Increases in the Service Connection Disability and Treatment Costs Associated With Posttraumatic Stress Disorder and/or Traumatic Brain Injury in United States Veterans Pre- and Post-9/11: The Strong Need for a Novel Therapeutic Approach
Received: 03-Jul-2018 / Accepted Date: 01-Oct-2018 / Published Date: 10-Oct-2018 DOI: 10.4172/2161-1165.1000353
Abstract
Objective: To evaluate the relative distribution of service connection disability ratings among veterans with a diagnosis of Posttraumatic Stress Disorder (PTSD) and/or Traumatic Brain Injury (TBI) from all branches of service who went to war before and after a historic attack on US by a terrorist group on September 11, 2001 (9/11); and to determine the associated cost to the nation.
Methods: The Veterans Health Administration (VHA) provides care to veterans at over 1,400 medical establishments across the United States. We used clinical data from these establishments, provided by researching the Veterans Administrations Informatics and Computing Infrastructure (VINCI). First, we identified all veterans with the ICD-9 code diagnosis of PTSD and/or TBI who received services within the VA between years 1998 to 2014. We excluded those who had no listed service connection disability rating. The remaining cohort was divided into four groups based on their period of service: Pre-9/11 Group – those who entered and left service before September 11, 2001; Post–9/11 Group– those who first entered the service after September 11, 2001; Overlap-9/11 Group – those who entered service before 2001 and left service after September 11, 2001; Reentered Post-9/11 Group – those who entered and then left service before September 11, 2001 and then reentered after September 11, 2001. Both annual and projected 50-year compensation costs were calculated for these groups.
Results: We identified 1,067,691 veterans with PTSD and/or TBI diagnosis who were service connected during the period under study. The relative distribution was highest in Pre-9/11 Group (N=797,285; 74.7%), followed by Post-9/11 Group (N=174,134; 16.3%), Overlap-9/11 Group (N=82,450; 7.7%) and Reentered Post-9/11 Group (N=13,822; 1.3%). Majority of veterans in all groups were male. Veterans in Pre-9/11 Group were oldest (66.3 ± 11.3), those in the Post-9/11 Group were the youngest (36.1 ± 8.7), with the Overlap-9/11 Group (41.2 ± 8.4) and the Reentered Post-9/11 Group (46.7 ± 8.9) showing intermediate average ages. The projected service connection disability compensation cost will be at least $20.28 billion/year and total $515 billion in coming 50 years. Based on the 2014 numbers, we project inpatient and outpatient costs to be $3.63 billion and $1.48 billion annually, and this represents $106.4 billion and 40.4 billion in over the next 50 years, respectively.
Conclusions: PTSD/TBI continues to be a devastating problem for veterans, their families, and our society. Rising costs and limited success with currently mandated therapies calls for a new therapeutic approach to help manage this unsustainable cost to the nation.
Keywords: Posttraumatic stress disorder (PTSD); Traumatic brain injury (TBI); Combat; Veterans; Service connection disability
Introduction
Post-Traumatic Stress Disorder (PTSD), an ongoing somatic and psychological reaction to extreme personal trauma, is a serious challenge for the Veterans Affairs (VA) Healthcare System, the Department of Defense (DOD), and US Veterans and their Families [1,2]. A comprehensive 2008 mental health study reported that 300,000 veterans, approximately 20% of the 1.65 million service members deployed to Iraq and/or Afghanistan, reported symptoms of PTSD [2]. A recent independent Army study reported PTSD rates of 10-15% among these soldiers [3]. Estimates based on earlier studies involving combat veterans from previous wars suggest the lifetime prevalence of PTSD to be 10-30% [4]. PTSD was formerly classed as an anxiety disorder, but has now been redefined as a trauma- and stressor-related disorder [5,6]. The incidence of PTSD increases as combat soldiers are exposed to increased frequency of traumatic events [7].
Traumatic Brain Injury (TBI) is defined as an alteration in brain function, or other evident brain pathology, caused by an external force [8]. In the US, approximately 5.3 million people suffer from TBI and related disabilities [9-11]. Approximately 1.7 million new cases develop each year, and 75% of these are mild TBI [12-14]. TBI is associated with increased risk of PTSD, depression, and posttraumatic headache [15-18] and often leads to broader cognitive, somatic, neurobiological, and psychosocial dysfunctions [19-21]. According to Veterans Affairs data, 201,435 veterans from all eras enrolled with VA have a diagnosis associated with TBI [22] and 56,695 veterans of Afghanistan: Operation Enduring Freedom/Iraq: Operation Iraqi Freedom (OEF/ OIF) enrolled with the VA have been evaluated for a condition possibly related to TBI [23]. According to the Defense and Veterans Brain Injury Center, more than 361,000 of US veterans were diagnosed with TBI reaching a peak of 32,000 cases per year in 2011 [24,25]. Despite the encouraging trend of decreased incidence of TBI in veterans, there will likely be more than 20,000 new incident cases per year as majority of these injuries occur in the non-deployed environment [26]. Due to changing nature of conflict with increased use of improvised explosive devices and blast injuries in recent wars, majority of veterans are being diagnosed with mild TBI, which overlaps and is associated with increased risk of PTSD. Since service connection disability rating and associated cost trends for these two overlapping mental conditions will not have any significant difference, we examined them together.
A majority (94%) of veterans seeking mental health treatment in VA clinics apply for PTSD disability benefits [27]. Between the period of 1999-2004, the number of veterans receiving disability payments for PTSD increased dramatically by 79.5% as compared to a 12.2% increase in other disabilities during the same period [28]. Two ways to explain this significant increase in PTSD associated disability payments include, (i) the suggestion that the nature of warfare has changed and with that change the recognition and the diagnosis of PTSD and associated trauma, or (ii) the argument that, increasingly, veterans exaggerate combat experiences [29,30], falsify military service [31-33] and malinger/exaggerate psychiatric symptoms to secure PTSD disability compensation [34-37].
