Evaluation of the Vestibular Aqueduct and the Retrolabyrinthine Region by High Resolution Computed Tomography in Patients with Unilateral Ménière’s Disease
Received: 17-Jan-2019 / Accepted Date: 06-Feb-2019 / Published Date: 14-Mar-2019 DOI: 10.4172/2161-119X.1000360
Abstract
Objectives: To systematize the anatomical study of the vestibular aqueduct using high resolution computed tomography (HRCT) and to evaluate the retrolabyrinthine region in patients with unilateral Ménière’s disease (MD).
Methods: The vestibular aqueduct is one of the most studied labyrinth structures in the genesis of endolymphatic hydrops and has a possible anatomic and physiological role in this disease. Twenty patients with unilateral Ménière’s disease and ten normal patients (control group) underwent HRCT of temporal bones. In total 60 ears were analyzed, 20 of them in each of the following groups: GI (ear affected by MD), GII (MD group - ear not affected), GIII (control). The images were analyzed blindly. The vestibular aqueduct was identified and the measurements were acquired in its middle portion and in the external opening. The retrolabyrinth dimension was also measured in these patients. These findings were analyzed and compared between these groups.
Results: The vestibular aqueduct was identified in the ears of 95% of GI, 90% of G II and 100% of G III, and measurements of the width of the middle portion and external opening of vestibular aqueduct were analyzed and showed no statistical difference between the three groups. The retrolabyrinthine dimension was similar between groups G I and G II, but significantly higher in G III (G I=G II<G III).
Conclusion: It is possible to apply the proposed systematization for the evaluation of the vestibular aqueduct by HRCT. The identification and measurement of vestibular aqueduct width did not show statistically significant differences between affected (GI) and unaffected (GII) ears of patients with Ménière’s disease, nor in relation to the control group (GIII). The retrolabyrinthine dimension was significantly higher in the control group (GIII) compared to that of GI and GII
Keywords: Vestibular aqueduct; Temporal bone; Meniere’s disease; Retrolabyrinthine dimension; High resolution computed tomography ; Endolymphatic hydrops; Ear
Introduction
The etiology and pathogenesis of Ménière’s disease (MD) are not yet fully understood. The vestibular aqueduct (VA) is one of the most studied labyrinth structures, with an anatomical and physiological role supposedly important in the genesis of hydrops. It consists of a bony tunnel that contains the duct and part of the endolymphatic sac [1], where the endolymph is absorbed [2].
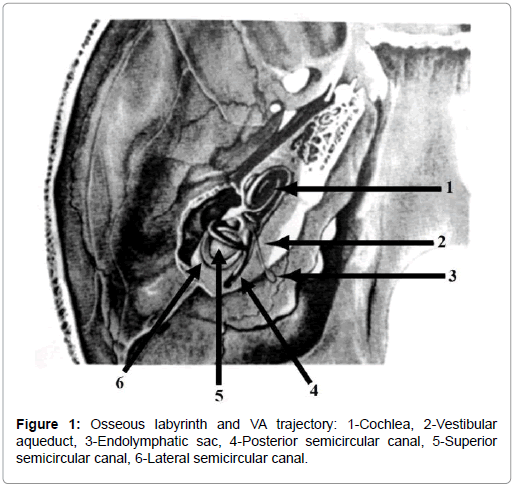
The proximal VA portion opens into the medial wall of the vestibule and travels medially and posteriorly to the otic capsule, close to the medial portion of the common crura, which is a useful marker for its radiological identification. A few millimeters down its trajectory, it forms a pronounced curve, followed by a rectified course in the inferior and posterior direction, until it meets medial and posterior opening of the petrous bone, between the internal acoustic pore and the sigmoid groove (Figure 1). The perilabyrinthine pneumatization reflects the area of the retrolabyrinth where the endolymphatic sac is located.
In the last 60 years, endolymphatic sac surgery has been revitalized and widely used in order to facilitate endolymph drainage. Consequently, VA imaging studies have gained tremendous interest, albeit having been the subject of much controversy. Efforts to correlate the radiological visualization and shape of VA with the etiology, diagnosis and treatment of MD have led to confusing and conflicting results. Some authors have described the high incidence of non-radiological visualization and/ or narrowing of VA [2-15] and mastoid with poor pneumatization in patients with MD [4-6,13-18], however other authors considered these radiological observations as non-specific signs seen in a variety of otological diseases and even in normal ears [19,20].
Despite the relevant number of publications correlating VA and Ménière’s disease, there is still no agreement as to the best way to study it. In addition, there is great difficulty in comparing the results of these works due to non-standardization of technique and radiological interpretation.
