Liuzijue Qigong, a New Method of Voice Training after Thyroidectomy Due to Unilateral Vocal Fold Paralysis: A Case Study
Received: 03-Oct-2017 / Accepted Date: 24-Oct-2017 / Published Date: 31-Oct-2017 DOI: 10.4172/2161-119X.1000328
Abstract
Background: Liuzijue Qigong (LQG), a traditional Chinese health exercise (TCHE), is often speculated to help improve respiratory function but few studies support this for improving vocal function.
Case presentation: We studied LQG for individuals who experienced unilateral vocal fold paralysis (UVFP) after thyroidectomy and we noted some benefits. Videostroboscopy revealed the primary cause of hoarseness—paralytic vocal fold (VF) was fixed in a midline position, with a glottal flow leakage in the closing phases and irregular vibrations of the 2 VFs. Overcompensation was present in the normal side, followed by high pitch and phonotrauma. The vibration frequency of the 2 VFs varied when the fundamental frequency (F0) was changed, leading to diplophonia. We hoped to observe promotion of glottal closure using LQG to establish the correct breathing mode, with pitch inflection (lower pitch) relaxing intrinsic laryngeal muscles and improving breathiness (diplophonia appeared as F0 dropped from 191 to 124 Hz). We also hoped to see improvement of overall voice quality, specifically, pitch that reached a similar vibration frequency between both VFs, with LQG training relaxing the VFs and eliminating diplophonia. Four voice parameters were measured-normalized noise energy (NNE), jitter, shimmer and F0. Two perceptual parameters were measured, including diplophonia and grade of hoarseness (G).
Conclusion: After LQG training, jitter, shimmer and NNE decreased significantly (p<0.01); F0 decreased dramatically (p<0.001); and diplophonia and G improved significantly (p<0.001). LQG training may help with regulating breath, establishing patterns of articulation, eliminating intensive voice, restoring regularity of VF movements and promoting glottal closure. Pitch regulation can be combined with LQG training to obtain proper tone and pronunciation and acquisition of similar vibration frequency between VFs eliminating hoarseness and diplophonia. The study has been approved by the clinical ethics committee of NO.7 hospital in Shanghai. The patient voluntarily joined the trial with informed consents and we promised that his legitimate rights and interests would not be violated. The results of the study were published on the premise of patient’s agreement for scientific purposes.
Keywords: Liuzijue Qigong; Thyroidectomy; Unilateral vocal fold paralysis; Hoarseness; Diplophonia
Introduction
Liuzijue Qigong (LQG) is thought to treat patients who have chronic obstructive pulmonary disease (COPD), regulate breath and increase the value of specific airway conductance (sGaw) [1]. For those with chronic heart failure (CHF), LQG respiratory exercises can help with breathing by modifying mouth shapes to increase lung capacity and ventilation function and relieve dyspnea to ultimately increase cardiopulmonary function [2]. LQG respiratory exercises thus may help with breathing and perhaps improve quality of life.
Pronunciation during LQG training is based on respiratory exercises using medium volume to speak 6 real words, ‘x?,’ ‘h?,’ ‘h?,’ ‘s?,’ ‘chu?’ and ‘x?.’ If these 6 words are split into initials and finals, the pronunciation will be similar to conventional voice training methods. The 6 words begin with /x/, /h/, /s/, /ch/, respectively and are said in a ‘breathy voice,’ similar to the relaxed way of pronunciation in yawn-sigh [3,4]. Semioccluded vocal tract exercises (SOVT) begin with /s/, /x/ and the friction sound to narrow the mouth and produce slow and smooth airflow [5]. The finals of the 6 words are high vowels. When producing high vowels, the increased resistance in the vocal tract potentially decreases the impact force during vocal fold oscillation, without damage to the vocal folds. The method is similar to Smith accent technique (SAT) because it selects /i/, /u/, /ü / as training samples [6].