PTSD-related healthcare costs are increasing rapidly because any service member diagnosed with war-related PTSD is entitled to disability payments that can now reach $2 million over a lifetime [38]; necessary treatments for associated comorbidities drive the total costs even higher. The VA currently spends between $3 and $4.5 billion each year to treat PTSD [39], and the scope of the problem is increasing. The cost of VA and Social Security disability payments combined with healthcare costs and treatment of PTSD is estimated to reach more than one trillion dollars over the next 30 years [40]. Factors that might be playing a role in this increasing cost include, (i) an increase in PTSD and TBI diagnosis, (ii) an increase in service connection because of frequent and multiple deployments and (iii) an increase in awareness about PTSD and associated treatment cost.
The US was attacked by a terrorist group on September 11th, 2011 and that initiated a new era of different and prolonged wars in which multiple countries were involved making it a historical event. Number of service members entering and deployed to the wars suddenly increased with multiple deployments. In addition, daily news about 9/11 on media acted as triggers for precipitating PTSD symptoms in Vietnam and First Gulf War veterans and they started coming to VA for care in increased numbers. The primary objective of this research study was to evaluate the relative distribution of service connection disability rating for veterans suffering from PTSD and/or TBI from all branches of service pre- and post-September 11, 2001. The secondary objective was to assess and project the disability/compensation costs and inpatient and outpatient treatments cost to the nation annually and over the next 50 years.
Methods
We conducted this retrospective cohort study using national data extracted through the Veterans Administrations Informatics and Computing Infrastructure (VINCI). VINCI workspace provides access to multiple databases including the Corporate Data Warehouse (CDW) and the National Patient Care Database. The Veterans Health Administration (VHA) provides care to veterans at over 1,400 establishments across the United States, organized into a system of 21 Veterans Integrated Service Networks (VISN). Each Veteran has a unique identifier in the CDW database. The quality of data from these sources is well documented, and the data have been widely used by our team and other investigators for retrospective longitudinal studies [41]. The data and analyses include veterans who received care through these VA establishments between December 1998 and May 2014. The study was reviewed and approved by the Institutional Review Board of Kansas City Veterans Affairs Medical Center, Missouri, USA.
Study population
As shown in the schematic representation of study population (Figure 1), we first identified all veterans with PTSD and/or TBI diagnosis using International Classification of Disease (ICD)-9 code(s) for PTSD (309.81) and TBI (850.0 – 859.9, V15.52) irrespective of gender, race, ethnicity and age, who received services within the VA between 1998 and 2014. From this population, we then excluded veterans who had no listed service connection to get a clean cohort of veterans with PTSD and/or TBI diagnosis and percent service connection. Thus, this analysis was restricted to veterans having 0-100% service connection.
We further divided the cohort into the following four groups based on their period of service:
• Pre- 9/11 Group – those who entered and left service prior to September 1, 2001
• Post – 9/11 Group – those who first entered the service after September 1, 2001
• Overlap - 9/11 Group – those who entered service prior to 2001 and left service after September 1, 2001
• Reentered Post- 9/11 Group – those who first entered and left service prior to September 1, 2001, then reentered in service after September 1, 2001.
Finally, data of veterans with PTSD and/or TBI within each service period group (Group 1 - 4) were analyzed for the following:
• Service-connection related disability ratings of 0% to 100% obtained from the records at the time of data extraction. VA determines about the severity of disability based on the submitted medical evidence as part of claim, or documents obtained from military records and rates disability from 0% to 100% in 10% increments (e.g. 10%, 20%, 30% etc.). If a Veteran has multiple disabilities, then a combined disability rating that are not additive is calculated and rounded to the nearest 10%, for example if a Veteran has one disability rating of 60% and a second disability of 20%, then the combined rating is 70% and not 80% because subsequent disability ratings are applied to an already disabled veteran [42].
• Demographic data including gender and age at the time of data extraction.
• Annual costs for service connection disability ratings (0% - 100%) in each group calculated by multiplying the number of veterans in that disability rating with US Veteran Compensation Programs listed 2017 compensation rates [42].
• Projected disability compensation cost for next 50 years calculated using predictive model that included number of veterans in service connection disability rating X annual 2017 compensation rates for specific service connection disability rating X expected years of payment obtained by subtracting average age of veterans in each group from projected life expectancy of 85 years.
• Associated costs with inpatient stays and outpatient visits were calculated using methodology developed by the VA Health Economics Resource Center (HERC) and reported in VINCI data base. Details of HERC methodology are in the Guidebook for the HERC Person-Level Cost Datasets FY1998 – Present [43]. For inpatient, HERC developed an average cost methodology which assigns each inpatient stay the average cost of all inpatient stays that share its same demographic and discharge characteristics. The HERC average cost methodology was used to calculate per capita national cost of all inpatient care in the behavioral category 29 (psychiatry) and 30 (substance abuse treatment) during the fiscal years 1998-2014. On the other hand, outpatient costs are determined by assigning the average cost for all visits with the same CPT codes and visit type. We used HERC average cost methodology to calculate per capita national cost of all outpatient care in the behavioral category 29 (psychiatry) and 30 (substance abuse treatment) during the fiscal years 1998-2014.
Statistical analysis
Applicable software on VINCI workspace including SQL, Excel and SAS were utilized. Descriptive statistics were presented using proportions and means. Distributions and trends in disability ratings and costs were presented in absolute numbers, tables, charts and graphs. Predictive models, using published US Veterans Compensation programs, were used to estimate annual and future costs.
