Extended Open Partial Laryngectomy with Titanium-Based Laryngeal Framework Reconstruction: Surgical Technique and Treatment Outcomes
Received: 03-Oct-2017 / Accepted Date: 24-Oct-2017 / Published Date: 31-Oct-2017 DOI: 10.4172/2161-119X.1000327
Abstract
Objective: To present surgical technique and treatment outcomes after extended open partial laryngectomy with titanium-based laryngeal framework reconstruction performed on 8 patients with T2-T3 squamous cell cancer of larynx.
Method: To evaluate respiratory, phoniatric and swallowing function of larynx, titanium plate tolerance and cancer treatment outcomes 3 years after used operating procedure.
Results: The procedure was uneventful and the airflow through the reconstructed part of the larynx was undisturbed in all cases. The titanium plate ensured airway patency and was well tolerated, except for one case, where it was explanted due to proliferation of granulation tissue on the skin over the plate. The anterior wall did not collapse following device explantation. Phoniatric evaluation demonstrated no social impact of patient vocal handicap. 5 patients reported mild vocal disability and 3 moderate vocal disabilities in the Voice Handicap Index. None of them developed dysphagia. Most patients reported high and very high swallowing-related quality-of-life in the M.D. Anderson Dysphagia Inventory (mean score of 79). Complete laryngectomy was performed in 2 patients due to local recurrence and cervical lymphadenectomy with subsequent radiotherapy was performed in 1 patient due to regional recurrence.
Conclusion: Extended open partial laryngectomy with titanium-based laryngeal framework reconstruction may be one of way of treatment of intermediate-stage laryngeal cancer, especially with a limited endoscopic access to the tumor or suspected thyroid cartilage infiltration, which preserves physiological laryngeal function. This cancer stage is an indication for complete laryngectomy, so the procedure represents organ sparing approach
Keywords: Squamous cell carcinoma; Open partial laryngectomy; Laryngeal framework reconstruction; Titanium prosthesis; Sternothyroid muscle flap
Introduction
Squamous cell carcinoma of the larynx constitutes 48% of all malignant head and neck cancers, excluding skin cancer [1-5]. In Poland, it accounts for approximately 2.7% of overall cancer morbidity in males and 0.4% in females [6]. Most cases originate in the glottis and the risk in males is eight times as high as in females [1-4].
Current trends in laryngeal surgery involve organ-sparing approaches, which do not impair it basic physiology, preserving the respiratory, phonation and swallowing function [2,3,6-13]. Such approach can be safely assumed when planning endoscopic laser, open partial laryngectomy or radiotherapy [1,4,7-15]. Treatment choices depend on the presence of local and regional tumor spread and its distant metastases [1,11]. In early tumors, clinical efficacy of surgery is comparable to the one of radiotherapy. However, radiotherapy cannot be repeated, so the surgery, which can be used as monotherapy or as a part of combined treatment, for instance followed by subsequent radiation therapy, appears a reasonable alternative [1-3,11].
There are many different types of open partial laryngectomies. We can divide them into two main groups: vertical partial laryngectomies (VPL) and open partial horizontal laryngectomies (OPHL) [1,4,5,11,14,16-18]. There are different types of reconstructions for different types of tumor localizations. The Sedlacek-Kambic-Tucker epiglottic reconstruction after vertical partial laryngectomy or are those of the most complicated examples [2,14-16].
Laryngeal reconstruction should restore laryngeal framework stability, undisturbed airflow and epithelial regrowth. It should also ensure sufficient speech quality, while not causing dysphagia [7,19]. Titanium and titanium alloys are currently the most commonly used prosthetic material in medicine. Apart from the ENT surgery, they are well known in general surgery, orthopaedics or maxillofacial surgery [20-27]. Such widespread use of titanium can be attributed to its favorable mechanical properties, corrosive resistance, biocompatibility and biotolerance [7,28]. Titanium laryngeal framework prostheses can be a valuable alternative in patients undergoing extended open partial laryngectomies for intermediate-stage laryngeal cancers with suspected thyroid cartilage infiltration [7].
Extended open partial laryngectomies undergone in our clinic are hard to classify. They are combinations of different types of laryngectomies and possible reconstructions. Different pieces of larynx are removed in case of cancer infiltrations. Patients with indications to total laryngectomy have opportunities to preserve larynx.
