Evaluation of Health Literacy in Veteran Affairs Outpatient Population: A Focus on Patient Self-Perceived Health Status
Received: 04-May-2018 / Accepted Date: 28-May-2018 / Published Date: 04-Jun-2018 DOI: 10.4172/2161-0711.1000613
Abstract
Health literacy is of great importance for clinicians to maximize patient involvement and in the effective delivery of healthcare services. Health literacy driven health communication strategies may encourage appropriate and optimal use of healthcare resources and medications. We evaluated health literacy level in veterans with unique population demographics and focused on patient self-perceived health status (SPHS). Veterans (N=194) were enrolled in this cross-sectional study. Only 40% had poor or inadequate health literacy level. Older individuals displayed poorer health literacy level. 57.2% of the patients had good/above SPHS. Patients with good or above SPHS had 1.7 times higher (OR: 1.68, 95% CI=0.79-3.54) compared to patients with below good SPHS. Veterans with hospitalization were 11% less likely (OR=0.89) to report good or adequate health literacy level compared to those not hospitalized. Veterans with good or adequate health literacy level perceived their health status to be better than veterans with poor or inadequate health literacy. Using plain and simple language by providers while counseling patients about their disease and medications, might have a positive ripple effect on the current patient-centered care delivery. Clinicians could use a tailored approach to improve communication with patients.
Keywords: Veteran; Health literacy; Medication use; Numeracy skills; Self-perceived health status
Introduction
Health literacy is of great importance for clinicians to maximize patient involvement and in the effective delivery of healthcare services. Improving health literacy level is paramount, not only in the delivery of health care services, but is also necessary for patient comprehension of health-related topics and patient-centered care. To that effect, the promotion of adequate health literacy is a driving force for maintaining and promoting health. Factors influencing health literacy is of great interest for clinicians. Similarly, self-perceived health status (SPHS) is an important determinant of health status related to functional status, morbidity and mortality, and health-related quality of life (HRQOL).
Key determinant of healthcare costs and outcomes is health literacy. Adequate health literacy skills provide the means for effective health care delivery. National data shows patients with low health literacy have increased office visits, emergency room visits, and increased costs associated with those visits and prescription medications [1]. Low health literacy is also associated with negative health outcomes, including difficulty taking medications properly, issues understanding health messages, decreased use of preventative services, and increased hospitalizations [2].
In the Veteran Affairs (VA) population health literacy is of concern due to its unique population demographics. Most VA patients are older adult males. Low health literacy in older adults predicts reduced physical function, mental health, and increased mortality compared to those with adequate health literacy skills [2,3]. On average, VA veterans also have more chronic conditions than non-veterans and lower socioeconomic status than veterans not using VA care, further implicating concern [4].
Few studies have investigated the impact of health literacy on health outcomes in the veteran population. Haun et al. confirmed an inverse association between health literacy and healthcare utilization and spending in the veteran population mirroring general population trends [5]. Previous studies investigated the association between health literacy and intermediate measures such as medication adherence [6,7], adverse drug events, and patient-physician relationships [8] in the veteran population. To date, none focus on the relationship between health literacy and global health status in the veteran population. Self-perceived health status (SPHS) is an important determinant of health status related to functional status, morbidity and mortality, and health-related quality of life (HRQOL).
Therefore, the objective of this cross-sectional study is to evaluate factors associated with health literacy level in veterans with a focus on patient self-perceived health status (SPHS).
Methods
Study population
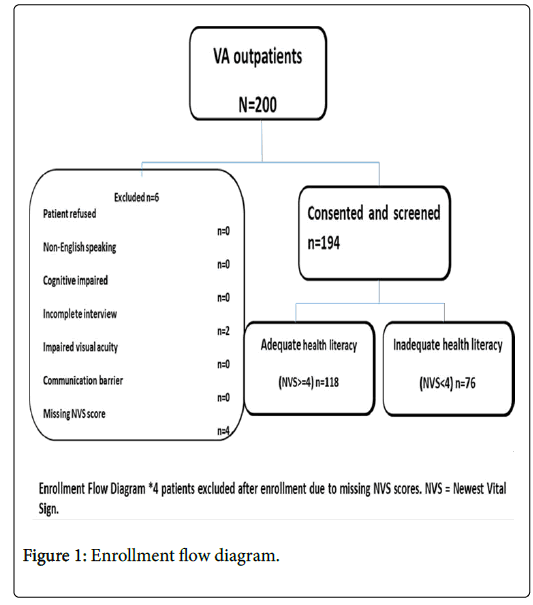
A total of 194 veterans receiving ambulatory care services at the Kansas City Veteran Affairs Medical Center (KCVAMC) were randomly selected and enrolled in this cross-sectional study. All consented participants were interviewed in-person. Newest Vital Sign (NVS) score was used to measure health literacy level. Veteran socio demographic, clinical characteristics, current medication use, and SPHS were measured. Recruitment and exclusion of study participants are shown in Figure 1.