Results
Distribution based on period of service and percent service connection
As shown in Table 1, analysis of VINCI data collected from year 1998 through 2014 showed that there was a total of 1,339,937 veterans with PTSD and/or TBI diagnosis. For our study cohort, we excluded 272,246 veterans, who had no listed percent service connection, thus leaving 1,067,691 veterans with PTSD and/or TBI diagnosis and listed percent service connection.
| Number of Veterans with PTSD and/or TBI Diagnosis between 1998-2014 (N=1,339,937) à Excluded 272,246 veterans who have no service connection listed → Veterans with PTSD/TBI Diagnosis & listed service connection (N=1,067,691) | |||||
|---|---|---|---|---|---|
| Percent Service Connection | Pre-9/11 Group N (%) |
Post 9/11 Group N (%) |
Overlap 9/11 Group N (%) |
Reentered 9/11 Group N (%) |
Total N (%) |
| 0% | 23221 (2.9) | 2723 (1.6) | 1084 (1.3) | 268 (1.9) | 27296 (2.6) |
| 10% | 40400 (5.1) | 7288 (4.2) | 2758 (3.3) | 478 (3.5) | 50924 (4.8) |
| 20% | 23316 (2.9) | 5070 (2.9) | 2242 (2.7) | 343 (2.5) | 30971 (2.9) |
| 30% | 36269 (4.5) | 9881 (5.7) | 3960 (4.8) | 533 (3.9) | 50643 (4.7) |
| 40% | 35288 (4.4) | 14032 (8.1) | 5185 (6.3) | 709 (5.1) | 55214 (5.2) |
| 50% | 43236 (5.4) | 13516 (7.8) | 5439 (6.6) | 705 (5.1) | 62896 (5.9) |
| 60% | 57105 (7.2) | 22,358 (12.8) | 8653 (10.5) | 1333 (9.6) | 89449 (8.4) |
| 70% | 121603 (15.3) | 25292 (14.5) | 10219 (12.4) | 1690 (12.2) | 158804 (14.9) |
| 80% | 99255 (12.4) | 26900 (15.4) | 12932 (15.7) | 2174 (15.7) | 141261(13.2) |
| 90% | 73561 (9.2) | 19312 (11.1) | 12045 (14.6) | 2137 (15.5) | 107055 (10.0) |
| 100% | 244031(30.6) | 27762 (15.9) | 17933 (21.8) | 3452 (25.0) | 293178 (27.5) |
| Total | 797285 | 174134 | 82450 | 13822 | 10,67,691 |
Table 1: Relative distribution of Veterans with percent service connection among service period groups.
The relative distributions of veterans by service period groups and disability ratings of 0% to 100% are detailed in Table 1. Majority of veterans were in Pre-9/11 Group (N=797,285; 74.7%), followed by Post-9/11 Group (N=174,134; 16.3%), Overlap-9/11 Group (N=82,450; 7.7%) and Reentered Post9/11 Group (N=13,822; 1.3%). Table 1 shows that majority of veterans in all groups have greater than 50% service connection disability ratings.
Distribution based on diagnosis, gender and age
As shown in Table 2, PTSD was the predominant diagnosis with a relative percentage of 88% in Pre-9/11 Group; 71% in Post-9/11 Group; 77% in Overlap-9/11 Group and 85% in Reentered-9/11 Group respectively. Most veterans across the entire cohort were male; the Pre-9/11 Group (94%), Post-9/11 Group (91%), Overlap-9/11 Group (88%) and Reentered-9/11 Group (89%). The non-male population increased in all three Post - 9/11 groups. Non-male veteran population with a PTSD-only diagnosis increased remarkably in the Post-9/11 Group (14%), Overlap 9/11 group (18%) and Reentered-9/11 Group (15%) as compared to the Pre-9/11 Group (8%). Veterans in the Pre-9/11 Group were oldest (66.3 ± 12.1 years), youngest in Post-9/11 Group (36.1 ± 8.4) as compare to Overlap-9/11 Group (41.2 ± 8) and Reentered-9/11 Group (46.4 ± 8.8).
| Gender and Age | Pre-9/11 Group | Post-9/11 Group | Overlap 9/11 Group | Reentered-9/11 Group |
|---|---|---|---|---|
| Male | 94% | 91% | 88% | 89% |
| Non-Male | 6% | 9% | 12% | 11% |
| Mean Age ± SD | 66.3 ± 12.1 | 35.3 ± 8.4 | 41.2 ± 8 | 46.4 ± 8.8 |
Table 2: Distribution of Veterans by gender and age among various service period groups.
Estimated yearly compensation cost associated with percent service connection
As shown in Table 3, the relative distribution of yearly compensation cost was highest in Pre-9/11 Group ($15.6 billion) and lower in the Re-entered 9/11 Group ($267 million), the Post-9/11 group ($2.88 billion) and the Overlap-9/11 Group ($1.52 billion). At present, there is a total cost of $20.28 billion to the nation each year.