Materials and Methods
Extended open partial laryngectomy with laryngeal framework reconstruction using titanium plates was performed in 8 patients with squamous cell carcinoma of the larynx treated in our Department in 2014. 2 females and 6 males aged 62-78 years old (mean age of 63 years) were enrolled in the study Tumor size assessment with biopsy specimen collection for histological diagnosis and staging were carried out during the direct laryngoscopy at baseline. Additionally, contrastenhanced computed tomography of the neck and cervical ultrasound were performed in all cases in order to determine potential local and regional tumor spread. All tumors were stage T2-T3 according to AJCC with a risk of thyroid cartilage infiltration. Functional assessment was carried out 3 years after the surgery (Table 1).
| Characteristics | HNSCC patients | Local Recurrence patients | Regional Recurrence patients | |||
|---|---|---|---|---|---|---|
| n=8 | (%) | n=2 | (%) | n=1 | (%) | |
| Sex | ||||||
| Male | 6 | 75 | 2 | 25 | 0 | 0 |
| Female | 2 | 25 | 0 | 0 | 1 | 12,5 |
| Age | ||||||
| Range | 62-78 | |||||
| Median | 62.00 | |||||
| Tumor site | ||||||
| Larynx and hypopharynx | 8 | 100 | ||||
| Oral cavity | 0 | 0 | ||||
| Clinicopathological characteristics | ||||||
| Tumor size | ||||||
| T1 | 0 | 0 | ||||
| T2 | 3 | 37.5 | ||||
| T3 | 5 | 62.5 | ||||
| T4 | 0 | 0 | ||||
| Tumor differentiation | ||||||
| G1 | 2 | 25 | ||||
| G2 | 3 | 37.5 | ||||
| G3 | 3 | 37.5 | ||||
| Nodal involvement | ||||||
| N+ | 1 | 12,5 | ||||
| N- | 0 | 0 | ||||
| Treatment | ||||||
| Tumour resection | 7 | 87.5 | ||||
| Tumour resection+neck dissection | 1 | 12.5 | ||||
| Total laryngectomy | 2 | 25 | ||||
| Radiotherapy | 1 | 12.5 | ||||
| Stage | ||||||
| I | 0 | 0 | ||||
| II | 7 | 87.5 | ||||
| III | 1 | 12.5 | ||||
| IV | 0 | 0 | ||||
Table 1: Clinicopathological characteristics c with primary tumours as well as genders and ages and recurrence group.
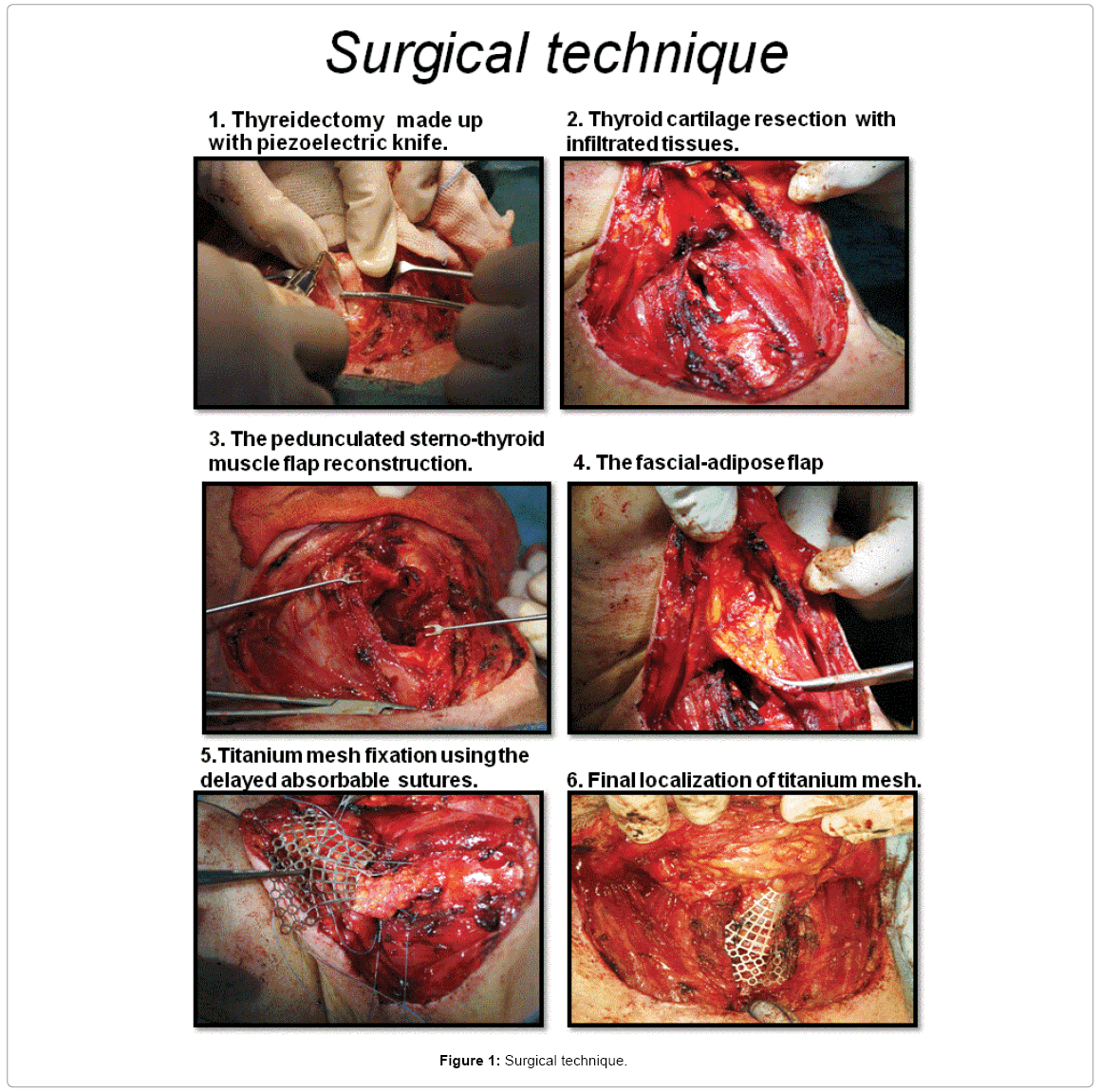
Surgical technique (Figure 1)
Extended open partial laryngectomy with laryngeal framework reconstruction using titanium plates under general anaesthesia was performed in all patients. The Gluck Sorenson U-shaped incision was preferred, with the symmetrical incision line starting a few cm below the mastoid process and extending along the anterior insertion of the sternocleidomastoid muscle. The layer-by-layer dissection was carried out, so as to create the musculocutaneous flap, involving skin, subcutaneous tissue, platysma muscle and its supplying blood vessels. Lifting the flap exposes prelaryngeal muscles, which are then moved to sides exposing the anterior wall of the larynx. Next, the perichondrium covering the thyroid cartilage laminae is dissected and pushed aside.