Thus, LQG training may be equivalent to conventional voice training methods as both can be used to regulate breathing mode and pronunciation, eliminating hoarseness caused by voice disorders. To verify this hypothesis, we first applied LQG training to individuals with unilateral vocal Fold paralysis (UVFP) after thyroidectomy. Xu’s group find that iatrogenic injuries caused by thyroidectomy often damage the recurrent laryngeal nerve (RLN), leading to unilateral or bilateral fixing in the vocal Folds (VF) [7]. Meek’s group analyze audio fragments of 67 cases after thyroidectomy and report that 7% have voice symptoms from UVFP [8], including breathiness, hoarseness, diplophonia, dysphagia, aspiration and cough [9]. The optimal rehabilitation period after UVFP is within one year after surgery, so timely and effective treatment may help patients to restore voice function. Many surgical treatments and voice training methods for UVFP have been reported for those who suffer from UVFP in a paramedian position and if they do not recover within 6 months, another surgery is needed, including intracordal injection, arytenoid adduction, laryngoplasty, transplantation or decompression of the RLN [10-19]. These surgeries could make the affected VF side move to the midline, promoting glottal closure and improving vocal function. Chen’s group summarize a review of patients with UVFP in the midline position who used voice training methods and during therapy, the potential psychological stress of UVFP patients was an important factor affecting voice rehabilitation [20]. Such individuals tend to lack confidence and avoid participation in social communication. Zheng’s group suggested that LQG training can help patients with panic and sleep disorders, reducing anxiety [21]. Sun’s group report that LQG training can improve work and life among the elderly and reduce dependence on drugs or medical treatment [22]. Psychological and physiological changes are relevant to gentle pronunciation encouraged in LQG training and those who persevere with LQG training often have better quality of life. Traditional Chinese health exercise (TCHE) may increase the frequency of social communication and promote psychological and physiological states positively. In our study, voice symptoms including hoarseness, diplophonia and high pitch were studied in an individual with UVFP after thyroidectomy. LQG training was used to observe whether easy and relaxed pronunciation of ‘x?,’ ‘h?,’ ‘h?,’ ‘s?,’ ‘chu?’ and ‘x?’ could improve hoarseness and whether LQG is useful for voice training.