| Disability rating | Annual cost | Veterans #Pre-9/11 Group | Pre-9/11 Group Cost | Veterans #Post-9/11 Group | Post-9/11 Group Cost | Veterans #Overlap-9/11 Group | Overlap 9/11 Group Cost | Veterans #Reentered-9/11 Group | Reentered-9/11 Group Cost |
|---|---|---|---|---|---|---|---|---|---|
| 0% | $ 0 | 23,221 | $0 | 2723 | $0 | 1084 | $0 | 268 | $0 |
| 10% | $1,603 | 40,400 | $64,761,200 | 7288 | $11,682,664 | 2758 | $4,421,074 | 478 | $766,234 |
| 20% | $3,168 | 23,316 | $73,865,088 | 5070 | $16,061,760 | 2242 | $7,102,656 | 343 | $1,086,624 |
| 30% | $4,908 | 36,269 | $178,008,252 | 9881 | $48,495,948 | 3960 | $19,435,680 | 533 | $2,615,964 |
| 40% | $7,069 | 35,288 | $249,450,872 | 14032 | $99,192,208 | 5185 | $36,652,765 | 709 | $5,011,921 |
| 50% | $10,064 | 43,236 | $435,127,104 | 13516 | $136,025,024 | 5439 | $54,738,096 | 705 | $7,095,120 |
| 60% | $12,747 | 57,105 | $727,917,435 | 22358 | $284,997,426 | 8653 | $110,299,791 | 1333 | $16,991,751 |
| 70% | $16,065 | 1,21,603 | $1,953,552,195 | 25292 | $406,315,980 | 10219 | $164,168,235 | 1690 | $27,149,850 |
| 80% | $18,674 | 99,255 | $1,853,487,870 | 26900 | $502,330,600 | 12932 | $241,492,168 | 2174 | $40,597,276 |
| 90% | $20,985 | 73,561 | $1,543,677,585 | 19312 | $405,262,320 | 12045 | $252,764,325 | 2137 | $44,844,945 |
| 100% | $34,987 | 2,44,031 | $8,537,912,597 | 27762 | $971,309,094 | 17933 | $627,421,871 | 3452 | $120,775,124 |
| $15,617,760,198 | $2,881,673,024 | $1,518,496,661 | $266,934,809 |
Table 3: Yearly cost associated with service connection disability rating for each service period group.
Projected service connection disability compensation costs over the next 50 years
As shown in Table 4, the relative distribution of compensation cost will be approximately $297 billion, $141 billion, $67 billion and $10 billion for Pre-9/11 Group, Post-9/11 Group, Overlap-9/11 Group and reentered-9/11 group, respectively. The total projected cost will be approximately $515 billion over the next 50 years.
Inpatient treatment cost trends for each service period group
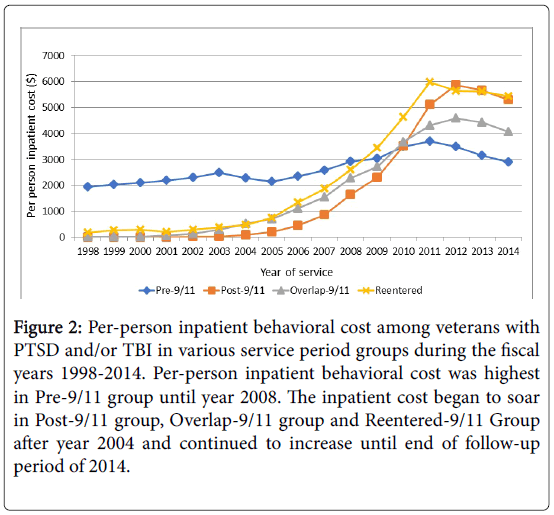
As shown in Figure 2, per capita national behavioral inpatient cost was highest in the Pre-9/11 Group until year 2008. Whereas, in the Post-9/11 Group, Overlap-9/11 Group and Re-entered-9/11 Group, the inpatient costs began to soar from around 2003-2004. In addition, 2008 through 2014, the per capita national behavioral inpatient cost remained remarkably higher in the Post-9/11 Group, the Overlap-9/11Group and the Reentered 9/11 Group.
Figure 2: Per-person inpatient behavioral cost among veterans with PTSD and/or TBI in various service period groups during the fiscal years 1998-2014. Per-person inpatient behavioral cost was highest in Pre-9/11 group until year 2008. The inpatient cost began to soar in Post-9/11 group, Overlap-9/11 group and Reentered-9/11 Group after year 2004 and continued to increase until end of follow-up period of 2014.
Estimated annual inpatient treatment costs for each service period group
As shown in Table 5, the relative distribution of annual inpatient treatment costs in year 2014 were highest in the Pre-9/11 Group ($2.3 billion), lowest in the Re-entered 9/11 Group ($75 million), while the Post-9/11 Group ($923 million) and Overlap-9/11 Group ($335.7 million) had more intermediate levels of cost. The total annual cost to the nation will be $3.63 billion in 2014 and presumably increase in coming years.
| Disability rating | Annual cost | Veterans #Pre-9/11 Group | Pre-9/11 Group Cost for 19 years | Veterans #Post-9/11 Group | Post-9/11 Group Cost for 49 years | Veterans #Overlap-9/11 Group | Overlap-9/11 Group Cost for 44 Years | Veterans # Reentered- 9/11 Group | Reentered-9/11 Group Cost for 38 Years |
|---|---|---|---|---|---|---|---|---|---|
| 0% | $0 | 23,221 | $0 | 2723 | $0 | 1084 | $0 | 268 | $0 |
| 10% | $1,603 | 40400 | $1,230,462,800 | 7288 | $572,450,536 | 2758 | $194,527,256 | 478 | $29,116,892 |
| 20% | $3,168 | 23316 | $1,403,436,672 | 5070 | $787,026,240 | 2242 | $312,516,864 | 343 | $41,291,712 |
| 30% | $4,908 | 36269 | $3,382,156,788 | 9881 | $2,376,301,452 | 3960 | $855,169,920 | 533 | $99,406,632 |
| 40% | $7,069 | 35288 | $4,739,566,568 | 14032 | $4,860,418,192 | 5185 | $1,612,721,660 | 709 | $190,452,998 |
| 50% | $10,064 | 43236 | $8,267,414,976 | 13516 | $6,665,226,176 | 5439 | $2,408,476,224 | 705 | $269,614,560 |
| 60% | $12,747 | 57105 | $13,830,431,265 | 22358 | $13,964,873,874 | 8653 | $4,853,190,804 | 1333 | $645,686,538 |
| 70% | $16,065 | 121603 | $37,117,491,705 | 25292 | $19,909,483,020 | 10219 | $7,223,402,340 | 1690 | $1,031,694,300 |
| 80% | $18,674 | 99255 | $35,216,269,530 | 26900 | $24,614,199,400 | 12932 | $10,625,655,392 | 2174 | $1,542,696,488 |
| 90% | $20,985 | 73561 | $29,329,874,115 | 19312 | $19,857,853,680 | 12045 | $11,121,630,300 | 2137 | $1,704,107,910 |
| 100% | $34,987 | 244031 | $162,220,339,343 | 27762 | $47,594,145,606 | 17933 | $27,606,562,324 | 3452 | $4,589,454,712 |
| $296,737,443,762 | $141,201,978,176 | $66,813,853,084 | $10,143,522,742 |
Table 4: Fifty Years projected cost associated with service connection disability rating for each service period group.