The aim is to preserve intact perichondrium on the lateral and posterior aspects of the thyroid cartilage. A vertical cut to the thyroid cartilage is made using the Carlo di Giorgi piezoelectric knife. The design of this cut depends on tumor location. The larynx is accessed along the median or paracentral line, contralateral to the tumor location. Laryngeal cartilage leaflets are pushed aside using Guthrie hooks. As a result, laryngeal lumen is exposed which ensures its thorough macroscopic assessment. Owing to the piezoelectric knife design it is possible to remove a preselected fragment of thyroid cartilage of any shape, together with the adjacent tumor mass. In case of cancer infiltration epiglottis, true vocal cords, ventricles, false vocal cords, arytenoids cartilages or subglottic area could be removed (Table 2). The created tissue defect is then reconstructed using the thyrohyoid muscle flap. It is essential that the muscle flap be harvested with the largest possible amount of perimysium. The muscle fragment prepared that way is then sutured onto the inner surface of the larynx. Matrix MIDFACE Orbital Floor Mesh Plate 0.2 mm porous malleable titanium prosthesis Synthes, Switzerland is used for laryngeal framework reconstruction. Prosthesis shape is tailored to fit the laryngeal anatomy of a given patient. The rectangular titanium plate is formed to match the shape of laryngeal framework and attached to the margins of the preserved thyroid cartilage using the delayed absorbable sutures. Thyroid cartilage resection may concern even almost whole thyroid cartilage. In order to ensure its proper function, the reconstructed laryngeal framework must be isolated from the lumen of the larynx. Therefore, the musculoadipose flap is prepared from the previously created musculocutaneous flap. It is inserted under the titanium laryngeal framework prosthesis thus creating a barrier between the laryngeal lumen and the prosthesis, which prevents granulation tissue formation later on. Due to the extensive tissue excision and potential postoperative oedema a tracheotomy is typically performed in all patients. It should be accomplished through a separate incision, so as to minimise potential gateway for implant infection. If accomplished through the same incision, it should be well separated from the implanting site. Later, passive wound drains are inserted, followed by wound closure using single subcutaneous and skin sutures. Finally, the compression dressing is placed on the postoperative wound.
| TUMOUR SITE | RESECTED TISSUES | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| NO. OF PATIENTS |
1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 |
| REGION OF LARYNX | ||||||||||||||||
| Epiglottis | - | + | - | - | - | - | - | - | - | + | - | - | - | - | - | - |
| Pre-epiglottis area | + | + | + | + | - | + | + | - | + | + | + | + | + | + | + | + |
False Vocal Cord
|
+ | + | + | + | + | + | + | - | + | + | + | + | + | + | + | - |
Ventricle
|
+ | + | + + |
+ | + + |
+ | + | + | + | + | + + |
+ | + + |
+ | + | + |
True Vocal Cord
|
+ | - | + + |
+ | + + |
+ | + | + | + | - | + + |
+ | + + |
+ | + | + |
| Anterior commissure | + | - | + | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Posterior commissure | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - | - |
Arytenoid area
|
+ | - | - | + | + | + | + | - | + | - | - | + | + | + | + | - |
| Subglottic area | - | - | - | - | - | + | - | - | - | - | - | - | - | + | - | - |
Table 2: Tumour site and resection rage.
