High Incidence of Non-Union Following Arthrodesis of the First Metatarsophalangeal Joint
Received: 29-Apr-2018 / Accepted Date: 22-May-2018 / Published Date: 29-May-2018 DOI: 10.4172/2329-910X.1000269
Abstract
Background: Non-union is a complication after arthrodesis of the first metatarsophalangeal joint (MTP-1). The reported incidence varies from 0 to 12%. However, we suspected the incidence might be higher in our clinic. The purpose of this study was to determine the incidence of non-union after MTP-1 arthrodesis.
Methods: In a retrospective cohort study, all patients that underwent primary MTP-1 arthrodesis between January 2015 and December 2016 were analysed.
Results: 89 toes were included among 84 patients. The cohort consisted of 63 females and 26 males with an average age of 60. The incidence of non-union was 23.5%. No significant differences in means of hallux valgus angle (HVA), age, smoking habits, ASA classification, gender, screw length, surgery duration, the number of bony cortices involved in the fixation, position of the screw intersection, fixation technique, articular surface preparation and the attending surgeon were found.
Conclusion: The incidence of non-union following MTP-1 arthrodesis is substantially higher compared to previously reported numbers in literature. No cause regarding the latter was identified. In an attempt to reduce the incidence of non-union, we have recently adjusted our treatment protocol and surgery techniques.
Keywords: Metatarsophalangeal joint; Arthrodesis; Joint fusion; Non-union; Hallux disorders; Hallux rigidus; Hallux valgus
Introduction
Arthrodesis of the first metatarsophalangeal joint (MTP-1) is a commonly performed treatment of patients suffering from disorders of the hallux including hallux rigidus, severe hallux valgus, rheumatoid arthritis, neuromuscular instability and as a possible salvage procedure for failed aligning treatments [1,2]. MTP-1 arthrodesis can be performed using a wide range of varying techniques regarding articular surface preparation and the fixation method [2].
The preparation of the articular surface can be performed either by using planar cuts of the bone ends or by using convex-concave reaming both of which can be done by using either hand instruments or power tools [2]. Manual cartilage removal has also been described. The convex-concave technique is increasing in popularity despite the lack of difference in biomechanical stiffness between the two methods [3-6]. A recent systematic review by Korim et al. showed better clinical outcome when hand instruments like curettes or rongeurs were used instead of power tools in the preparation of the articular surface [2]. Several fixation methods have been described for MTP-1 arthrodesis. These include: staple fixation, single-screw fixation, crossed-screw fixation and fixation using locked or non-locked plates. Biomechanical studies have identified dorsal plating in combination with a lag screw as the most stable fixation [7-10]. However, Korim et al. demonstrated no difference regarding the clinical outcome of either of these earlier mentioned fixation methods [2].
The reported incidence of union following MTP-1 arthrodesis ranges from 88% to 100% [2]. However, due to the previously mentioned heterogeneity in study populations regarding both the indication and the surgical technique there is no general consensus on the optimal surgical technique. Reported incidence of non-union following arthrodesis for hallux valgus is higher than for hallux rigidus (7% and 3.7% respectively) [2,11,12]. However, incidence of non-union after MTP1 arthrodesis was felt to be higher at our hospital, despite a standardized and intended evidence-based approach. Retrospectively we analysed the incidence of non-union following MTP-1 arthrodesis to identify its possible risk factors as to improve our treatment protocol and reduce the incidence of non-union after MTP-1 arthrodesis.
Patients and Methods
We aimed to identify the incidence and risk factor of non-union following primary MTP-1 arthrodesis. Non-union was defined as local pain, movement in the MTP-1 joint during clinical assessment and radiological signs of non-union (radiolucency/osteolysis, hardware failure and migration). When delayed union was established, the duration of cast immobilisation was extended before considering revision surgery. All patients who underwent primary MTP-1 arthrodesis, for osteoarthritis (rigid and painful MTP-1 joint, combined with radiological signs of osteoarthritis (joint space narrowing, sclerosis, osteophytosis and subchondral cysts) or severe hallux valgus (severe valgus deformity of the MTP-1 joint, defined as HVA>40°) in our clinic between January 2015 up to December 2016 were retrospectively identified. No patients were lost to follow up. All patients could be identified: 84 patients and 89 toes underwent MTP-1 arthrodesis, all MTP-1 fixations were performed using either crossed screws (Figure 1) or locked plate fixation (pedofix®) depending on the surgeon’s preference.