Projected inpatient treatment costs for the next 50 years
As shown in Table 5, assuming a life expectancy of 85 years of age, the Pre-9/11 group veterans will require care for 19 years. The Post-9/11 group, being the youngest, will require care for 49 years. The Overlap-9/11 group will need care for 44 years, and the Reentered-9/11 group will need care for 38 years. Using estimated annual inpatient treatment costs for each service period group we project the relative distribution of inpatient cost will be approximately $43.7 billion, $45.2 billion, $14.7 billion and $2.8 billion for Pre-9/11, Post-9/11, Overlap-9/11 and Reentered-9/11 groups, respectively. The total projected cost will be approximately $106.4 billion to the nation over the next 50 years.
| Service period groups | # of veterans | Per person Inpatient TX cost 2014 data | Annual inpatient TX Cost | Per person Outpatient TX cost 2014 data | 50 Year Cost inpatient treatment | Annual outpatient TX cost | 50 Year Cost outpatient treatment |
|---|---|---|---|---|---|---|---|
| Pre-9/11 Group | 7,97,285 | $2886.76 | $2.3 billion | $1328.27 | $43.7 billion | $1.06 billion | $20.14 billion |
| Post-9/11 Group | 1,74,134 | $5300.64 | $923 million | $1578.72 | $45.23 billion | $275 million | $13.48 billion |
| Overlap-9/11 Group | 82,450 | $4071.57 | $335.7 million | $1479.75 | $14.78 billion | $122 million | $5.37 billion |
| Reentered-Group | 13,822 | $5426.25 | $75 million | $1987.20 | $2.85 billion | $27.5 million | $1.05 billion |
| Total | $3.63 billion | $106.56 billion | $1.48 billion | $40.04 billion |
Table 5: Annual and 50 years projected inpatient and outpatient treatment cost for PTSD. and TBI.
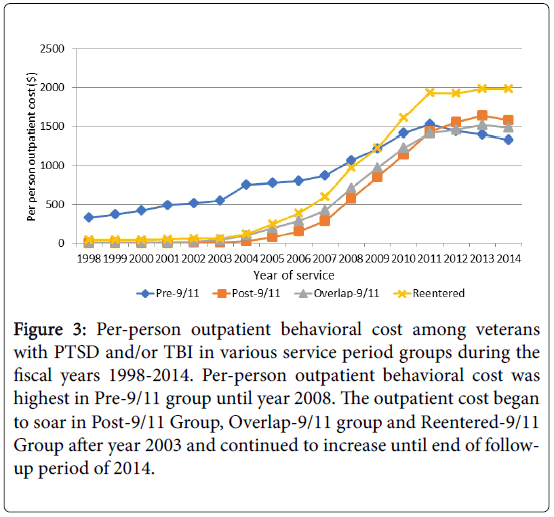
Outpatient treatment cost trends for each service period group
As shown in Figure 3, the per capita national behavioral outpatient cost was also highest in the Pre-9/11 Group until year 2008. However, the Post-9/11 Group, Overlap-9/11 group and Reentered- 9/11 Group, outpatient costs began to soar after 2003. In addition, after 2009 until the end of the follow-up period for 2014, the per capita national behavioral outpatient cost remained remarkably higher in the Post-9/11, the Overlap-9/11 and the Reentered-9/11 Groups.
Figure 3: Per-person outpatient behavioral cost among veterans with PTSD and/or TBI in various service period groups during the fiscal years 1998-2014. Per-person outpatient behavioral cost was highest in Pre-9/11 group until year 2008. The outpatient cost began to soar in Post-9/11 Group, Overlap-9/11 group and Reentered-9/11 Group after year 2003 and continued to increase until end of followup period of 2014.
Estimated annual outpatient treatment cost for each service period group
As shown in Table 5, the relative distribution of annual outpatient treatment costs for 2014 was highest in the Pre-9/11 ($1.06 billion), lowest in the Re-entered 9/11 ($27.5 million) and intermediate for both the Post-9/11 ($275 million) and Overlap-9/11 ($122 million) groups, respectively. In 2014, total cost to the nation was $1.48 billion, and presumably this will increase in future years.
Projected outpatient treatment cost for next 50 years
As shown in Table 5, using estimated annual outpatient treatment cost for each service period group, we now project the relative distribution of outpatient cost to be approximately $20 billion, $13.5 billion, $5.86 billion and $1.04 billion for Pre-9/11, Post-9/11, Overlap-9/11 and Reentered-9/11 Groups, respectively. The total projected cost to the nation over the next 50 years will be approximately $40.4 billion.
Discussion
In this retrospective cohort study of 1.339,937 million veterans from all branches of services between the years 1998 and 2014, majority of veterans had a diagnosis of PTSD alone (85%), followed by PTSD & TBI (8%) and TBI alone (7%). Group analysis revealed that veterans with PTSD alone or TBI alone diagnosis were highest in the Pre-9/11 Group. An increase in awareness among both veterans and VA healthcare providers, changes in institutional policies and programs for the routine screening of veterans for PTSD and TBI has resulted in increasing number of veterans seeking care at VA facilities due to a PTSD and/or TBI diagnosis [2,7,15,18,26,39].