Laryngeal functional assessment
Respiratory function: The reconstructed vocal fold and airway patency were assessed at 1 month following primary surgery. Laryngeal framework and unobstructed airflow, mucous membranes with potential inflammatory granulation tissue and the structure of the pseudocord was assessed using Kleinsasser suspension laryngoscope.
Voice function: Phoniatric assessment was carried out in all patients. It involved laryngostroboscopy using the Storz 70° rigid laryngoscope with digital image recording using the PC. Due to the nature of the disease and received treatment, it was impossible to fully assess the vocal folds. Instead, phoniatric assessment focused on oscillatory amplitude, marginal shift and oscillation regularity as compared to the healthy vocal cord. Furthermore, voice recording and its acoustic analyses were performed using the IRIS software developed by the students of Wroclaw Technical University. In order to perform an objective acoustic analysis of vocal fold phonation, the laryngeal tone was analysed upon producing the long a vowel [a:]. Using the IRIS software, vocal parameters were assessed, such as frequency perturbation parameters (Jitter, RAP, PPQ), voice amplitude (Schimmer, APQ) and the Noise to Harmonic Ratio (NHR), which is a relative noise parameter. With a patient producing long a vowel (a:), their voice acoustic intensity (decibels, dB) and maximum phonation time (seconds, s) were measured. Additionally, phonation was assessed using self-reported Pruszewicz-modified Voice Handicap Index (VHI), which consists of questions relative to the three domains of patient life: functional, emotional and physical. The functional scale reflects the effect of voice disorder on the quality of professional and social life. The emotional scale assesses patient feelings regarding their voice disorder. Finally, the physical scale makes it possible to ascertain physical symptoms associated with the partial loss of speech organ. The VHI consists of 30 items with patient circling the most accurate of the 5 possible options. Each item scores 0-4 points, with ‘never’ scoring 0 and ‘always’ scoring 4 points. The maximum achievable score is 120. The patients were classified into one of three groups according to their scores, with the score of 0 considered to be normal voice, scores of 1 to 30 considered mild vocal handicap, scores of 31-60 considered moderate vocal handicap and 61-120 considered severe vocal handicap.
Swallowing function: Swallowing function was assessed using the fiberoendoscopic examination of the swallow (FEES). During the procedure, the patients were instructed to swallow liquid, semi-liquid and solid foods to assess the swallowing process using the Fujinon, System 2200 Processor video fiberoscope Fujijon, Japan. The test foods included Braunoldyed saline, Nutri-Drink and cottage cheese. In line with Donzelli’s scoring reduced to 3-point-scale, the patients were classified into one of the three groups: 1) Pooling in vallecula or pyriform, 2) Laryngeal penetration of secretions above true vocal cords or 3) Secretions on true vocal cords and/ or tracheal aspiration. Additionally, swallowing function was assessed using the M.D. Anderson Dysphagia Inventory (MDADI), which is a subjective, patient self-reported swallowing assessment instrument. In this 20-item questionnaire the patient chooses the response option which reflects their swallowing problem in the most accurate manner. Each item is scored with 1-5 points, with ‘strongly agree’ scoring 1 and ‘strongly disagree’ scoring 5 points. The maximum achievable score is 100. Based on their scores, the patients are classified as having severe (0-40), moderate (41-60) or mild (60-100) dysphagia.
Cancer treatment outcomes: Local tumour spread was assessed using direct laryngoscopy one month following surgery and during subsequent video fiberoscopy procedures. 2 patients underwent total laryngectomy due to local recurrence. Regional tumor spread was assessed with cervical ultrasound performed every three months. 1 patient underwent cervical lymphadenectomy and subsequent radiotherapy due to regional recurrence.
Results
Uneventful surgical procedure was carried out in all cases. In treeyear follow up, a successful decannulation was successfully performed in all patients by the end of month 3 postoperatively.