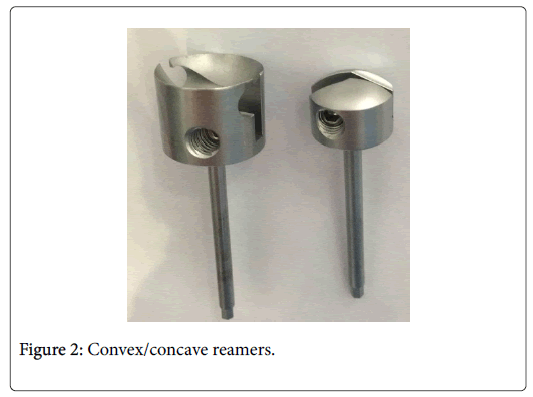
7 different surgeons preformed the operations during this period. Preparation of the articular surface was performed using either motorized convex/concave reamers (Figure 2), an oscillating saw for cutting planar saw planes or manually using curettes. Aftercare involved a standardized protocol which consisted of 6 weeks of weight bearing mobilization in a hallux-cast protecting the fused MTP-1 joint. Follow-up consisted of an outpatient control after 2 weeks, to remove the stitches and to apply a new halluxabductioncast, and after 6 weeks for clinical and radiological evaluation of the fusion. Patients were assessed using standardized follow-up intervals of 6 weeks to clinically and radiographically assess union of the arthrodesis. Compliance regarding cast immobilization and weight bearing was good. From medical records we registered anthropometric data, American Society of Anaesthesiologists (ASA) classification, smoking, articular surface preparation method, fixation method, surgeon, screw length, pre and postoperative hallux valgus angle (HVA), the number of cortices involved in cortical screw fixation and positioning of the screw intersection. These data were assessed as secondary outcome measures for their association with non-union. The incidence of non-union was the primary outcome measure.
Statistical analysis
All data was processed in SPSS (SPSS version 23.0 Inc. Chicago, IL, USA) for statistical analysis. Descriptive statistics were used to summarize the data. Distributed data are presented as mean with standard deviation. For assessment of possible cause-effect relationships between non-union and the previously mentioned risk factors, we created 2 subgroups: Joint with hallux rigidus or hallux valgus as primary diagnosis. We used an independent samples t-test and the Pearson chi-square test to assess whether any of the previously hypothesized risk factors differed significantly among patients with and without union. Differences were considered statistically significant with a P-value less than 0.05.
Results
In the years 2015 and 2016 a total of 88 (63 women and 25 men) patients underwent primary MTP-1 arthrodesis in our clinic. The average age was 61 ranging from 36 to 80 years. Please refer to Table 1 for demographic details on the study cohort.
| Statistics | Hallux Rigidus (n=70) | Hallux Valgus (n=18) | Total |
|---|---|---|---|
| Female (%) | 49 (70%) | 14 (78%) | 63 (72%) |
| Male (%) | 21 (30%) | 4 (22%) | 25 (28%) |
| Smoking (%) | 14 (20%) | 0 (0%) | 14 (16%) |
| Age, Std. Error, Range | 62, 1.0, 42 – 80 | 56, 2.6, 36 – 78 | 61, 1.0, 36 – 80 |
| HvA; SE.; Range | 23.8; 1.4; 6.8 – 56 | 43.6; 1.0; 33.3 – 50 | 28.9; 1.4; 6.8 – 56 |
| ASA-1 | 15 (21%) | 6 (33%) | 21 (24%) |
| ASA-2 | 50 (71%) | 12 (67%) | 62 (71%) |
| ASA-3 | 4 (6%) | 0 (0%) | 4 (5%) |
| ASA-4 | 1 (1%) | 0 (0%) | 1 (1%) |
Table 1: Descriptive statistics.
Radiographic union occurred in 77.3% of joints, thereby making the incidence of non-union 22.7%. 3 patients experienced an asymptomatic non-union in a single joint, thereby yielding an overall success rate of 80.1%. The incidences of non-union in subgroups of joints that underwent surgery for hallux rigidus of hallux valgus were 22.9% and 22.1% respectively. Pearson Chi-square test showed no significant difference regarding the incidence of non-union between these subgroups (p=0.954). Most joint fusions were fixated by using 2 screws (Table 2).
| Diagnosis | Joint surface preparation | Fixation method | ||||
| Convex/Concave | Planar cuts | Curette | 2 Screws | Locked plate | Lag-screw + plate fixation | |
| Rigidus | 52 (74%) | 9 (13%) | 9 (13%) | 67 (96%) | 2 (3%) | 1 (1%) |
| Valgus | 18 (100%) | 0 (0%) | 0 (0%) | 18 (100%) | 0 (0%) | 0 (0%) |
Table 2: Distribution of fixation and joint surface preparation methods over the primary diagnosis.