Service connected disability rating are assigned on case by case basis to veterans, who suffered injuries or diseases while on active duty or made worse by military service [27,28,30]. A service connected disability of 0% simply means a mental condition (e.g. PTSD) has been formally diagnosed, but symptoms are not severe enough either to interfere with occupational and social functioning or to require continuous medication. At a more heightened traumatization (50% Service Connected) occupational and social impairment with reduced reliability and productivity due to such symptoms as: flattened affect; circumstantial, circumlocutory, or stereotyped speech; panic attacks more than once a week; difficulty in understanding complex commands; impairment of short- and long-term memory (e.g., retention of only highly learned material, forgetting to complete tasks); impaired judgment; impaired abstract thinking; disturbances of motivation and mood; difficulty in establishing and maintaining effective work and social relationships would be noted. At the most debilitating point, a service connection of 100% suggests total occupational and social impairment, due to such symptoms as: gross impairment in thought process or communication; persistent delusions or hallucinations; grossly inappropriate behavior; persistent danger of hurting self or others; intermittent inability to perform activities of daily living (including maintenance of minimal personal hygiene); disorientation to time or place; memory loss for names of close relatives, own occupation, or own name [28,30,42].
US Department of Veterans Affairs and veterans’ service organizations such as Disabled American Veterans have gotten better in educating veterans and helping them to file VA claims for disability benefits [43,44]. Service connected disability rating based compensation is a monthly tax-free benefit paid to veterans according to the degree of the disability on a scale from 10% to 100% [43]. In this study, we found that majority of veterans with a disability rating were in the Pre-9/11 group, followed by the Post-9/11 Group, Overlap-9/11 Group and Re-entered 9/11 Group. In addition, our results showed that majority of veterans had more than 50% service connected rating in each group. Using the published 2017 Compensation Rates, we project that the compensation cost for veterans with PTSD and/or TBI diagnosis will exceed $514 billion within 50 years. Our projection is conservative because it does not include additional benefits obtained from social security disability, Dependency and Indemnity Compensation, Special Monthly Compensation, housing and insurance benefits, medical treatments (inpatient and outpatient) and VA health care benefits for the spouse and any children less than 26 years old. Additionally, our projection does not also include the numbers from the support forecast issued by the Congressional Budget Office that the per patient costs of treating PTSD/TBI along with disability cost is increasing at an alarming rate and can potentially exceed a trillion dollars in the next 30-50 years [38,39].
In this study, the average age of veterans in the Pre-9/11 Group is approximately 66 years of age, as compared to the Post 9/11 Group that has an average age of 36 years. An increase in diagnosis-based disability at younger age poses unique challenges to the veteran and family members that include diminished career success, productivity and earnings coupled with increased cost of maintenance and healthcare due to an increased incidence of disease per adjusted life years [27,33]. Other challenges stemming from this group include increased costs for treatment and sustained rehabilitation to the nation. While treatment in the past has focused on addressing psychiatric issues, the medical understanding of the relationship between probable TBI and PTSD has changed significantly so that the phenomenon is now considered a psychiatric and/or physical disorder rather than solely a psychiatric problem [35-37].
The prevalence of PTSD/TBI is increasing, and the per patient cost of treating PTSD/TBI, along with associated service connection/ disability costs is also increasing at an alarming rate with a potential to exceed $660 billion over the next 50 years. While veterans receive treatment in support of PTSD and/or TBI, there is no evidence that current treatment is sufficient and or effective in reducing compensation cost associated with PTSD and/or TBI. There is no treatment approach that can be offered confidently for long-term benefit to PTSD patients [45]. The VA-mandated treatments for PTSD include standard psychiatric/psychopharmacological care, Cognitive Processing Therapy (CPT), Prolonged Exposure (PE) therapy, and PTSD Symptoms Management Group Therapy [46]. The overall approach focuses heavily on trauma and symptomology rather than on personal, social and vocational rehabilitation and community reintegration. Neither PE nor CPT recruits more than 3.8% of eligible veteran patients; furthermore, these mandated therapies are plagued by high drop-out rates such that they provide limited improvement for only the 28-40% of patients who do complete the therapy [47-49].
Current evaluations document that only 1.1 to 1.5% of PTSD sufferers/patients received benefit from the current VA mandated approaches [47]. In addition, a recent study indicates that significant numbers of caregivers delivering CPT and PE to veterans experience significant professional burnout and leave the system [48,49]. Numerous researchers are trying other complementary and alternative treatments for PTSD including meditation-based mantram intervention [50], acupuncture [51], healing touch therapy [52], yoga and mindfulness-based stress reduction therapy, but only limited evidence of therapeutic effectiveness is available. Given the current ineffectiveness of treatments for PTSD that result in significant reduction in the amount of needed compensations, exploration of a treatment model that reinforces veteran’s efforts to return to work and contribute to their community should be explored with high priority. In conclusion, there is a desperate and driving need for alternatives as well as more effective and innovative approaches to provide care for and help to in rehabilitating and re-integrating war veterans in to society and to manage unsustainable cost to the nation.
In this retrospective database cohort study, we considered and tried to minimize the impact of any of the usual potential limitations of including (i) accuracy of data quality and linkage, (ii) identifying cohort appropriately (study groups), (iii) defining endpoints clearly to avoid misclassifications, and, (iv) including all important cofounders. We identified veterans utilizing medical services at VA Hospitals during a defined period and diagnosed with PTSD and TBI using ICD-9 codes and to appropriately link them with the disability data, we removed all those veterans without listed disability rating from the population to make a cohort which then was further divided in four well defined groups. We included both PTSD and/or TBI diagnosis in groups as it is hard to dissociate the disability ratings and medical care cost from one or the other. Since the study excluded veterans not listed with disability rating during the study period, this study cannot comment if any of those veterans might get the disability and thus may affect the projected cost. In addition, one of the limitation of our study is to not accurately predict the increase in number of veterans with PTSD and/or TBI and the associated disability and medical care cost in coming years. In addition, we have not included cost-of-living adjustments in disability associated compensation benefits in projecting the cost. Despite these limitations our study helps in filling the knowledge gap by predicting conservative estimate of PTSD and/or TBI associated cost to nation in coming 50 years.