Respiratory function
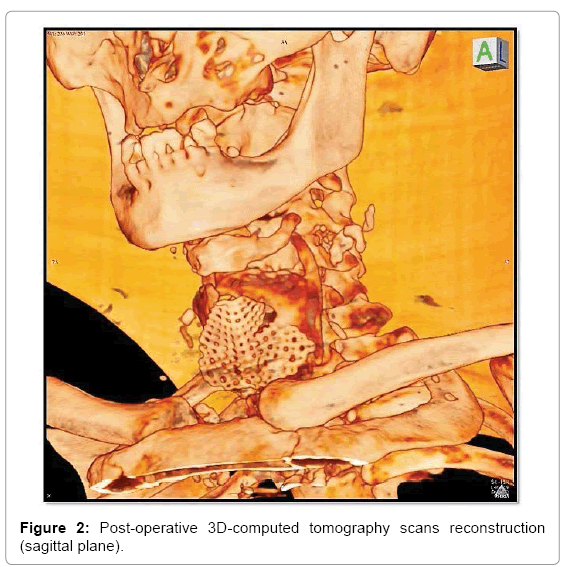
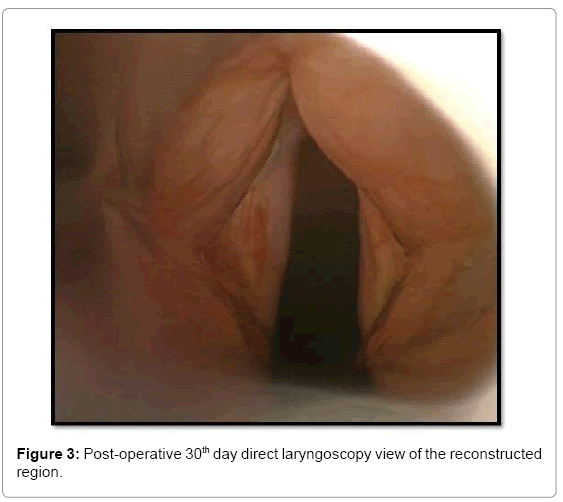
During the assessment at one month following surgery and subsequent video endoscopies performed over an average follow-up of 3 years, no airflow disturbance through the upper respiratory tract or signs of allergy to titanium used for reconstruction were shown. No stenosis, acute inflammation or intralaryngeal granulation tissue was seen at the implantation site. The titanium laryngeal framework prosthesis had to be explanted in one case due to granulation tissue growth on the overlying skin. The anterior wall did not collapse following prosthesis explantation and the airway patency was preserved. Titanium prosthesis served as laryngeal framework expander. The remaining patients still live with the prosthesis in place (Figure 2). The pseudocord reconstructed using the sternothyroideus flap resembled the actual vocal fold in structure (Figure 3).
Voice function
In patients after extended open partial laryngectomy, voice is generated between the pseudocord reconstructed using the pedunculated sternothyroideus flap and the true vocal fold. Positioning the pseudocord opposite the true vocal fold enables proper apposition during phonation. It is difficult to compare the symmetry of oscillation between the true vocal fold and the pseudocord, due to the inability of the latter to oscillate independently. Patients with good adduction and apposition of voice-generating surfaces achieved significantly better voice quality. Except for asymmetry, the healed reconstructed pseudocord did not appear substantially different from the true vocal cord in macroscopic visualisation. Only after stroboscopic light was used, the nil-phonation of the implanted flap could have been visualised. Postoperative voice quality was considered good with patients frequently not needing any voice rehabilitation. The video laryngostroboscopy revealed full occlusion at phonation in 5 patients, as compared to semioccluded phonation in 3 cases, where the non-occlusion was seen in a part of the glottis. The maximum phonation time was 10-15 s (median 12 s). Acoustic intensity for whisper fell into the range of 25-40 dB, for normal speech - of 40-50 dB and for shout - of 30-60 dB. The mean values of acoustic analyses of laryngeal tone when producing long a vowel (a:) were as follows: F0 110 Hz, Jitter 1.5%, RAP 1.0%, PPQ 1.01%, Shimmer 10.1% APQ 6.03% and NHR 18% (Table 3). In the study selftest failures voice (Pruszewicz- modified Voice Handicap Index) mild vocal handicap had 3 patients, moderate vocal handicap had 5 patients and no one had severe vocal handicap (Table 4).
| Phoniatric Examination | ||||
|---|---|---|---|---|
| Occlusion at Phonation | ||||
| Total | 5 | |||
| Non-total | 3 | |||
| Maximum Phonation Time (seconds) | Operated Patients Scores | Average Standard Scores | ||
| Range | 10-15 s | 20-30 s | ||
| Median | 12 s | 25 s | ||
| Acoustic Intensity (dB) | ||||
| Whisper | 25-40 dB | 50-55 dB | ||
| Normal speech | 40-50 dB | 60-65 dB | ||
| Shout | 30-60 dB | 80-87 dB | ||
| The Mean Values of Acoustic Analyses of Laryngeal Tone When Producing Long a Vowel a: | Operated Patients Scores | Average Standard Patients Scores | ||
| Women | Men | |||
| F0 | 110 Hz | 250 Hz | 120 Hz | |
| Jitter | 1.50% | 0.9% | 0.8% | |
| RAP | 1.00% | 0.3% | 0.2% | |
| PPQ | 1.01% | 0.4% | 0.4% | |
| Shimmer | 10.10% | 4.7% | 4.2% | |
| APQ | 6.03% | 4.7% | 4.5% | |
| NHR | 18% | 8.1% | 7.9% | |
Table 3: The results phoniatric examination.
| The results of the study self-test failures voice (Pruszewicz-modified Voice Handicap Index) | |
|---|---|
| Score | Number of patients (%) |
| 0-30 mild vocal handicap | 3 (37.5%) |
| 31-60 moderate vocal handicap | 5 (62.5%) |
| 61-120 severe vocal handicap | 0 (0%) |
Table 4: The results of the study self-test failures voice (Pruszewicz-modified Voice Handicap Index).