Study protocol
This study was approved by the local VA Office of Research and Development (ORD) and reviewed by the VA Central Institutional Review Board and by the University of Kansas IRB. For each eligible and consenting patient, a research assistant administered all health literacy tests during the patient’s ambulatory visit. All screeners received standardized training on the administration of screening instruments, which consisted of an in-person presentation, practice sessions administering the instruments to mock patients, and monitored screening of the first patient. The screeners consisted of VA pharmacists, a pharmacist research assistant and a pharmacy professor. Training included specific instruction to avoid language that might lead patients to lean toward one response or the other. Screeners read participants standardized instructions for each of the health literacy screening instruments and recorded the start and stop times for all screening. Screening did not interfere with patient care. Screening could be continued after an interruption (laboratory or imaging studies, patient appointment time, etc.) provided, it was completed within a certain time frame. When present during screening, family members, caregivers or friends were asked not to assist with responses. The screeners carefully recorded all participant responses. Demographic data elements were collected during the interview. Missing demographic data and number of comorbidities, hospital admissions, and prescriptions was abstracted from the VA patient information portal, Computerized Patient Record System (CPRS).
Measures
Sociodemographic
Self-reported sociodemographic information included participant age, gender, race or ethnicity, education, and the number of different prescription medications taken daily.
Health literacy test: NVS
The screening tools administered included the Newest Vital Sign (NVS). The NVS is a validated, quick, and comprehensive health literacy screening tool. The NVS requires patients to answer 6 questions based on an ice cream nutrition label and assesses patient numeracy, comprehension, and abstract reasoning skills [9]. The assessment takes on average 3 minutes to administer. A score of 4 or greater (out of 6) indicates adequate health literacy; while a score less than 4 indicates possible limited health literacy (sensitivity 100%, specificity 64%) [9]. Compared to the other health literacy assessment tools Test of Functional Health Literacy in Adults (TOFHLA), Short Test of Functional Health Literacy in Adults (S-TOFHLA), Rapid Estimate of Adult Literacy in Medicine (REALM); NVS is the shortest test that includes a numeracy component, thus making it a suitable option in busy primary care settings [10].
Clinical characteristics and hospitalization status
VA’s electronic medical record portal, CPRS, was used to collect the number of different prescription medications veterans were taking at the time of the study. Co-morbidities reported in their charts were collected. We also reported if veterans were hospitalized in the last year and if they were living independently.
Analytical variable categorization
NVS was used to measure the patients’ health literacy level. Health literacy levels (dependent variable) were categorized into two groups: inadequate or adequate. SPHS (expressed as good or above and below good) was considered as an independent variable. Demographic and socioeconomic factors included: age-categorized as 18–24, 25–39, 40– 49, 50–59, 60–74, or greater than or equal to75 years; gendercategorized as male or female; race-categorized as white, black, American Indian/Alaska Native, Asian/Pacific Islander and Multiracial; income-categorized as poor/near poor, or low income, middle income, or high income; residence in a metropolitan area (MSA) or a non-metropolitan area (non-MSA); individual’s educational attainment - categorized as ‘still in high school’, ‘still in college/some college’, ‘less than high school’, ‘high school/GED (General Educational Development)’, and ‘bachelor’s degrees or higher’; marital status categorized as married, divorced/widowed/ separated, or never married; and language spoken at home - categorized as English or other; insurance types as private or public; living condition - categorized as ‘live independently’, ‘has help with IADL’ (Instrumental activities of daily); polypharmacy categorized as ‘less than 5 Prescription Medication (rx-meds)’ or ‘5 rx-meds or more’; number of hospitalization in past year as ‘yes’ or ‘no’; and number of co-morbidities as ‘less than 5 co-morbidities’ or ‘5 or more comorbidities’. All data were entered in a VB.Net program with a Microsoft Access (Microsoft Corp., Redmond, WA) as the backend database. The data was de-identified with each participant receiving a randomly generated unique identification number. Data was then exported to STATA statistical software for data analysis.
