P | MeanBP | MeanPulse rate | 1st | 2nd | P | 3rd | P | Mean BP | Mean Pulse rate |
| SD | 15.3 | 13.2 | 14.3 | 13.2 | 12 | 15.7 | 13.7 | 12.7 | 12.6 | 12 | ||||
| Min | 92 | 91 | 91 | 79 | 48.3 | 99 | 94 | 92 | 92 | 49.7 | ||||
| Max | 212 | 189 | 180 | 178 | 129.7 | 221 | 187 | 187 | 191 | 121.7 | ||||
| Left arm Diastolic readings | Right arm diastolic readings | |||||||||||||
| BP (mmHg) | 1st | 2nd | P | 3rd | P | Meanleft arm BP | MeanPulse rate | 1st | 2nd | P | 3rd | P | Meanleft arm BP | Mean Pulse rate |
| Mean | 77.2 | 76.3 | <0.083 | 74.9 | <0.001 | 76.1 | 82.5 | 76.6 | 75.5 | <0.008 | 74.1 | <0.001 | 75.4 | 82.7 |
| SD | 11.3 | 9.7 | 10.3 | 8.7 | 12 | 10 | 9.8 | 9.9 | 8.8 | 12 | ||||
| Min | 57 | 49 | 51 | 54 | 48.3 | 48 | 54 | 46 | 55 | 49.7 | ||||
| Max | 111 | 116 | 116 | 111 | 129.7 | 109 | 114 | 116 | 108 | 121.7 | ||||
*P<0.001 significant difference between mean right arm and Left arm Systolic and Diastolic BPs
Table 2: Mean BP and pulse rate measurements in the left and right arms.
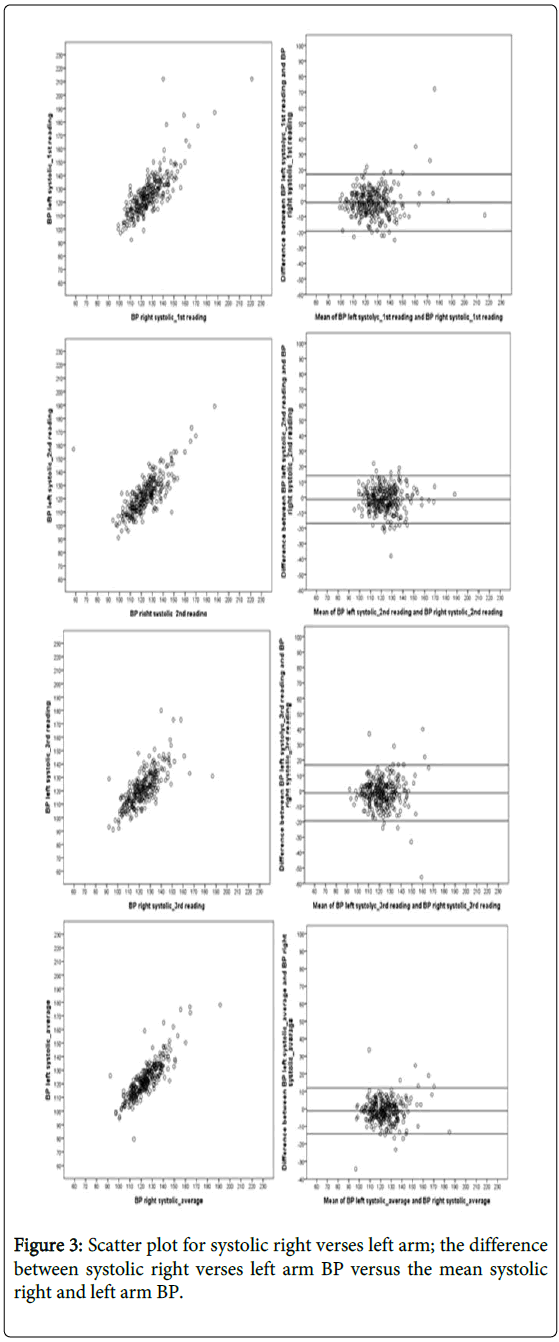
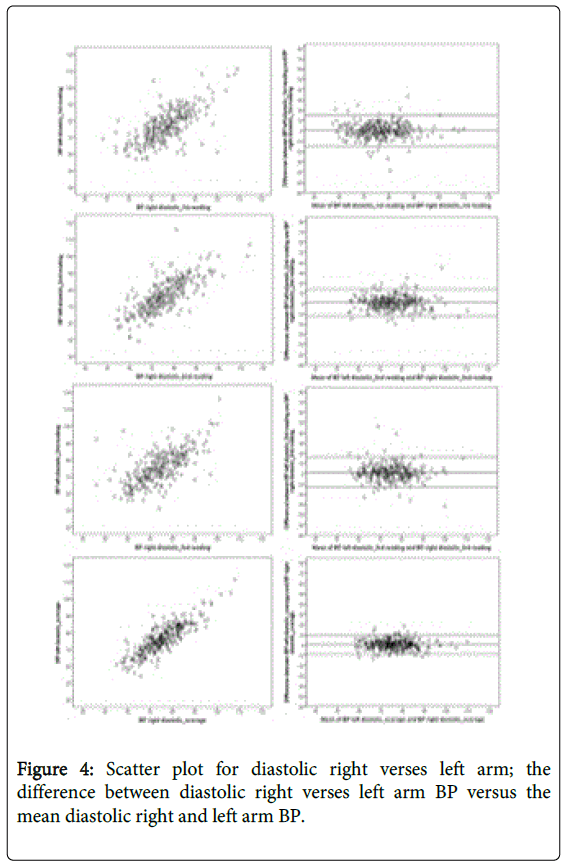
Figures 3 and 4 shows the sequence in measurements for each arm as a scatter plots for systolic and diastolic mean differences respectively, together with the Altman-Bland plots for agreement. The mean difference in SBP between arms amounted to -1.18 mmHg (95% CI:-1.94-0.42]) and the mean difference in DBP between arms to 0.72 mmHg (95% CI: 0.17-1.27) Table 4.