Swallowing function
We did not observe dysphagia when swallowing solid, semi-liquid or liquid foods during FEES in of 7 our patients, whom we considered to be Donzelli’s score 1. In 1 case, Donzelli’s score 3 dysphagia was present when swallowing liquids, which was not confirmed when swallowing semi-liquid or solid foods (score 1) (Table 5). Assessed with MDADI, most patients were found to have very high swallowing-related qualityof- life (Table 6). Their MDADI scores were 77, 77, 78, 79, 79, 80, 80 and 82, respectively, with the mean score of 79.
| The results of the Donzelli's score dysphagia | |||
|---|---|---|---|
| Test Food Score |
Number of patients (%) | ||
| Braunol-dyed saline | Nutri-Drink | Cottage cheese | |
| 1 Pooling in vallecula or pyriform |
7 (83%) | 8 (100%) | 8(100%) |
| 2 Laryngeal penetration of secretions above true vocal cords |
0 (0%) | 0 (0%) | 0 (0%) |
| 3 Secretions on true vocal cords and/or tracheal aspiration |
1 (17%) | 0 (0%) | 0 (0%) |
Table 5: The results of the Donzelli's score dysphagia.
| The results of the M.D. Anderson Dysphagia Inventory (MDADI scale) |
|
|---|---|
| Score | Number of patients (%) |
| 0-40 Severe dysphagia |
0 (0%) |
| 31-60 Moderate dysphagia |
0 (0%) |
| 61-100 Mild dysphagia |
8 (100%) |
Table 6: The results of M.D. Anderson dysphagia inventory.
Cancer treatment outcomes
2 patients (2 males) underwent total laryngectomy due to local recurrence. 1 patient (1 female) underwent cervical lymphadenectomy and subsequent radiotherapy due to regional recurrence. Patient noncompliance (by smoking or alcohol abuse) was confirmed in all cases of recurrence (Table 1).
Discussion
The first attempts to perform laryngeal reconstruction using titanium prosthesis were made our Department in the 1990’s, when the available titanium devices were thick and poorly malleable. Our first patient, who had a 2 mm thick titanium device implanted due to postoperative laryngeal stenosis, is still alive, with his titanium device in place. In a 20 year follow-up, we have not observed device intolerance. It provided optimum laryngeal framework support and acted as an expander, preventing recurrent stenosis, ensuring airway patency and good respiratory function. Currently, the development of medical technology has allowed for the titanium elements to be manufactured in any shape, size, thickness and with improved medical properties. The literature search yields several reports of titanium-based airway reconstruction and their functional outcomes [7,29-31].
Schultz et al. performed a histological analysis of titanium tolerance following laryngeal reconstruction in rats and confirmed good mechanical stability, negligible inflammatory response as well as good tissue proliferation and vascularisation of explanted titanium prostheses [29]. Similarly, histological evaluation of explanted titanium prosthesis in one of our patients showed its good tolerance, with effective tissue proliferation into the prosthesis and the absence of inflammatory tissue. Furthermore, it was stable enough to ensure proper laryngeal framework in the absence of natural thyroid cartilage. This confirms the findings by Schultz et al. [29] who argue that titanium prostheses make good long-term restoration material for upper respiratory tract reconstruction.
Balasubramanian et al. reported cricoid cartilage reconstruction using a pedunculated radial forearm flap and a titanium plate following thyroid cancer resection. They achieved good functional outcomes with patent airways, showing only a minimum risk of plate exposure and rejection by the host, due to biointegration of titanium with adjacent tissues, which we confirmed in our patients [31].
Yanagihara et al. used Nitinol for treating tracheal stenosis in patients with invasive tracheal cancer. They confirmed that the selfexpanding titanium and nickel alloy stent offered high flexibility and durability, sufficient to preserve the primary shape of the reconstructed organ. Additionally, they noticed that titanium structure prevented tumor proliferation into the prosthesis [32]. This was not confirmed by our findings, since our patients with cancer recurrence presented with malignant infiltrations involving the titanium prosthesis.