Data analyses
Health literacy levels (dependent variable) derived from NVS scoring rules were categorized into two groups: inadequate or adequate. SPHS (expressed as good or above and below good) was the independent variable. We ran a bivariate logistic regression (unadjusted) between health literacy level and each for the demographic and socioeconomic factors including SPHS. An adjusted logistic model was performed for health literacy level and SPHS with demographic and socioeconomic factors as covariates. All analyses were performed using STATA version 9 (College Station, TX).
Results
Our results document that of 194 participating veterans majority were male (90.2%), Caucasian (58.8%) and English-speaking (98.9%) with mean age of 57.8 years; Standard deviation SD ± 14.2. Less than half of these patients (40.2%) were married. Most of the patients evaluated (93.8%) live independently and 22.7% reported having at least a bachelor degree. Almost all participants (99%) reported speaking English at home and reported to be in middle income group (51.5%). Most of the patients (93.8%) lived in a MSA, geographical region with a relatively high population density at its core and close economic ties throughout the area.
Based on NVS, 40% of the veteran have possible limited or inadequate health literacy (score of <4). They were categorized as at risk for poor or inadequate health literacy for the purpose of this study. Based on SPHS, 57.2% of the veterans reported having good or above good SPHS. Two-thirds of patients (65.5%) were taking 5 or more medications (polypharmacy). Majority of these patients (84.5%) had 5 or more comorbidities (multi-morbidities). One fifth (24.2%) of these patients were hospitalized in the last year (Table 1).
| Characteristics | Health Literacy(NVS) | Total N (%) | |
|---|---|---|---|
| Inadequate | Adequate | ||
| Self-perceived health status | |||
| Below good | 37 (48.7) | 46 (39) | 83 (42.8) |
| Good or above | 39 (51.3) | 72 (61) | 111 (57.2) |
| Gender | |||
| Female | 4 (5.3) | 15 (12.7) | 19 (9.8) |
| Male | 72 (94.7) | 103 (87.3) | 175 (90.2) |
| Age | |||
| 18-24 | 0 (0) | 3 (2.5) | 3 (1.5) |
| 25-39 | 2 (2.6) | 23 (19.5) | 25 (12.9) |
| 40-49 | 2 (2.6) | 17 (14.4) | 19 (9.8) |
| 50-64 | 29 (38.2) | 38 (32.2) | 67 (34.5) |
| 65-74 | 35 (46.1) | 32 (27.1) | 67 (34.5) |
| 75+ | 8 (10.5) | 5 (4.2) | 13 (6.7) |
| Race | |||
| White | 37 (48.7) | 78 (66.1) | 115 (59.3) |
| Black | 36 (47.4) | 31 (26.3) | 67 (34.5) |
| Asian/Pacific Islander | 1 (1.3) | 2 (1.7) | 3 (1.5) |
| American Indian | 0 (0) | 2 (1.7) | 2 (1) |
| Multiracial | 2 (2.6) | 5 (4.2) | 7 (3.6) |
| Education level | |||
| Still in high school | 0 (0) | 2 (1.7) | 2 (1) |
| Still in college/some college | 9 (11.8) | 1 (0.8) | 10 (5.2) |
| Less than high school | 25 (32.9) | 26 (22) | 51 (26.3) |
| High school/GED | 29 (38.2) | 58 (49.2) | 87 (44.8) |
| Bachelor’s degrees or higher | 13 (17.1) | 31 (26.3) | 44 (22.7) |
| Income level | |||
| Poor/Near poor | 9 (11.8) | 10 (8.5) | 19 (9.8) |
| Low income | 30 (39.5) | 42 (35.6) | 72 (37.1) |