Thus, this study was designed with the intention of applying the anatomical study of VA using high resolution computed tomography (HRCT) [21] and evaluating the retrolabyrinthine region in patients with unilateral Ménière’s disease and comparing with normal individuals (Figure 1).
Methods
This was an observational cross-sectional study that twenty patients with unilateral Ménière’s disease were selected from the outpatient clinic of Otology and Otoneurology of the Hospital São Paulo, according to the criteria proposed by the American Academy of Otolaryngology - Head and Neck Surgery [22] and with the ratio of summating potential/ action potential of equal or greater action to 35% (SP/AP ≥ 35%) in the electrocochleography test (EcoG) [23]. They were submitted to clinical otorhinolaryngological evaluation, complete otoneurological evaluation, including audiometric tests, electronystagmography (ENG) and bilateral (transthympanic) EcoG.
We selected 10 individuals without auditory or balance complaints, without history of chronic otitis, without exposure to noise or use of ototoxic drugs and with normal audiometric evaluation to compose the control group.
The study was approved by the Ethics Committee of the School of Medicine-Federal University of São Paulo, no. 0081/04. Subjects and patients were invited to participate in the study, and those that accepted and passing all criteria were included and signed a consent form and formally joined the study.
Our sample consisted of 30 subjects who underwent HRCT of temporal bones to evaluate the inner ear. The images were acquired using a spiral technique, Somatom Balance, Siemens, with supine position, orbitomeatal axial plane of 1.0/0.5 mm thickness/increment, 512 × 512 matrix, 135 mAs, 130 kVp, FOV of 180 mm, pitch of 1,5, bone filter, reading performed with window/level of 4,000/600 Hounsfield units. The study of the images was blinded to disease or control groups and was systematized for evaluation of the posterior labyrinth.
The image evaluation was done by two radiologists and one otorhinolaryngologist, and consisted of consensus categorization or averages of measurements of the following aspects of the posterior labyrinth and the post-isthmic segment of VA:
1. VA visualization or non-visualization: when VA was not visible in its middle portion was considered not visible.
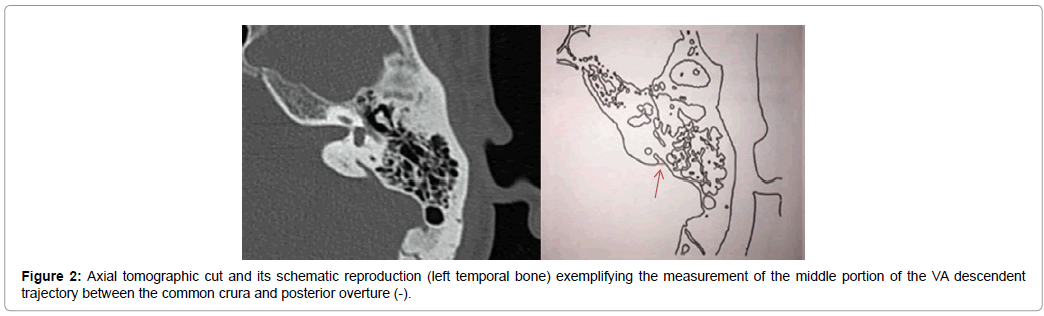
2. Measurement of the middle portion of descending path of the VA: for the measurement of the VA descending middle portion, we identified the common crura (superior and posterior semicircular canal) and this cut was considered the first cut of interest, and the last cut of interest was in which the external opening was identified. We counted the number of cuts in this interval and the measurement was made in the middle cut. The measurement of the width of the middle portion of the VA lumen in its downward path, between the common crura and external aperture, was performed by moving the digital slider from medial to lateral (Figure 2).
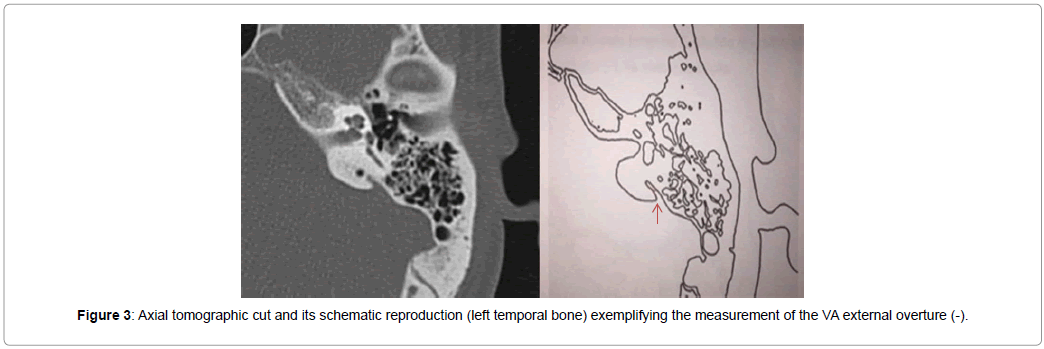
3. Measurement of the external diameter of the VA opening: the external aperture was measured at its greatest diameter (medial to lateral) (Figure 3).