Conclusion
PTSD/TBI continues to be a devastating problem for veterans, their families, and our society. Rising costs and limited success with currently mandated therapies calls for a new therapeutic approach to help manage this unsustainable cost to the nation.
Acknowledgement
This work was supported by resources from both Kansas City VA Medical Center and Midwest Biomedical Research Foundation. Special thanks to Miss. Margarita Thakur of Research Service for her contributions in ensuring that scheduled meetings are held in timely manner among researchers for analysis of data and preparation of manuscript.
References
- Ghaffarzadegan N, Ebrahimvandi A, Jalali MS (2016) A Dynamic Model of Post-Traumatic Stress Disorder for Military Personnel and Veterans. PLoS One 11: e0161405.
- Tanielian T, Jaycox LH (2008) Invisible wounds of war: Psychological and cognitive injuries, their consequences and services to assist recovery. Santa Monica CAO: RAND Corp.
- Eisen SV, Schultz MR, Vogt D, Glickman ME, Elwy AR, et al. (2012) Mental and physical health status and alcohol and drug use following return from deployment to Iraq or Afghanistan. Am J Public Health 102 Suppl 1: S66-73.
- Richardson LK, Frueh BC, Acierno R (2010) Prevalence estimates of combat-related post-traumatic stress disorder: critical review. Aust N Z J Psychiatry 44: 4-19.
- Friedman MJ, Resick PA, Bryant RA, Strain J, Horowitz M, et al. (2011) Classification of trauma and stressor-related disorders in DSM-5. Depress Anxiety 28: 737-749.
- Kearney DJ, Simpson TL (2015) Broadening the Approach to Posttraumatic Stress Disorder and the Consequences of Trauma. JAMA 314: 453-455.
- Litz BT, Schlenger WE (2009) PTSD in Service Members and New Veterans of the Iraq and Afghanistan Wars: A Bibliography and Critique. PTSD Research Quarterly 20: 2009.
- McAllister TW (2011) Neurobiological consequences of traumatic brain injury. Dialogues in Clin Neurosci 13: 287-300.
- Selassie AW, Zaloshnja E, Langlois JA, Miller T, Jones P, et al. (2008) Incidence of long-term disability following traumatic brain injury hospitalization,United States, 2003. J Head Trauma Rehabil 23: 123-131.
- Thurman DJ, Alverson C, Dunn KA, Guerrero J, Sniezek JE (1999) Traumatic brain injury in the United States: A public health perspective. J Head Trauma Rehabil 14: 602-615.
- Zaloshnja E, Miller T, Langlois JA, Selassie AW (2008) Prevalence of long-term disability from traumatic brain injury in the civilian population of the United States, 2005. J Head Trauma Rehabil 23: 394-400.
- Corrigan JD, Selassie AW, Orman JA (2010) The epidemiology of traumatic brain injury. J Head Trauma Rehabil 25: 72-80.
- Coronado VG, Xu L, Basavaraju SV, McGuire LC, Wald MM, et al. (2011) Surveillance for traumatic brain injury-related deaths--United States, 1997-2007. MMWR Surveill Summ 60: 1-32.
- Leibson CL, Brown AW, Ransom JE, Diehl NN, Perkins PK, et al. (2011) Incidence of traumatic brain injury across the full disease spectrum: a population-based medical record review study. Epidemiology 22: 836-844.
- Lew HL, Otis JD, Tun C, Kerns RD, Clark ME, et al. (2009) Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: polytrauma clinical triad. J Rehabil Res Dev 46: 697-702.
- Carlson K, Kehle S, Meis L, Greer N, MacDonald R, et al. (2009) The Assessment and Treatment of Individuals with History of Traumatic Brain Injury and Post-Traumatic Stress Disorder: A Systematic Review of the Evidence. Washington (DC): Department of Veterans Affairs.
- Gironda RJ, Clark ME, Ruff RL, Chait S, Craine M, et al. (2009) Traumatic brain injury, polytrauma, and pain: challenges and treatment strategies for the polytrauma rehabilitation. Rehabil Psychol 54: 247-258.
- Hoge CW, McGurk D, Thomas JL, Cox AL, Engel CC, et al. (2008) Mild traumatic brain injury in U.S. Soldiers returning from Iraq. N Engl J Med 358: 453-463.
- Bazarian JJ, Cernak I, Noble-Haeusslein L, Potolicchio S, Temkin N (2009) Long-term neurologic outcomes after traumatic brain injury. J Head Trauma Rehabil 24: 439-451.
- Peskind ER, Brody D, Cernak I, McKee A, Ruff RL (2013) Military- and sports-related mild traumatic brain injury: clinical presentation, management, and long-term consequences. J Clin Psychiatry 74: 180-188.
- Riggio S (2011) Traumatic brain injury and its neurobehavioral sequelae. Neurol Clin 29: 35-47, vii.
- Bagalman E (2013) Traumatic brain injury among veterans. Congressional Research Service.
- Helmick KM, Spells CA, Malik SZ, Davies CA, Marion DW, et al. (2015) Traumatic brain injury in the US military: epidemiology and key clinical and research programs. Brain Imaging Behav 9: 358-366.
- DVBIC (2015) DOD Worldwide numbers for TBI. Defense and Veterans Brain Injury Center.