| Middle income | 35 (46.1) | 65 (55.1) | 100 (51.5) |
| High income | 2 (2.6) | 1 (0.8) | 3 (1.5) |
| Marital status | |||
| Married | 32 (42.1) | 46 (39) | 78 (40.2) |
| Never married | 11 (14.5) | 24 (20.3) | 35 (18) |
| Divorced/Widowed/Separated | 33 (43.4) | 48 (40.7) | 81 (41.8) |
| Language at home | |||
| English | 74 (97.4) | 118 (100) | 192 (99) |
| Other | 2 (2.6) | 0 (0) | 2 (1) |
| Insurance type | |||
| Any private | 30 (39.5) | 40 (33.9) | 70 (36.1) |
| Public only | 46 (60.5) | 78 (66.1) | 124 (63.9) |
| Living condition | |||
| Live independently | 69 (90.8) | 113 (95.8) | 182 (93.8) |
| Has help with IADL | 7 (9.2) | 5 (4.2) | 12 (6.2) |
| Rurality | |||
| MSA | 72 (94.7) | 110 (93.2) | 182 (93.8) |
| Non-MSA | 4 (5.3) | 8 (6.8) | 12 (6.2) |
| Polypharmacy | |||
| Less than 5 rx-meds | 22 (28.9) | 45 (38.1) | 67 (34.5) |
| 5 rx-meds or more | 54 (71.1) | 73 (61.9) | 127 (65.5) |
| Hospitalization status (in past year) | |||
| No hospital admission | 54 (71.1) | 93 (78.8) | 147 (75.8) |
| Hospital admission | 22 (28.9) | 25 (21.2) | 47 (24.2) |
| Number of comorbidities | |||
| Less than 5 co-morbidities | 10 (13.2) | 20 (16.9) | 30 (15.5) |
| 5 Co-morbidities or more | 66 (86.8) | 98 (83.1) | 164 (84.5) |
Table 1: Demographic and clinical characteristics of veterans who were screened by Newest Vital Sign (NVS) health literacy tool.
Bivariate analyses indicated that there was an association between health literacy and the demographic/socioeconomic factors. This was more significantly observed in patient age groups 50-64 years and 65-74 years. Veteran age group 50-64 years and 65-74 years were 90% and 93% less likely to have adequate health literacy level compared to patients aged 18-39, respectively (odds ratio [OR]=0.10 95% CI : 0.02 to 0.46 ; [OR]=0.07 95% CI: 0.02 to 0.32). Older individuals displayed poorer numeracy literary levels. This relationship stayed the same for patients above 75 years of age.
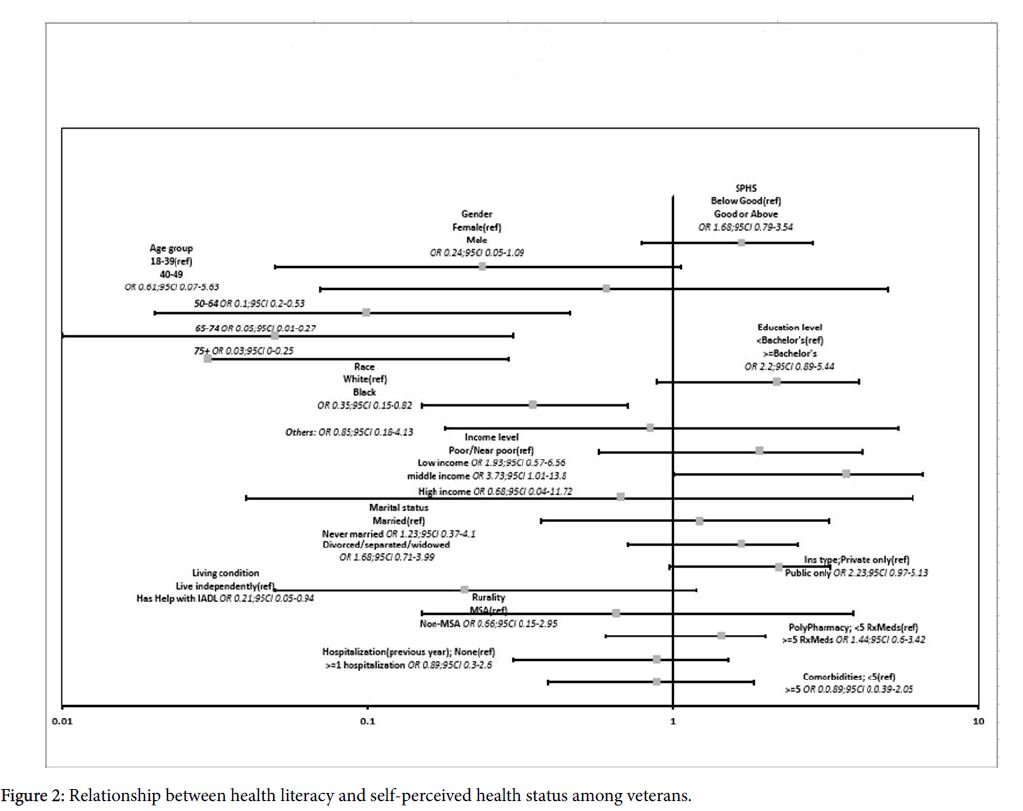
In unadjusted analysis, those with good or above SPHS had increased odds (odds ratio [OR]=1.48, 95% confidence interval [CI]: 0.83 to 2.66) of adequate health literacy skills compared with those with below good SPHS, however, the OR for adequate health literacy with SPHS was not statistically significant which was also seen after adjusted for covariates. (OR=1.68, 95% CI: 0.79 to 3.54) (Table 2). After adjusting for demographic and socioeconomic factors, the following results were obtained: veterans with bachelor degrees were 2.2 times more likely (OR=2.2, 95% CI: 0.89 to 5.44) to have adequate health literacy (Figure 1).
Veterans who had multiple chronic co-morbidities were 11% less likely (OR=0.89, 95% CI: 0.39 to 2.05) to have adequate health literacy compared to patients who had less than 5 co-morbidities. Although not statistically significant, veterans with polypharmacy (taking ≥ 5 meds) were 23% less likely to have adequate health literacy compared to veterans taking less than 5 medications.