Materials and Methods
Medical history, symptoms and signs
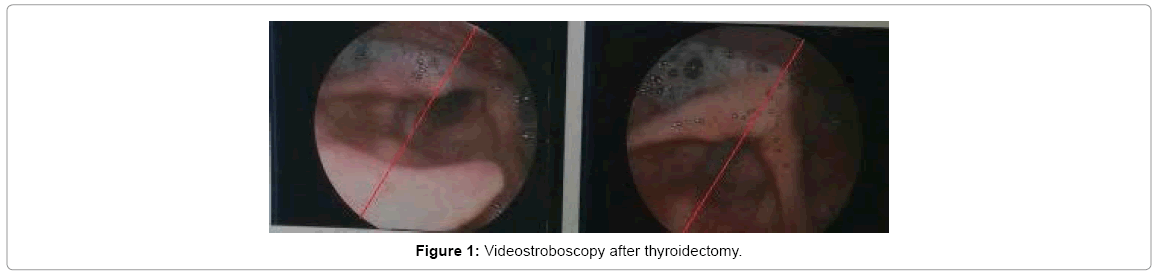
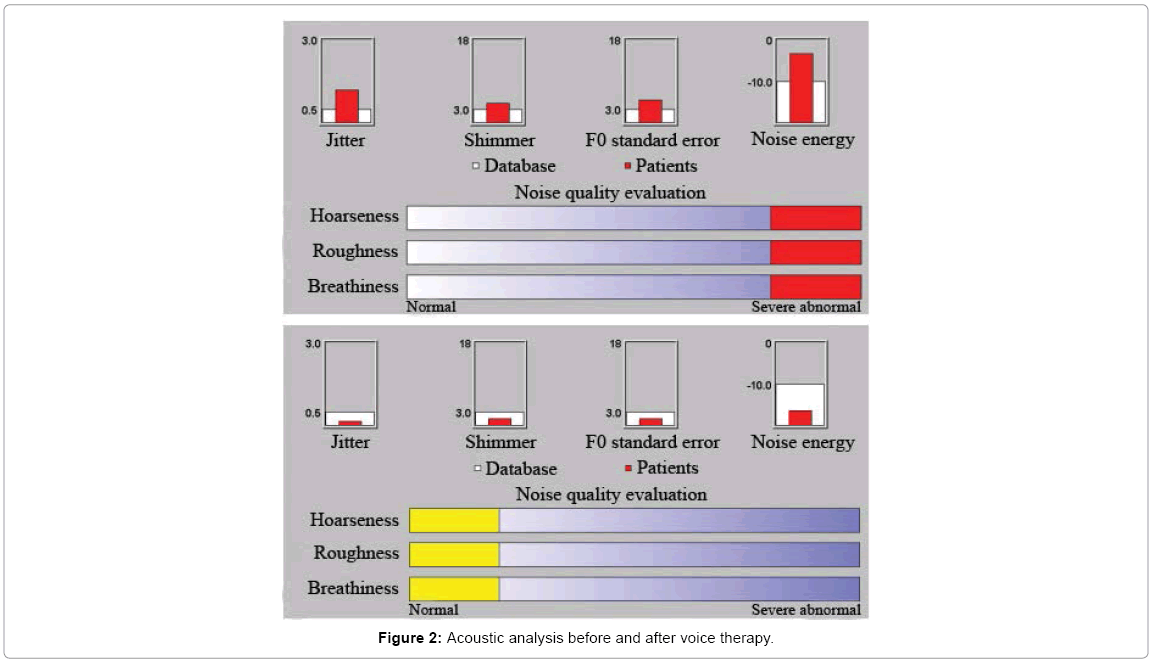
Y.S.C., a 64 year old male patient had a history of chronic laryngitis due to high-frequency voice use and loud speaking. Papillary thyroid tumors were suspected in 2014, so he underwent thyroidectomy in June at Changhai Hospital and thyroid adenoma was diagnosed after surgery. The movements of both VFs were normal before surgery, but the right side was paralyzed at the midline after thyroidectomy. Hoarseness appeared within 2 months. The patient reported in late 2015 that symptoms of hoarseness became serious. He then went to the Department of Respiration at Shanghai Seventh People’s Hospital and CT showed pneumonia. Antibiotics were administered for 15 days, but no significant improvement in hoarseness occurred. Videostroboscopy (Figure 1) showed paralysis on the right side, some sputum adhesion in the pyriform sinus and edema in the left side. Voice acoustic analysis (Figure 2) showed that severe breathiness and hoarseness before voice training and the breathing mode was chest respiration.
Acoustic analysis (Dr. Voice 3.0)
Acoustic testing was performed in a quiet room and the ambient noise was less than 40 dB SPL. The patient performed vocal exercises before recording, until he could make long and smooth sound; sit down, lips about 5-10 cm away from the microphone, with comfortable and natural sound sending out steady vowel /æ/ for more than 3 s. Acoustic analysis was made before and after voice training. The examiner intercepted 0.6 s of stable fragments in 3 s of sound /æ/ and noted the variables of the four voice parameters, including NNE, jitter, shimmer and F0. NNE was used to compare improvements in breathiness before and after voice training to confirm VF closure. Jitter and shimmer were used to compare changes of hoarseness. F0 variables were used to observe the effect of pitch in voice training in the individual with UVFP.