| Variable | n | Systolic | Diastolic | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI | Mean | SD | 95% CI | ||||
| Lower | Upper | Lower | Upper | ||||||
| BP left_1st reading | 293 | 125.6 | 15.3 | 123.9 | 127.4 | 76.9 | 9.6 | 75.8 | 78 |
| BP right_1st reading | 293 | 126.6 | 14.2 | 125 | 128.3 | 76.8 | 9.5 | 75.7 | 77.9 |
| p value | 0.067 | 0.745 | |||||||
| BP left_2nd reading | 293 | 122.8 | 13.2 | 121.3 | 124.3 | 76.3 | 9.7 | 75.2 | 77.5 |
| BP right_2nd reading | 293 | 124.2 | 13.3 | 122.7 | 125.7 | 75.5 | 9.8 | 74.3 | 76.6 |
| p value | 0.003 | 0.027 | |||||||
| BP left_3rd reading | 293 | 121.8 | 12.9 | 120.3 | 123.3 | 75.1 | 9.5 | 74 | 76.2 |
| BP right_3rd reading | 293 | 123.1 | 12.7 | 121.6 | 124.5 | 74 | 9.6 | 72.9 | 75.1 |
| p value | 0.02 | 0.01 | |||||||
| BP left_average | 293 | 123.3 | 13.2 | 121.8 | 124.8 | 76.1 | 8.7 | 75.1 | 77.1 |
| BP right_average | 293 | 124.5 | 12.6 | 123 | 125.9 | 75.4 | 8.8 | 74.4 | 76.4 |
| p value | 0.003 | 0.01 | |||||||
*Significant at P<0.05 BP: Blood Pressure
Table 4: Paired comparisons of left and right systolic and diastolic BP.