Based on SPHS about 61% of good or above SPHS patients had good/adequate HLL which is 1.7 times higher (OR: 1.68, 95%CI=0.79 to 3.54) compared to patients with below good SPHS.
(Table 2 and Figure 2) Bivariate and multivariate analyses indicated that there was an inverse association between HLL and the demographic/socioeconomic factors. This was more significantly observed in patient age groups 50-64 years and 65-74 years. Figure 1 shows the odds ratios of HLL and SPHS after adjusted for demographic and socioeconomic factors.
| Self-Perceived Health Status(SPHS) | Unadjusted OR (95%CI) | Adjusted OR (95%CI) |
|---|---|---|
| Below Good | Reference | Reference |
| Good or above | 1.48 (0.83 to 2.66) | 1.68 (0.79 to 3.54) |
| Gender | ||
| Female | Reference | Reference |
| Male | 0.38 (0.12 to 1.20) | 0.24 (0.05 to 1.09) |
| Age | ||
| 18-39 | Reference | Reference |
| 40-49 | 0.65 (0.08 to 5.09) | 0.61 (0.07 to 5.63) |
| 50-64 | 0.10 (0.02 to 0.46) | 0.1 (0.02 to 0.53) |
| 65-74 | 0.07 (0.02 to 0.32) | 0.05 (0.01 to 0.27) |
| 75+ | 0.04 (0.01 to 0.3) | 0.03 (0 to 0.25) |
| Educational level | ||
| <Bachelor’s | Reference | Reference |
| ≥ Bachelor’s | 1.72 (0.84 to 3.56) | 2.2 (0.89 to 5.44) |
| Race | ||
| White | Reference | Reference |
| African american | 0.41 (0.22 to 0.77) | 0.35 (0.15 to 0.82) |
| Others | 1.60 (0.42 to 6.20) | 0.85 (0.18 to 4.13) |
| Income level | ||
| Poor/Near poor | Reference | Reference |
| Low income | 1.26 (0.46 to 3.48) | 1.93 (0.57 to 6.56) |
| Middle income | 1.67 (0.62 to 4.50) | 3.73 (1.01 to 13.8) |
| High income | 0.45 (0.03 to 5.84) | 0.68 (0.04 to 11.72) |
| Marital status | ||
| Married | Reference | Reference |
| Never married | 1.52 (0.65 to 3.53) | 1.23 (0.37 to 4.1) |
| Divorced/Widowed/Separated | 1.01 (0.54 to 1.90) | 1.68 (0.71 to 3.99) |
| Insurance type | ||
| Any private | Reference | Reference |
| Public only | 1.27 (0.70 to 2.31) | 2.23 (0.97 to 5.13) |
| Living condition | ||
| Live independently | Reference | Reference |
| Has help with IADL | 0.44 (0.13 to 1.42) | 0.21 (0.05 to 0.94) |
| Rurality | ||
| MSA | Reference | Reference |
| Non-MSA | 1.30 (0.32 to 4.51) | 0.66 (0.15 to 2.95) |
| Polypharmacy | ||
| Less than 5 rx-meds | Reference | Reference |
| 5 rx-meds or more | 0.66 (0.36 to 1.22) | 0.77 (0.37 to 1.64) |
| Readmission status(1 Year) | ||
| No hospital admission | Reference | Reference |
| Hospital admission | 0.66 (0.34 to 1.28) | 0.89 (0.3 to 2.6) |
| Number-of-co-morbidities | ||
| Less than 5 comorbidities | Reference | Reference |
| 5 Comorbidities or more | 0.74 (0.33 to 1.69) | 0.89 (0.39 to 2.05) |
| Adjusted model--includes demographics and socioeconomic factors (age, race, gender, education, income level, and marital status, living conditions, number of co-morbidities, polypharmacy and Rurality). CI, confidence interval; OR, odds ratio. | ||
Table 2: Unadjusted and adjusted models of the relationship between health literacy level and self-perceived health status (SPHS).
Discussion