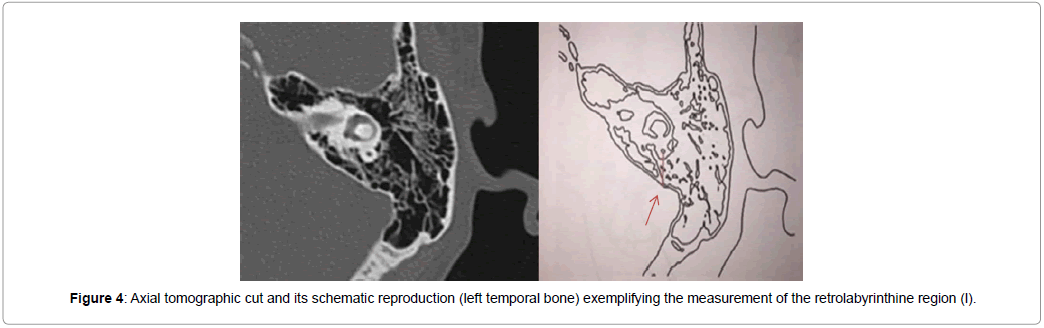
4. Measurement of the size of the retrolabyrinthine region: it was defined by the smaller distance between the lumen of the posterior semicircular canal and the posterior surface of the temporal bone [12] (Figure 4).
5. All measurements were obtained in millimeters, and assigned to each corresponding group.
Results
In the Ménière’s disease group, women (n=16) predominated, age ranged from 31 to 82 years, with a mean of 52 years. The period of illness or related complaints ranged from one to 30 years (mean=19 years and 6 months). In the control group, six individuals were female and four were males, the age ranged from 24 to 37 years and the mean age was 28 years.
Sixty ears were studied, constituting three groups:
Group I (GI): 20 ears with MD; Group II (GII): 20 contralateral ears of patients with unilateral MD; Group III (control - GIII): 20 normal ears.
The ANOVA test, with a significance level of 5%, standard deviations were calculated for each group. The analysis of VA visualization in the three groups is expressed in Table 1.
| Vestibular aqueduct | Group I N (%) | Group II N (%) | Group III N(%) | Total N(%) |
|---|---|---|---|---|
| Identified Non identified |
19 (95) 1 (5) |
18 (90) 2 (100) |
20 (100) 0 (0) |
57 (95) 3 (5) |
| Total | 20 (100) | 20 (100) | 20 (100) | 60 (100) |
Table 1: Analysis of the vestibular aqueduct visualization in groups I, II and III.
The VA visualization was superior to 90% in all groups, and the small number of non-visualized cases made it impossible to apply a statistical test.
The middle portion of the descending VA path (width) is shown in Table 2.
| Width of VA middle portion | Group I | Group II | Group III |
|---|---|---|---|
| Average (mm) | 0.78 | 0.74 | 0.68 |
| Standard deviation (mm) | 0.35 | 0.18 | 0.16 |
| Total (n) | 17 | 16 | 19 |
ANOVA-level of significance F (p)=0.471
Table 2: Mean and standard deviation of the VA portion (width).
The external opening could not be identified in one GI patient and two GII patients. There was no significant difference between the groups regarding the measurement of VA opening diameter (p=0.593).
The evaluation of the retrolabyrinthine dimension is shown in Table 3.
| Retrolabyrinthine dimension. | Group I | Group II | Group III |
|---|---|---|---|
| Average (mm) | 2.58 | 3.33 | 4.69 |
| Standard deviation (mm) | 1.75 | 1.58 | 2.62 |
| Total (n) | 20 | 20 | 20 |
ANOVA-F (p)=0.006.
Table 3: Retrolabyrinthine dimension.
There was a significant difference between the groups regarding the measurement of the retrolabyrinthine dimension (p=0.006). By multiple comparisons the following hierarchy was observed: GI=GII<GIII. Groups I and II (MD) had lower values than group III (control), that is, control individuals had a larger dimension of the retrolabyrinthine region.
ANOVA-level of significance F (p)=0.471 (Table 3).