| Measurement time | Mean Difference (I-J) | Std. Error | p value | 95% Confidence Interval for Difference | ||
|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||
| Right arm systolic | ||||||
| Measurement 1 | Measurement 2 | 2.420* | 0.428 | <0.001 | 1.39 | 3.45 |
| Measurement 3 | 3.536* | 0.566 | <0.001 | 2.174 | 4.898 | |
| Measurement 2 | Measurement 1 | -2.420* | 0.428 | <0.001 | -3.45 | -1.39 |
| Measurement 3 | 1.116041 | 0.491 | 0.071 | -0.066 | 2.298 | |
| Measurement 3 | Measurement 1 | -3.536* | 0.566 | <0.001 | -4.898 | -2.174 |
| Measurement 2 | -1.11604 | 0.491 | 0.071 | -2.298 | 0.066 | |
| Left arm systolic | ||||||
| Measurement 1 | Measurement 2 | 2.805 | 0.489 | <0.001 | 1.628 | 3.983 |
| Measurement 3 | 3.799* | 0.558 | <0.001 | 2.455 | 5.142 | |
| Measurement 2 | Measurement 1 | -2.805* | 0.489 | <0.001 | -3.983 | -1.628 |
| Measurement 3 | 0.993 | 0.452 | 0.086 | -0.094 | 2.081 | |
| Measurement 3 | Measurement 1 | -3.799* | 0.558 | <0.001 | -5.142 | -2.455 |
| Measurement 2 | -0.993 | 0.452 | 0.086 | -2.081 | 0.094 | |
| Right arm Diastolic | ||||||
| Measurement 1 | Measurement 2 | 1.283* | 0.379 | 0.002 | 0.371 | 2.196 |
| Measurement 3 | 2.782* | 0.434 | <0.001 | 1.738 | 3.825 | |
| Measurement 2 | Measurement 1 | -1.283* | 0.379 | 0.002 | -2.196 | -0.371 |
| Measurement 3 | 1.498* | 0.371 | <0.001 | 0.604 | 2.392 | |
| Measurement 3 | Measurement 1 | -2.782* | 0.434 | <0.001 | -3.825 | -1.738 |
| Measurement 2 | -1.498* | 0.371 | <0.001 | -2.392 | -0.604 | |
| Left arm Diastolic | ||||||
| Measurement 1 | Measurement 2 | 0.56 | 0.418 | 0.543 | -0.446 | 1.565 |
| Measurement 3 | 1.768* | 0.417 | <0.001 | 0.763 | 2.773 | |
| Measurement 2 | Measurement 1 | -0.56 | 0.418 | 0.543 | -1.565 | 0.446 |
| Measurement 3 | 1.208* | 0.429 | 0.016 | 0.175 | 2.242 | |
| Measurement 3 | Measurement 1 | -1.768* | 0.417 | <0.001 | -2.773 | -0.763 |
| Measurement 2 | -1.208* | 0.429 | 0.016 | -2.242 | -0.175 | |
Table 5: Between arm paired comparisons for left and right systolic and diastolic BP.
Discussion
In this cross-sectional survey of women farmers in the semi-arid midlands of Kenya, we showed the importance of taking repeated BP measurements on both arms to ensure that all those at risk of, or with, hypertension are identified correctly and timely.
A difference in BP readings between arms has been observed in several apparently healthy populations [11].
Our study measured BP in both arms to examine if there are differences that could lead to undetected high blood pressure.
The findings showed marginal, though statistically significant differences in mean BP between arms.
The BP differences between the right and left arm were significant (P=0.001) and also inter-arm BP differences between successive sessions were significant, demonstrating a factual possibility of misdiagnosis of HBP, or BP misclassification, depending on which arm is used and how many BP measurements are taken.
However, even though BP recordings frequently differ between arms, the extent to which these differences are reproducible and whether the differences have prognostic importance is unclear [13].
The mean inter-arm differences at the three time points in this study found no significant difference during the first readings for both systolic and diastolic BP measurements.
However, the significant mean inter-arm differences between the subsequent BP measurements suggest that misclassification and failed diagnosis of stage 1 hypertension is possible, especially when based on single measurements only, which tends to be the common practice in clinical settings Table 4.