Utilizing NVS we observed a relatively lower (60%) prevalence of veterans with good or adequate numeric health literacy compared to past studies utilizing S-TOFHLA and REALM assessment tools (60-85%). This discrepancy can be explained by the conceptual differences between NVS, S-TOFHLA, and REALM [11]. NVS emphasizes health numeracy skills, while S-TOFHLA and REALM mainly assess reading comprehension and analytical health literacy skills with little focus on health numeracy. We observed that older individuals displayed poorer numeracy literary levels. Studies utilizing S-TOFHLA have observed adequate health literacy rates in the 70-85% range [12,13]. In a cross-sectional study of 1,796 veterans from 4 large VA medical centers, 85.8% of veterans had adequate health literacy based on the S-TOFHLA assessment [14]. Adequate health literacy rates based on REALM have ranged from 60-80% [7,12,14,15]. Our results indicate 60% of veterans have adequate health literacy. Compared to other instruments, NVS is a unique problem-solving based assessment with high sensitivity. Thus, it may detect more cases of inadequate health literacy, but may also overestimate the prevalence in this population [9,16].
In a previous study, Rodriguez et al. (2013) administered NVS in an outpatient veteran population but found fewer veterans (45%) had adequate health literacy compared to our study (60%) [8]. This difference could likely be due to demographic differences between geographic regions. Rodriguez et al. conducted their study in a single VA medical center located in Miami, Florida in study population with more African Americans (55%) and Hispanics (19%) [8]. The study also found inadequate health literacy were more common in African Americans than White veterans. Miami’s larger African American population likely contributed to the health literacy level differences observed compared to our Midwestern veterans with white majority (58.8%).
Our study focuses on self-perceived health status, a surrogate indicator for overall health and quality of life. In our study veterans with good or above SPHS were 1.7 times more likely to have adequate health literacy compared to patients with below good SPHS, but this relationship was not statistically significant. Rodriguez et al. (2013) also reported a positive association between SPHS and health literacy skill, finding veterans with adequate health literacy were more likely to describe their health as “very good or excellent” (55%) compared to veterans with inadequate health literacy (45%) [8]. Overall, veterans with adequate health literacy level perceive their health status to be better than veterans with inadequate health literacy level.
Associations observed between HLL and patient demographic and socioeconomic factors coincided with those cited in the literature. In our study, a statistically significant inverse association was found between HLL and age, as well as health literacy and independence (requiring help with IADLs). Past studies in the VA population have found statistically significant associations between HLL and age, education, income, and race [8,12,13].