Pearson chi-square testing of the entire cohort showed no significant difference regarding the fixation method (p=0.14), the articular surface preparation (p=0.67), positioning of screw intersection (p=0.692), ASA classification (p=0.204) and the attending surgeon (p=0.883).
Independent samples t-test of the entire cohort demonstrated no significant differences when comparing means of the preoperative HVA (p=0.085), postoperative HVA (p=0.141), Δ HVA (p=0.309), age (p=0.683), screw length (p=0.660), number of bony cortices involved in the fixation (p=0.663) and surgery duration (p=0.232) when comparing union and non-union groups (Table 3).
| T-test | Mean (non-union) | Mean (union) | p-value |
|---|---|---|---|
| Preoperative HVA | 32.4 (14.6) | 26.5 (12.9) | 0.085 |
| Postoperative HVA | 18.4 (9.1) | 15.3 (8.0) | 0.141 |
| Δ HVA | 14.0 (11.3) | 11.3 (10.5) | 0.309 |
| Age (years) | 61.5 (9.7) | 60.5 (9.0) | 0.683 |
| Length of screws (mm) | 61.7 (15.5) | 63.2 (12.6) | 0.66 |
| Surgery duration (min) | 42.5 (17.7) | 37.5 (6.1) | 0.232 |
| Number of cortices (n) | 3.74 (0.45) | 3.79 (0.45) | 0.663 |
Table 3: Results of the independent samples student’s t-test for comparing means between the union and non-union subgroups.
The Pearson chi-square further identified no significant difference in the incidence of smoking (p=0.899), indication for surgery (p=0.954) and male or female gender (p=0.701) between union and non-union groups (Table 4).
| Chi-square test | Percentage (non-union) | Percentage (union) | p-value |
|---|---|---|---|
| Indication (rigidus) | 80% | 79%% | 0.954 |
| Smoking | 15% | 16% | 0.899 |
| Gender (male) | 25% | 29.00% | 0.701 |
Table 4: Results of the chi-square test for comparing proportions between the union and non-union subgroups.
Discussion
We identified no significant differences in gender, smoking habits or primary diagnosis between union and non-union subgroups. T-test and chi-square tests showed no significant differences in means of HVA, age, smoking habits, ASA classification, gender, screw length, surgery duration, the number of bony cortices involved in the fixation,position of the screw intersection, fixation technique, articular surface preparation and the attending surgeon.
We have identified a radiographic union rate of 76.5% with no significant difference between hallux valgus and hallux rigidus subgroups. This does not match the findings in literature with a reported union rate of 88 to 100%, with a higher incidence of nonunion found in patients for whom the primary diagnosis was hallux valgus [2]. However, Chien et al. found no differences in outcome between hallux valgus and hallux rigidus when fixated with dorsal plate and a lag screw [11].
Two systematic reviews by Roukis et al. and Korim et al. found that respectively 32.7% and 82.4% of radiographically confirmed nonunions is symptomatic [2,12]. In our study 85.7% of non-unions were symptomatic. When regarding asymptomatic non-union as successful, the rate of succeeded MTP-1 joint fusions in our institute is 82%. This is still substantially lower than the results of the previously mentioned systematic reviews (98.2% and 94.6% respectively) [2,12].
In our study, 95% of joints were fixated using two crossed screws. This is the most popular fixation method and regarded as an adequate technique [3,8]. However, there is no clinical evidence suggesting a superior method of fixation although biomechanical studies suggest dorsal plating combined with a lag screw yields the most stable construction [2,3,7-10,12,13].
Aftercare protocols dictated all joints be immobilised by means of a hallux-cast in which full weight bearing was allowed. These protocols are based on several studies that suggest immediate full weight bearing is not causative to non-union. Moreover, detrimental effects of nonweight bearing are thereby prevented [2,14-16].
We are aware that this study has its limitations like the retrospective study design, no uniform treatment, several different surgeons, but a realistic reflection of daily practice in a large teaching hospital with fellows that stay for only a year.