Discussion
The roles that VA size and shape, and the size of the retrolabyrinthine region play in the pathogenesis of hydrops is still discussed. These parameters were studied in many patients with MD, but without conclusive results. In this study, the VA was systematically evaluated to define the capacity of its visualization. We measured the dimensions of the descending portion and its external aperture. We also measured the size of the retrolabyrinthine region to evaluate the development of the mastoid in the ears affected and not affected by MD and control individuals.
There are many controversies in the literature [3-18,24,25] regarding the visualization of VA in Ménière’s disease using CT, or even HRCT, and the studies do not allow us many comparisons because there is no systematization of the study protocols. Since 1973, with the introduction of CT, this technology has been improving at an accelerated pace, allowing better visualization of smaller structures. In HRCT, it is possible to study anatomic details in a resolution as high as 0.5 mm. For this reason, we proposed to systematize the study of VA by HRCT and then to study the descending pathway of the VA and the retrolabyrinthine region of the temporal bone in the three groups (I, II, III). We were able to conclude that it is possible to systematize HRCT for evaluation of VA, with axial acquisition, using the same radiological technique, anatomical knowledge and sequential follow-up of the inner ear structures [21].
There is no specific radiological signal for Ménière’s disease [16]. The non-visualization of VA is described in other pathological conditions (such as chronic otitis media) and in normal ears [19,20].
Another questionable aspect refers to using the width of the VA, which is also not standardized, to define what is narrow or widened, making it difficult to compare studies. We propose in another work [21] a systematization for acquiring measurements.
The retrolabyrinthine dimension allows evaluation of the development and pneumatization of the mastoid [23], and it is also discussed in the literature [4-6,8,13,17,18,24,26,27]. This dimension is significantly reduced in MD, and this was observed in our study, both in the affected ear and in the ear not affected by MD, when compared to that of normal individuals. This alteration seems to suggest that the reduced perilabirinthine pneumatization, with the consequent reduction of the size of the retrolabyrinthine area, where the endolymphatic sac is located, may have some contribution to the pathogenesis of the hydrops, but it still constitutes a non-specific image signal for MD.
Imaging evaluation has a limited clinical interest in Ménière’s disease. Only the size of the retrolabyrinthine region would be relevant in the cases selected for surgical treatment. The molecular basis may play an important role in the pathogenesis of hydrops.
With the advent of endolymphatic hydrops imaging, the magnetic resonance imaging (MRI), three-dimensional fluid-attenuated inversion recovery (3D-FLAIR), besides of the sequence weighting highlights differences in the T2 relaxation time of tissues (T2 WI) and their relationship with electrophysiological test should be considered in follow-up the Meniere Disease patients in future longitudinal study.
Conclusion
1) It is possible to apply the proposed systematization for the evaluation of the VA by HRCT.
2) The identification and measurement of VA width did not show statistically significant differences between the affected (GI) and unaffected (GII) ears of patients with Ménière’s disease, nor of the control group (GIII).
3) The retrolabyrinthine dimension was significantly higher in the control group (GIII) than in the GI and GII groups.
Imaging evaluation has a limited clinical interest in Ménière’s disease. Only the size of the retrolabyrinthine region would be relevant in the cases selected for surgical treatment. Thus, changes at the molecular level in the production and absorption of endolymph appear to play a more relevant role in the pathogenesis of hydrops than any anatomical changes.
References
- Anson BJ, Donaldson JA, Warpeha RL, Winch TR (1964) Surgical anatomy of the endolymphatic sac and perilymphatic duct. Laryngoscope 74: 480-497.
- Sennaroglu L, Yilmazer C, Basaran F, Sennaroglu G, Gursel B (2001) Relationship of vestibular aqueduct and inner ear pressure in Ménière’s disease and the normal population. Laryngoscope 111: 1625-1630.
- Clemis JD, Valvassori GE (1968) Recent radiographic and clinical observation on the vestibular aqueduct. Otolaryngol Clin North Am 1: 339-352.
- Arenberg IK, Portmann G, Shea JJ Jr, Shambaugh GE Jr (1976) Review of the pathophysiologic mechanisms of Ménière’s disease and correlation with clinical diagnosis and therapy. Rev Laryngol Otol Rhinol (Bord) 97: 399-409.
- Xenellis J, Vlahos L, Papadopoulos A, Nomicos P, Papafragos K, et al. (2000) Role of the new imaging modalities in the investigation of Meniere's disease. Otolaryngol Head Neck Surg 123: 114-119.
- Yazawa Y, Kitahara M (1994) Computerized tomography of the petrous bone in Menière's disease. Acta Otolaryngol Suppl 510: 67-72.