In addition, low HLL was associated with hospital admission and a higher number of medications (polypharmacy). Veterans who were hospitalized in the last year were 34% less likely (OR=0.66) to report adequate HLL compared to who did not report hospitalization. This association report was 11% less likely (OR=0.89) when adjusted for all demographic and clinical characteristics reported in our study (Table 2). In previous studies limited health literacy has been associated with poorer health, higher medical expenses, and increased hospitalization [1,17,18]. Limited health literacy has even been linked to increased mortality. In heart failure patients, patients with low health literacy have a 32% increased risk of death after discharge compared to patients with adequate health literacy [19].
Inadequate health literacy continues to affect VA patients. Prevalence rates have varied based on the health literacy assessment tool used. Because there no consensus yet on the best instrument, future studies should continue to assess health literacy with multiple instruments. The relationship between HLL results should be tested for association with indicators of overall health status, such as SPHS. Identifying the health literacy instrument most predictive of health outcomes in the VA population will help target subpopulations within the VA for health literacy interventions.
Adequate health literacy skills are necessary for patient comprehension of health information and provide the means for effective health care delivery. Veterans with adequate health literacy perceive their health status to be better than veterans with inadequate health literacy. Complicated by cognitive decline with age, many veterans will not have the basic health literacy skills needed to successfully manage their health conditions. These patients may also lack the numeracy skills, a component of health literacy, needed to understand lab values, take medications appropriately, or interpret risk probabilities [20]. Clinicians should recognize health literacy as an important determinant of health outcomes.
Practice Implications
Adequate health literacy skills are necessary for patient to comprehend health information for effective health care delivery. Clinicians should be vigilant in identifying patients with poor or inadequate HLL and must use a tailored approach to improve communication with patients. Health literacy driven health communication strategies, such as using plain simple medical language and utilizing teach-back techniques, may encourage appropriate and optimal use of healthcare resources and medications [1]. These techniques might have a positive ripple effect on the current patientcentered care delivery system.
NVS or other health literacy screening tools can be successfully incorporated into inpatient and primary care settings [21] to identify patients at risk. Baseline health literacy levels as part of the medical record may help clinicians to individualize patient interactions to achieve better health outcomes, including improved medication adherence, especially for underserved populations [18].
Clinicians should use plain and simple medical language that can be applied to veterans with varying literacy levels. For the older adult, simple strategies can be implemented to help patients improve cognitive function [22]. For all populations, strategies such as using plain simple medical language and utilizing teach-back techniques are recommended [23-25].
Conclusion
Veterans with good or adequate HLL perceived their health status to be better than veterans with poor or inadequate health literacy. Using plain and simple language by providers while counseling patients about their disease and medications might have a positive ripple effect on the current patient-centered care delivery system.
Limitations
Participants were English-speaking only (99%) and 90.2% were male. The predominance of males in the study was an accurate depiction of the veteran population. The participants in our study were drawn from two primary care VA outpatient clinics, which may affect the generalizability of the study. Future research is warranted to further investigate or establish the association or causal contributions of sociodemographic clinical factors to health literacy.
Funding
This study was funded by University of Kansas General Research Fund.
Acknowledgement
Amanda Peterson, PharmD for her help in data entry, Elaine Ogden, PharmD for her help in acquiring IRB approval through the Kansas City- Veteran Affairs (KC-VA) Institutional Review Board (IRB).
References
- Rasu RS, Bawa WA, Suminski R, Snella K, Warady B (2015) Health literacy impact on national healthcare utilization and expenditure. Int J Health Policy Manag 4: 747-755.
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K (2011) Low health literacy and health outcomes: An updated systematic review. Ann Intern Med 155: 97-107.
- Wolf MS, Gazmararian JA, Baker DW (2005) Health literacy and functional health status among older adults. Arch Intern Med 165: 1946-1952.
- Eibner C, Krull H, Brown KM, Cefalu M, Mulcahy AW, et al. (2016) Current and projected characteristics and unique health care needs of the patient population served by the department of veterans affairs. Rand Health Q 5: 13.
- Haun JN, Patel NR, French DD, Campbell RR, Bradham DD, et al. (2015) Association between health literacy and medical care costs in an integrated healthcare system: A regional population based study. BMC Health Serv Res 15: 249.