Data collection, labeling and selection
Audio recordings of sustained phonations were obtained before and after diplophonia treatment for a total of 16 voice samples. All audio fragments were recorded from Dr. Voice 3.0. To explore whether diplophonia existed in each audio fragment, these labels were used, 0 (diplophonia absent) and 1 (diplophonia present). For the GRBAS auditory perception assessment scale, the grade of hoarseness (G) is considered standard for voice evaluation and the labels were 0 (no deviance from normal voice quality), I (mild deviance), II (moderate deviance) and III (severe deviance).
Statistical analysis
Four voice and two perceptual parameters were collected, recorded and analyzed using SPSS 21.0 (IBM, city, state) to observe the variation tendency of NNE, jitter, shimmer, F0, G and diplophonia before and after voice training.
The intra-/inter-rater reliability for acoustic evaluation materials
Labels for G and diplophonia in 16 audio fragments were assigned by 3 authors JT, MWY and PW at 2 random times (morning and in the afternoon) before and after diplophonia treatment, respectively. A total of 96 variables were selected to calculate the intra-/inter-rater reliability using SPSS 21.0 (IBM). We calculated the intraclass correlation (ICC) to analyze the intra-/inter-rater reliability. The inter-rater reliability as ICC calculation was 0.939 to 0.773 and the intra-rater reliability as ICC calculation was 0.794 to 0.914.
Treatment
LQG training emphasizes that on the basis of abdominal respiration, lip constriction expiration is used to exhale slowly and uniformly for a long period of time. Pronunciation is as follows. When producing ‘x?,’ one should open the lips and teeth slightly, gather the corners of the mouth, set the upper and lower trough at the same level, retract the tongue body and leave a gap between trough and tongue, so that the airflow can be exhaled from upper and lower trough and tongue on both sides. When producing ‘h?,’ one should open the lips and teeth slightly and the tongue body should be slightly retracted and arched, sticking to the upper molars lightly, so that the airflow can be exhaled from the tongue and hard palate. When producing ‘h?,’ one should open the lips and teeth, lip-rounding and stick out the tongue. When producing ‘s?,’ one should gather the corners of the mouth, set the upper and lower trough in the same level, put the tip of the tongue into slot, so that the airflow can be exhaled from the teeth. When producing ‘chu?,’ one should gather the tongue body and the corners of the mouth and pull the lips open to tighten them. When producing ‘x?,’ one should close teeth and open the mouth and lips, retract the tip of the tongue and touch the middle of the lower trough gently, gather the corners of the mouth, set the upper and lower trough in the same level, so that the airflow can be exhaled from the gap between the upper and lower trough.
The patient’s surgery was more than a year prior and as selfhealing of RLN mostly occurs within a half year [20], the treatment was scheduled for a long term about 6 months, at the beginning of November 28th, 2015, for a total of 23 outpatient treatments (which is divided into 8 sessions and 15 sessions). After two months (8 sessions, once every Thursday) of LQG practice, breathiness was more obvious, but roughness and hoarseness were somewhat alleviated (Figure 2). LQG training can not only ease excessive throat tension, but also reduce the high value of F0, with better use of lower pitch. The individual was suggested to continue training at home with abdominal respiration and the 6 tones were exercised 5 times for each group, with training for 3 groups, for about 18 minutes. Hoarseness and diplophonia, however, still existed in daily communication. Therefore, in the following 4 months (15 sessions, once every Thursday) in the outpatient treatment, pitch inflection was considered to reach similar vibration frequency between both of the VFs, with LQG training establishing an easy pattern of articulation to improve overall standard of voice quality.