The BP variability between arms has been described as the ‘interarm difference’ phenomenon. It was first recognised more than 100 years ago [8]. Hence, 13 out of 15 blood pressure guidelines recommend that BP should be measured on both arms during initial clinical evaluation [16,17] and the arm with the higher BP be used at subsequent visits, but there is little evidence that this is followed [18]. Agarwal et al. [13] have pointed out that BPs differ between arms, with the right arm consistently reading higher by a small amount. Kim [19] observed that if the difference is 10 mmHg or more on repeated simultaneous measurements, the likelihood of peripheral vascular disease of the upper extremities is high and further diagnostic evaluation is warranted, especially in people with other risk factors for cardiovascular disease. Kim [19] also recommended that subsequent blood pressure monitoring should use the arm with the higher readings and these findings agree with those of Martin et al. [18,19] who suggested that differences in right and left arm pressures may be caused by undiagnosed peripheral vascular disease affecting the upper limbs and may therefore predict an increased risk of cardiovascular disease.
Previous studies have suggested a bias towards higher BP readings from the right arm, whereas others have failed to show this. Studies looking specifically at left or right handedness have also failed to show an association with the arm producing the higher reading [11].
In 1960, using aneroid sphygmomanometers, Harrison et al. performed three simultaneous blood pressure measurements on both arms at one minute intervals in 447 patients. 50% of these subjects had between-arm differences in systolic blood pressure greater than or equal to 5 mmHg and 44% had differences in diastolic blood pressure of at least 5 mmHg.
Other studies have reported a prevalence of inter-arm differences in BP ranging from 12.0 to 18.4% for a systolic difference (sIAD) X20 mmHg and from 13.0 to 33.7% for a diastolic difference (dIAD) X10 mm Hg in various populations (8). In contrast, the systolic and diastolic BP differences were -1.18 mmHg and 0.72 mmHg for SBP and DBP, respectively in this rural Kenyan community population.
Strengths and limitations of this study
Since no strict order of first arm measurement was adopted, any difference observed between any arms does not suggest any systematic bias. Blood pressure measurements are expected to reduce with subsequent sequential measurements. We used sequential measurements as opposed to simultaneous measurements, however, it’s suggested that simultaneous measurements using two BP machines would be ideal to confirm the blood pressure differences between arms as suggested in other studies [11,14]. This study used a cross-sectional survey design and therefore had only one time contact for BP assessments thus provides inter-arm BP differences over a short period.
Conclusion
The mean population BP in our group of free-living, apparently healthy adult women fell fairly within the normal range and this could explain why the differences between arms was slightly lower than reported in other studies. Although several studies have reported that blood pressure measurements can differ in a consistent manner between the two arms our results do not support this finding. What our findings do support is that a limited awareness of this difference may lead to errors in the diagnosis and treatment of stage 1 hypertension. The prevalence of interarm blood pressure differences is often higher in hypertensive subjects than in normotensives. Our findings can be extended to the care of normotensives in a clinical setting and support the guidelines regarding taking BP measurements on both arms at the initial assessment and for timely diagnosis and further vascular assessments where risks are suspected. This study found that there are inter-arm measurement differences, however, considering that the BP differences in our study was determined over a few hours (short term variability) which has been defined by Hocht et al. [20] as the ascillation of blood pressure within 24 hours. For appropriate confirmation of blood pressure differences between arms in populations, it may be an important consideration for future studies to assess for long term differences, which may include day to day, visit or seasonal assessments.
Acknowledgements
This work was carried out with the aid of grant from the Canadian International Food Security Research Fund (CIFSRF), a program of Canada’s International Development Research Centre (IDRC) Project Number 106510 undertaken with the financial support of the Government of Canada provided through Foreign Affairs, Trade and Development Canada (DFATD). The authors wish to acknowledge the support of Lutta W. Muhammad and Gordon M. Hickey, principal investigators of the CIFSRF project for the Kenya Agricultural and Livestock Research Organization (KALRO) (former Kenya Agricultural Research Institute (KARI)) and McGill University, respectively. Further acknowledgement is to all the farmers who participated in the study. The authors also thank the Director of KEMRI for granting permission to undertake this study.