Liu et al. described the reconstruction technique using titanium mesh after frontolateral vertical partial laryngectomy in selected cases of T2-T3 glottic cancer, which resembles ours the most. All their patients had preserved respiratory function with some dysphonia and without dysphagia. No local or regional recurrence observed in the long-term follow up and titanium was assessed as good prosthetic material for laryngeal framework reconstruction [7]. Our technique, however, additionally involves separation of titanium prosthesis from the laryngeal lumen using the fasciocutaneous flap, which minimises the risk of granulation tissue formation with subsequent postoperative stenosis. Furthermore, using the piezoelectric knife improves surgical precision, since it is possible to remove any shape of thyroid cartilage. Titanium prosthesis is then fitted individually to match the laryngeal defect, which ensures its appropriate reconstruction. Finally, our patients have pseudofold reconstruction performed routinely in order to improve postoperative QoL through better phonation.
Conclusion
Extended open partial laryngectomy with titanium-based laryngeal framework reconstruction is a good treatment of intermediate-stage laryngeal cancer, especially with a limited endoscopic access to the tumor or suspected thyroid cartilage infiltration, which offers optimum functional outcomes. This cancer stage is an indication for total laryngectomy, so the procedure represents organ sparing approach and offers the patients preserved laryngeal function. Thin titanium plates, porous and malleable enough to be fitted individually to match the laryngeal defect, enable successful laryngeal framework reconstruction.
Conflict of Interest
All authors certify that they have NO affiliations with or involvement in any organization or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements) or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial or not for-profit sectors.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
References
- Chawla S, Carney AS (2009) Organ preservation surgery for laryngeal cancer. Head Neck Oncol 1: 12.
- Succo G, Crosetti E, Bertolin A, Lucioni M, Arrigoni G, et al. (2016) Benefits and drawbacks of open partial horizontal laryngectomies, Part B: Intermediate and selected advanced stage laryngeal carcinoma. Head Neck 38: E649-E657.
- Succo G, Crosetti E, Bertolin A, Lucioni M, Caracciolo A, et al. (2016) Benefits and drawbacks of open partial horizontal laryngectomies, Part A: Early- to intermediate-stage glottic carcinoma. Head Neck 38: E333-E340.
- Gilbert RW, Goldstein DP, Guillemaud JP, Patel RS, Higgins KM, et al. (2012) Vertical partial laryngectomy with temporoparietal free flap reconstruction for recurrent laryngeal squamous cell carcinoma: Technique and long-term outcomes. Arch Otolaryngol Head Neck Surg 138: 484-491.
- Marchese-Ragona R, Marioni G, Chiarello G, Staffieri A, Pastore A (2005) Supracricoid laryngectomy with cricohyoidopexy for recurrence of early-stage glottic carcinoma after irradiation. Long-term oncological and functional results. Acta Otolaryngologica 125: 91-95.
- Kawecki A, Nawrocki S (2013) Nowotwory nablonkowe narzadów glowy i szyi. In: Krzakowski M, Warzocha K (eds.) Zalecenia postepowania diagnostyczno-terapeutycznego w nowotworach zlosliwych 2013 rok. Gdansk: Via Medica. Arch Int Physiol Biochim, pp: 1-32.
- Liu XK, Zhang Q, Li Q, Liu WW, Li H, et al. (2010) Laryngeal framework reconstruction using titanium mesh in glottic cancer after frontolateral vertical partial laryngectomy. Laryngoscope 120: 2197-2202.
- Marioni G, Marchese-Ragona R, Lucioni M, Staffieri A (2008) Organ-preservation surgery following failed radiotherapy for laryngeal cancer. Evaluation, patient selection, functional outcome and survival. Curr Opin Otolaryngol Head Neck Surg 16: 141-146.
- Olsen KD, DeSanto LW (1990) Partial vertical laryngectomy--indications and surgical technique. Am J Otolaryngol.11: 153-160.
- Piquet J, Piquet JJ (1963) Indications for partial vertical laryngectomy. Lille Chir 18: 208-212.
- Yeager LB, Grillone GA (2005) Organ preservation surgery for intermediate size (T2 and T3) laryngeal cancer. Otolaryngol Clin North Am 38: 11-20, vii.
- Schindler A, Pizzorni N, Fantini M, Crosetti E, Bertolin A, et al. (2016) Long-term functional results after open partial horizontal laryngectomy type IIa and type IIIa: A comparison study. Head Neck 38: E1427-E1435.
- Ratajczak J, Wojtowicz P, Krzeski A (2014) Estimation of quality of voice after removal of neoplasms T1 and T2 of glottis with simultaneous reconstruction of vocal fold with pedunculated sterno-thyroid muscle flap. Otolaryngol Pol 68: 258-263.
- Leroux-Robert J (1957) Conservative surgery of laryngeal cancer by laryngofissure or partial laryngectomy. Fulorrgegegyogyaszat, pp: 49-61.