- De Groot JA, Huizing EH, Damsma H, Van Waes PF, Zonneveld FW (1986) Computed tomography of the petrous bone in otosclerosis and Menière's disease. Acta Otolaryngol Suppl 434: 1-135.
- Stahle J, Wilbrand H (1974) The vestibular aqueduct in patients with Menière's disease. A tomographic and clinical investigation. Acta Otolaryngol 78: 36-48.
- Wilbrand HF, Stahle J, Rask-Andersen H (1978) Tomography in Menière's disease--why and how. Morphological, clinical and radiographic aspects. Adv Otorhinolaryngol 24: 71-93.
- Valvassori GE, Clemis JD (1978) The large vestibular aqueduct syndrome. Laryngoscope 88: 723-728.
- Austin DF (1981) Polytomography in Ménière's disease: An update. Laryngoscope 91: 1669-1675.
- Rumbaugh CL, Bergeron T, Scanlan RL (1974) Vestibular aqueduct in Meniere's disease. Radiol Clin North Am 12: 517-525.
- Nidecker A, Pfaltz CR, Matéfi L, Benz UF (1985) Computed tomographic findings in Ménière’s disease. ORL J Otorhinolaryngol Relat Spec 47: 66-75.
- Miyashita T, Toyama Y, Inamoto R, Mori N (2012) Evaluation of the vestibular aqueduct in Ménière's disease using multiplanar reconstruction images of CT. Auris Nasus Larynx 39: 567-571.
- Krombach GA, van den Boom M, Di Martino E, Schmitz-Rode T, Westhofen M, et al. (2005) Computed tomography of the inner ear: Size of anatomical structures in the normal temporal bone and in the temporal bone of patients with Menière's disease. Eur Radiol 15: 1505-1513.
- Wilbrand HF (1976) Menière's disease-roentgenologic diagnosis. Arch Otorhinolaryngol 212: 331-337.
- Dauphin D, Laffont J, Garand G, Reynaud J (1981) Menière's disease, petrous bone tomography. A new radiographic sign? Neuroradiology 22: 15-18.
- Han L, Jing YY, Yu LS, Xia RM (2013) Development of the mastoid air cells and its relationship to Ménière's disease. Zhonghua Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 48: 135-138.
- Oigaard A, Thomsen J, Jensen J, Dorph S (1975) The narrow vestibular aqueduct. An unspecific radiological sign? Arch Otorhinolaryngol 211: 1-4.
- Kraus EM, Dubois PJ (1979) Tomography of the vestibular aqueduct in ear disease. Arch Otolaryngol 105: 91-98.
- Alvarenga EHL, Cruz OLM, Yamashita HK, de Lima EJ, Alvarenga AM, et al. (2006) Systematization of vestibular aqueduct anatomical study by high-resolution computed tomography in patients with unilateral Ménière’s disease. Radiol Bras 39: 345-349.
- Committee on Hearing and Equilibrium (1995) Committee on hearing and equilibrium guidelines for the diagnosis and evaluation of therapy in Ménière’s disease. Otolaryngol Head Neck Surg 113: 181-185.
- Munhoz MSL (2001) Sensibility and specificity of transtympanic eletrocochleography in patients with and without endolymphatic hydrops. Dissertation Universidade Federal de São Paulo.
- Hall SF, O’Connor AF, Thakkar CH, Wylie IG, Morrison AW (1983) Significance of tomography in Ménière’s disease: Periaquedutal pneumatization. Laryngoscope 93: 1551-1553.
- Takeda T, Sawada S, Kakigi A, Saito H (1997) Computed radiographic measurement of the dimensions of the vestibular aqueduct in Ménière’s disease. Acta Otolaryngol Suppl 528: 80-84.
- Dimopoulos PA, Smedby Ö, Wilbrand HF (1996) Anatomical variations of the human vestibular aqueduct. Part II. A radioanatomical study. Acta Radiol 37: 33-41.
- Castagno LA (1987) Anatomy of the temporal bone in Ménière’s disease. Folha Méd 95: 341-343.
Citation: Alvarenga EHL, Dall’Oglio GP, Yamashita HK, do Vale NABS, Cruz OLM (2019) Evaluation of the Vestibular Aqueduct and the Retrolabyrinthine Region by High Resolution Computed Tomography in Patients with Unilateral Ménière’s Disease. Otolaryngol (Sunnyvale) 9:360. DOI: 10.4172/2161-119X.1000360
Copyright: © 2019 Alvarenga EHL, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4375
- [From(publication date): 0-2019 - Dec 17, 2025]
- Breakdown by view type
- HTML page views: 3439
- PDF downloads: 936