- Marzec LN, Carey EP, Lambert-Kerzner AC, Del Giacco EJ, Melnyk SD, et al. (2015) Cognitive dysfunction and poor health literacy are common in veterans presenting with acute coronary syndrome: Insights from the MEDICATION study. Patient Prefer Adherence 9: 745-751.
- Mosher HJ, Lund BC, Kripalani S, Kaboli PJ (2012) Association of health literacy with medication knowledge, adherence, and adverse drug events among elderly veterans. J Health Commun 3: 241-251.
- Rodriguez V, Andrade AD, Garcia-Retamero R, Anam R, Rodriguez R, et al. (2013) Health literacy, numeracy, and graphical literacy among veterans in primary care and their effect on shared decision making and trust in physicians. J Health Commun 1: 273-289.
- Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, et al. (2005) Quick assessment of literacy in primary care: The newest vital sign. Ann Fam Med 3: 514-522.
- Duell P, Wright D, Renzaho AM, Bhattacharya D (2015) Optimal health literacy measurement for the clinical setting: A systematic review. Patient Educ Couns 98: 1295-1307.
- Haun J, Luther S, Dodd V, Donaldson P (2012) Measurement variation across health literacy assessments: Implications for assessment selection in research and practice. J Health Commun 17: 141-159.
- Griffin JM, Partin MR, Noorbaloochi S, Grill JP, Saha S, et al. (2010) Variation in estimates of limited health literacy by assessment instruments and non-response bias. J Gen Intern Med 25: 675-681.
- Thrall D, Bent K (2005) Health literacy in the diabetes population at VA eastern colorado health care system.
- Chew LD, Griffin JM, Partin MR, Noorbaloochi S, Grill JP, et al. (2008) Validation of screening questions for limited health literacy in a large VA outpatient population. J Gen Intern Med 23: 561-566.
- Ravenell K, Asch D, Henry C, Fosnocht K, Murphy J, et al. (2002) Health literacy and patient satisfaction.
- Osborn CY, Weiss BD, Davis TC, Skripkauskas S, Rodrigue C, et al. (2007) Measuring adult literacy in health care: Performance of the newest vital sign. Am J Health Behav 1: S36-46.
- Ngoh LN (2003) Health literacy: A barrier to pharmacist-patient communication and medication adherence. J Am Pharm Assoc 49: e132-146.
- Sawkin MT, Deppe SJ, Thelen J, Stoner SC, Dietz CA, et al. (2015) Health literacy and medication adherence among patients treated in a free health clinic: A pilot study. Health Serv Res Manag Epidemiol
- McNaughton CD, Cawthon C, Kripalani S, Liu D, Storrow AB, et al. (2015) Health literacy and mortality: A cohort study of patients hospitalized for acute heart failure. J Am Heart Assoc 4: e000682.
- Rothman RL, Montori VM, Cherrington A, Pignone MP (2008) Perspective: The role of numeracy in health care. J Health Commun 13: 583-595.
- Cawthon C, Mion LC, Willens DE, Roumie CL, Kripalani S (2014) Implementing routine health literacy assessment in hospital and primary care patients. Jt Comm J Qual Patient Saf 40: 68-76.
- Park DC, Gutchess AH, Meade ML, Stine-Morrow EA (2007) Improving cognitive function in older adults: Nontraditional approaches. J Gerontol B Psychol Sci Soc Sci 62: 45-52.
- Agency for Healthcare Research and Quality (2010) AHRQ health literacy universal precautions toolkit (2nd edn).
- Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, et al. (2003) Closing the loop: Physician communication with diabetic patients who have low health literacy. Arch Intern Med 163: 83-90.
- Weiss BD, Brega AG, LeBlanc WG, Mabachi NM, Barnard J, et al. (2016) Improving the effectiveness of medication review: Guidance from the health literacy universal precautions toolkit. J Am Board Fam Med 29: 18-23.
Citation: Rasu R, Bawa WA, Anna Hu, Sharma R, Stanke A, et al. (2018) Evaluation of Health Literacy in Veteran Affairs Outpatient Population: A Focus on Patient Self-Perceived Health Status. J Community Med Health Educ 8: 613. DOI: 10.4172/2161-0711.1000613
Copyright: © 2018 Rasu R, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 8363
- [From(publication date): 0-2018 - Dec 06, 2025]
- Breakdown by view type
- HTML page views: 7274
- PDF downloads: 1089