- Brumund KT, Gutierrez-Fonseca R, Garcia D, Babin E, Hans S, et al. (2005) Frontolateral vertical partial laryngectomy without tracheotomy for invasive squamous cell carcinoma of the true vocal cord: A 25 year experience. Ann Otol Rhinol Laryngol 114: 314-322.
- Wein RO, Weber RS (2005) The current role of vertical partial laryngectomy and open supraglottic laryngectomy. Curr Probl Cancer 29: 201-214.
- Woo P (1990) Laryngeal framework reconstruction with miniplates. Ann Otol Rhinol Laryngol 99: 772-777.
- Succo G, Peretti G, Piazza C, Remacle M, Eckel HE, et al. (2014) Open partial horizontal laryngectomies: A proposal for classification by the working committee on nomenclature of the European Laryngological Society. Eur Arch Otorhinolaryngol 271: 2489-2496.
- Liu B, Pan ZM, Ji WY (2005) Reconstruction of laryngeal defect in vertical partial laryngectomy with resection of arytenoid cartilage. Zhonghua er bi yan hou tou jing wai ke za zhi. Chin J Otorhinolaryngol Head Neck Surg 40: 52-55.
- Tarsitano A, Battaglia S, Ciocca L, Scotti R, Cipriani R, et al. (2016) Surgical reconstruction of maxillary defects using a computer-assisted design/computer-assisted manufacturing-produced titanium mesh supporting a free flap. J Craniomaxillofac Surg 44: 1320-1326.
- Sane VD, Kadam P, Jadhav A, Saddiwal R, Merchant Y (2016) Multidisciplinary approach for reconstruction of cranial defect with polymethyl methacrylate resin reinforced with titanium mesh. J Indian Prosthodont Soc 16: 294-297.
- Sakat MS, Kilic K, Altas E, Gozeler MS, Ucuncu H. (2016) Comminuted frontal sinus fracture reconstructed with titanium mesh. J Craniofac Surg 27: e207-e208.
- Lizio G, Mazzone N, Corinaldesi G, Marchetti C (2016) Reconstruction of extended and morphologically varied alveolar ridge defects with the titanium mesh technique: Clinical and dental implants outcomes. Int J Periodontics Restorative Dent 36: 689-697.
- Dai J, Shen G, Yuan H, Zhang W, Shen S, et al. (2016) Titanium mesh shaping and fixation for the treatment of comminuted mandibular fractures. J Oral Maxillofac Surg 74: 337.e1-337.e11.
- Akkas Y, Peri NG, Kocer B, Kaplan T (2016) Repair of lung herniation with titanium prosthetic ribs and prolene mesh. Asian Cardiovasc Thorac Ann 24: 280-282.
- Abdeen K. (2016) Efficacy of titanium mesh cages for anterior column reconstruction after thoracolumbar corpectomy. Asian Spine J 10: 85-92.
- Otero-Rivas MM, Gonzalez-Sixto B, Alonso-Alonso T, Perez-Bustillo A, Valladares-Narganes LM, et al. (2015) Titanium mesh in reconstructive surgery of the nasal pyramid. Follow-up of our 11 initial cases. Int J Dermatol 54: 961-965.
- Przekora A, Benko A, Nocun M, Wyrwa J, Blazewicz M, et al. (2014) Titanium coated with functionalized carbon nanotubes--a promising novel material for biomedical application as an implantable orthopaedic electronic device. Mater Sci Eng C Mater Biol Appl 45: 287-296.
- Schultz P, Vautier D, Chluba J, Marcellin L, Debry C (2002) Survival analysis of rats implanted with porous titanium tracheal prosthesis. Ann Thorac Surg 73: 1747-1751.
- Yener M, Acar GO, Cansiz H, Oz B, Cigerciogullari E, et al. (2010) Use of titanium mesh in laryngotracheal reconstruction: An experimental study on rabbits. Eur Arch Otorhinolaryngol 267: 1247-1253.
- Balasubramanian D, Thankappan K, Shetty S, Jayaprasad K, Mathew J, et al. (2013) Cricotracheal reconstruction with free radial forearm flap and titanium mesh. Head Neck 35: E178-180.
- Yanagihara K, Mizuno H, Wada H, Hitomi S (1997) Tracheal stenosis treated with self-expanding nitinol stent. Ann Thorac Surg 63: 1786-1789.
Citation: Wójtowicz P, Jurek-Matusiak O, Ratajczak J, Krzeski A (2017) Extended Open Partial Laryngectomy with Titanium-Based Laryngeal Framework Reconstruction: Surgical Technique and Treatment Outcomes. Otolaryngol (Sunnyvale) 7:327. DOI: 10.4172/2161-119X.1000327
Copyright: © 2017 Wójtowicz P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 6377
- [From(publication date): 0-2017 - Aug 30, 2025]
- Breakdown by view type
- HTML page views: 5374
- PDF downloads: 1003