- Frueh BC, Elhai JD, Gold PB, Monnier J, Magruder KM, et al. (2003) Disability compensation seeking among veterans evaluated for posttraumatic stress disorder. Psychiatr Serv 54: 84-91.
- McNally RJ (2003) Progress and controversy in the study of posttraumatic stress disorder. Annu Rev Psychol 54: 229-252.
- Frueh BC, Grubaugh AL, Elhai JD, Buckley TC (2007) US Department of Veterans Affairs disability policies for posttraumatic stress disorder: Administrative trends and implications for treatment, rehabilitation, and research. Am J Public Health 97: 2143-2145.
- Baggaley M (1998) ‘Military Munchausen’s’: assessment of factitious claims of military service in psychiatric patients. Psychiatr Bull 22: 153-154.
- Frueh BC, Elhai JD, Grubaugh AL, Monnier J, Kashdan TB, et al. (2005) Documented combat exposure of US veterans seeking treatment for combat-related post-traumatic stress disorder. Br J Psychiatry 186: 467-472.
- Sparr L, Pankratz LD (1983) Factitious posttraumatic stress disorder. Am J Psychiatry 140: 1016-1019.
- Wessely S (2005) War stories: Invited commentary on documented combat exposure of US veterans seeking treatment for combat-related post-traumatic stress disorder. Br J Psychiatry 186: 473-475.
- Freeman T, Powell M, Kimbrell TA (2008) Measuring symptom exaggeration in veterans with chronic posttraumatic stress disorder. Psychiatry Res 158: 374-380.
- Frueh BC, Hamner MB, Cahill SP, Gold PB, Hamlin KL (2000) Apparent symptom overreporting in combat veterans evaluated for PTSD. Clin Psychol Rev 20: 853-885.
- Bilmes LJ (2011) Current and Projected Future Costs of Caring for Veterans of the Iraq and Afghanistan Wars. Harvard Kennedy School Mossavar- Rahmani Center for Business and Government.
- Congressional Budget Office (2012) The Veterans Health Administration’s Treatment of PTSD and Traumatic Brain Injury among Recent Combat Veterans. Congressional Budget Office.
- US Department of Veterans Affairs (2013) National Center for PTSD. Guidelines and Handout about under-standing of PTSD and PTSD treatment.
- US Department of Veterans Affairs (2015) VHA Corporate Data Warehouse. Veterans Affairs.
- US Veteran Compensation program (2017) Compensation rates for that percent service connection scale listed on US Veteran Compensation Programs website.
- Chen S, Shane A (2014) Guidebook for the HERC Person-Level Cost Datasets. Health Economics Resource Center.
- US Department of Veterans Affairs (2018) Veterans Benefits Administration, Compensation.
- Disabled American Veterans (2017) Fulfilling Our Promises To The Men And Women Who Served. DAV.
- Reisman M (2016) PTSD Treatment for Veterans: What's Working, What's New, and What's Next. P T 41: 623-634.
- Schnurr PP, Friedman MJ, Foy DW, Shea MT, Hsieh FY, et al. (2003) Randomized Trial of Trauma-Focused Group Therapy for Posttraumatic Stress Disorder Results From a Department of Veterans Affairs Cooperative Study. Arch Gen Psychiatry 60: 481-489.
- Steenkamp MM, Litz BT, Hoge CW, Marmar CR (2015) Psychotherapy for Military-Related PTSD: A Review of Randomized Clinical Trials. J American Medical Association 314: 489-500.
- Imel ZE, Laska K, Jakupcak M, Simpson TL (2013) Meta-analysis of dropout in treatments for posttraumatic stress disorder. J Consult Clin Psychol 81: 394-404.
- Garcia G, McGeary CA (2015) Evidence Based Treatments for PTSD and VHA Provider Burnout: The Impact of Cognitive Processing and Prolonged Exposure Therapies, Traumatology 21: 7-13.
- Bormann JE, Thorp SR, Wetherell JL, Golshan S, Lang AJ (2013) Meditation-based mantram intervention for veterans with posttraumatic stress disorder: A randomized trial. Psychological Trauma: Theory, Research, Practice, and Policy 5: 259-267.
- Kim YD, Heo I, Shin BC, Crawford C, Kang HW, et al. (2013) Acupuncture for posttraumatic stress disorder: A systematic review of randomized controlled trials and prospective clinical trials. Evidence Based Complementary and Alternative Medicine Article ID 6158.
- Jain S, McMahon GF, Hasen P, Kozub MP, Porter V, et al. (2012) Healing touch with guided imagery for PTSD in returning active duty military: A randomized controlled trial. Military Medicine 177: 1015-1021.
- Mitchell KS, Dick AM, DiMartino DM, Smith BN, Niles B, et al. (2014) A pilot study of a randomized controlled trial of yoga as an intervention for PTSD symptoms in women. J Trauma Stress 27: 121-128.
- Polusny MA, Erbes CR, Thuras P, Moran A, Lamberty GJ, et al. (2015) Mindfulness-Based Stress Reduction for Posttraumatic Stress Disorder Among Veterans A Randomized Clinical Trial. JAMA 314: 456-465.
- Ray WA (2011) Improving automated database studies. Epidemiology 22: 302-304.
Citation: Thakur H, Oni O, Singh V, Sharma R, Sharma M, et al. (2018) Increases in the Service Connection Disability and Treatment Costs Associated With Posttraumatic Stress Disorder and/or Traumatic Brain Injury in United States Veterans Pre- and Post-9/11: The Strong Need for a Novel Therapeutic Approach. Epidemiology (Sunnyvale) 8: 353. DOI: 10.4172/2161-1165.1000353
Copyright: © 2018 Thakur H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 5370
- [From(publication date): 0-2018 - Oct 31, 2025]
- Breakdown by view type
- HTML page views: 4484
- PDF downloads: 886