Conclusion
We found a 23.5% incidence of non-union following arthrodesis of the first metatarsophalangeal joint. This incidence is alarmingly higher than described in previous literature, despite the usage of an apparent reliable joint preparation and fixation method. No clear risk factors for non-union were identified. Care must be taken in preforming this type of surgery since the results might be unfavourable than previously suggested.
Level of Evidence
Level 4
Conflict of Interest and Funding
All authors, their immediate families, and any research foundation with which they are affiliated did not receive any financial payments or other benefits from any commercial entity related to the subject of this article.
References
- Brewster M (2010) Does total joint replacement or arthrodesis of the first metatarsophalangeal joint yield better functional results? A systematic review of the literature. J Foot Ankle Surg 49: 546-552.
- Korim MT, Mahadevan D, Ghosh A, Mangwani J (2017) Effect of joint pathology, surface preparation and fixation methods on union frequency after first metatarsophalangeal joint arthrodesis: A systematic review of the English literature. Foot Ankle Surg 23: 189-194.
- Harris E, Moroney P, Tourne Y (2017) Arthrodesis of the first metatarsophalangeal joint-A biomechanical comparison of four fixation techniques. Foot Ankle Surg 23: 268-274.
- Johansson JE, Barrington TW (1984) Cone arthrodesis of the first metatarsophalangeal joint. Foot Ankle 4: 244-248.
- Wilkinson J (1978) Cone arthrodesis of the first metatarsophalangeal joint. Acta Orthop Scand 49: 627-630.
- Wilson JN (1967) Cone arthrodesis of the first metatarso-phalangeal joint. J Bone Joint Surg Br 49: 98-101.
- Buranosky DJ, Taylor DT, Sage RA, Sartori M, Patwardhan A, et al. (2001) First metatarsophalangeal joint arthrodesis: Quantitative mechanical testing of six-hole dorsal plate versus crossed screw fixation in cadaveric specimens. J Foot Ankle Surg 40: 208-213.
- Campbell B, Schimoler P, Belagaje S, Miller MC, Conti SF (2017) Weight-bearing recommendations after first metatarsophalangeal joint arthrodesis fixation: A biomechanical comparison. J Orthop Surg Res 12: 23.
- Curtis MJ, Myerson M, Jinnah RH, Cox QG, Alexander I (1993) Arthrodesis of the first metatarsophalangeal joint: a biomechanical study of internal fixation techniques. Foot Ankle 14: 395-399.
- Politi J, John H, Njus G, Bennett GL, Kay DB (2003) First metatarsal-phalangeal joint arthrodesis: A biomechanical assessment of stability. Foot Ankle Int 24: 332-337.
- Chien C, Alfred T, Freihaut R, Pit S (2017) First metatarsophalangeal joint arthrodesis in hallux valgus versus hallux rigidus using cup and cone preparation compression screw and dorsal plate fixation. Cureus 9: e1786.
- Roukis TS (2011) Nonunion after arthrodesis of the first metatarsal-phalangeal joint: a systematic review. J Foot Ankle Surg 50: 710-713.
- Hyer CF, Glover JP, Berlet GC, Lee TH (2007) Cost comparison of crossed screws versus dorsal plate construct for first metatarsophalangeal joint arthrodesis. J Foot Ankle Surg 47: 13-18.
- Berlet GC, Hyer CF, Glover JP (2008) A retrospective review of immediate weightbearing after first metatarsophalangeal joint arthrodesis. Foot Ankle Spec 1: 24-28.
- Dayton P, McCall A (2004) Early weightbearing after first metatarsophalangeal joint arthrodesis: A retrospective observational case analysis. J Foot Ankle Surg 43: 156-159.
- Kumar S, Pradhan R, Rosenfeld PF (2010) First metatarsophalangeal arthrodesis using a dorsal plate and a compression screw. Foot Ankle Int 31: 797-801.
Citation: Füssenich W, Scholten R, Rijnberg WJ, Somford MP (2018) High Incidence of Non-Union Following Arthrodesis of the First Metatarsophalangeal Joint. Clin Res Foot Ankle 6: 269. DOI: 10.4172/2329-910X.1000269
Copyright: © 2018 Füssenich W, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 8573
- [From(publication date): 0-2018 - Dec 19, 2025]
- Breakdown by view type
- HTML page views: 7565
- PDF downloads: 1008