Authors Contributions
ZB conceptualized the study, developed the research design, planned the survey, led the field teams and participated in data collection, analysis and drafted the manuscript. MM was involved in the research design and analyzed and interpreted the data. LK, JK, and FH read and contributed to the manuscript. All authors approved the final manuscript.
References
- Lawes CMM, Hoorn S Vander, Law MR, Elliott P, Macmahon S, et al. (2004)High blood pressure.
- Giles TD, Materson BJ, Cohn JN, Kostis JB (2009) Definition and Classification of Hypertension?: An Update. 11:611-4.
- Hendriks ME, Wit FWNM, Roos MTL, Brewster LM, Akande TM, et al. (2012) Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities.PLoS One, 7:e32638.
- WHO (2009) Global health risks. Mortality and burden of disease attributable to selected major risks. p. 70.
- Parker E, Glasziou P (2009) Use of evidence in hypertension guidelines: should we measure in both arms? Br J Gen Pract 59:e87-92.
- WHO (2005) Clinical guidelines for the management of hypertension. Cairo: EMRO Techinical Publication Series, 29.
- McAlister FA, Straus SE (2001) Evidence based treatment of hypertension. Measurement of blood pressure: an evidence based review. BMJ 322:908-11.
- Clark CE, Campbell JL, Powell RJ (2007) The interarm blood pressure difference as predictor of cardiovascular events in patients with hypertension in primary care: cohort study. J Hum Hypertens 21(8):633-8.
- Clark CE, Taylor RS, Shore AC, Ukoumunne OC, Campbell JL (2012) Association of a difference in systolic blood pressure between arms with vascular disease and mortality: a systematic review and meta-analysis. Lancet [Internet]. Elsevier Ltd, 379:905-14.
- Frese EM, Fick A, Sadowsky HS (2011) Blood pressure measurement guidelines for physical therapists. CardiopulmPhysTher J 2011;22:5-12.
- Clark CE, Taylor RS, Shore AC, Campbell JL (2012) The difference in blood pressure readings between arms and survival: primary care cohort study. Bmj 344:e1327-e1327.
- Jevon P (2006) Blood pressure measurement. Part one: taking a manual reading. Nurs Times 103(18):26-7.
- Agarwal R, Bunaye Z, Bekele DM (2008) Prognostic significance of between-arm blood pressure differences. Hypertension 51(3):657-62.
- Weinberg I, Gona P, O’Donnell CJ, Jaff MR, Murabito JM (2014) The systolic blood pressure difference between arms and cardiovascular disease in the Framingham Heart Study. Am J Med. Elsevier Inc127(3):209-15.
- Jaetzold R, Schmidt H, Hornet ZB (2006) Farm Management Handbook of Kenya Subpart,(2ndedn). Nairobi: Publisher Ministry of Agriculture, Kenya, in Cooperation with the German Agency for Technical Cooperation.
- Bland JM, Altman DG (1999) Measuring agreement in method comparison studies. Stat. Meth. pp. 135-60.
- NHS (2011) Quick reference guide. Hypertension, Clinical Managment of promary hypertension in adults. p. 16.
- Martin U, Holder R, Hodgkinson J, McManus R (2013) Inter-arm blood pressure differences compared with ambulatory monitoring: a manifestation of the “white-coat†effect? Br J Gen Pract.
- Kim D (2012) Differences in blood pressure between arms. BMJ-British Med J.
- Höcht C (2013) Blood Pressure Variability: Prognostic Value and Therapeutic Implications. IntSch Res Not.
Citation: Bukania ZN, Mwangi M, Kaduka LU, Kimiywe J, van der Haar F (2015) Difference in Blood Pressure between Arms of Normotensive Female Farmers in the Semi-arid Midlands of Kenya. Epidemiology (sunnyvale) S1:002. DOI: 10.4172/2161-1165.S1-002
Copyright: © 2015 Bukania ZN, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 15132
- [From(publication date): 0-2015 - Aug 30, 2025]
- Breakdown by view type
- HTML page views: 10529
- PDF downloads: 4603