Results
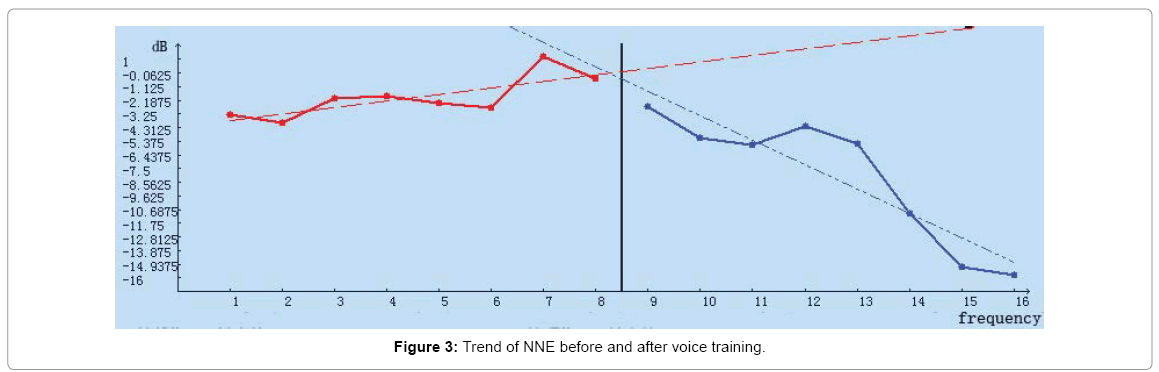
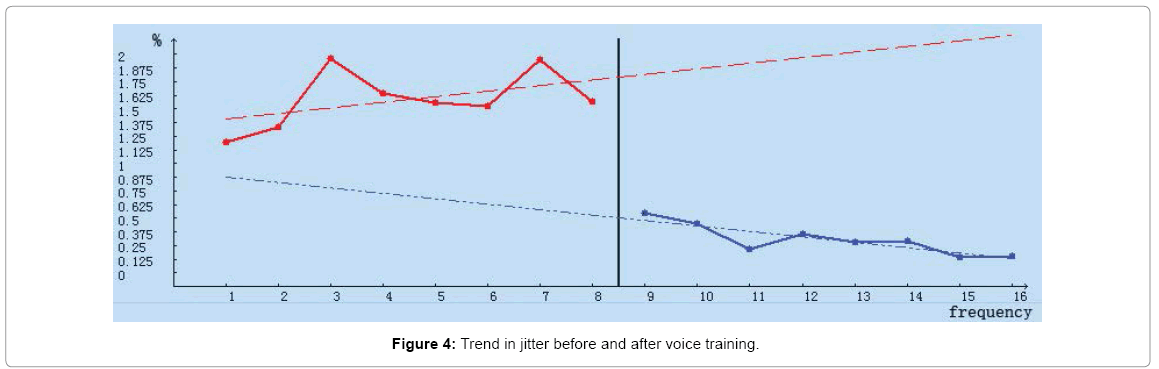
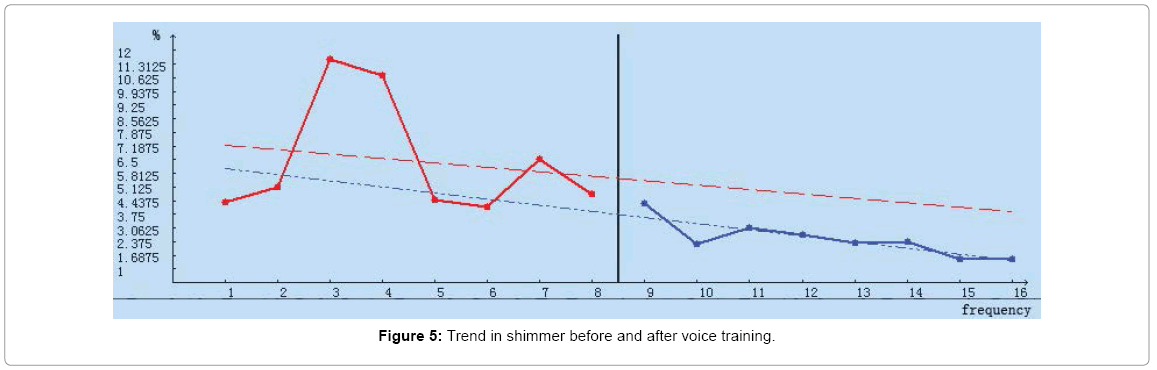
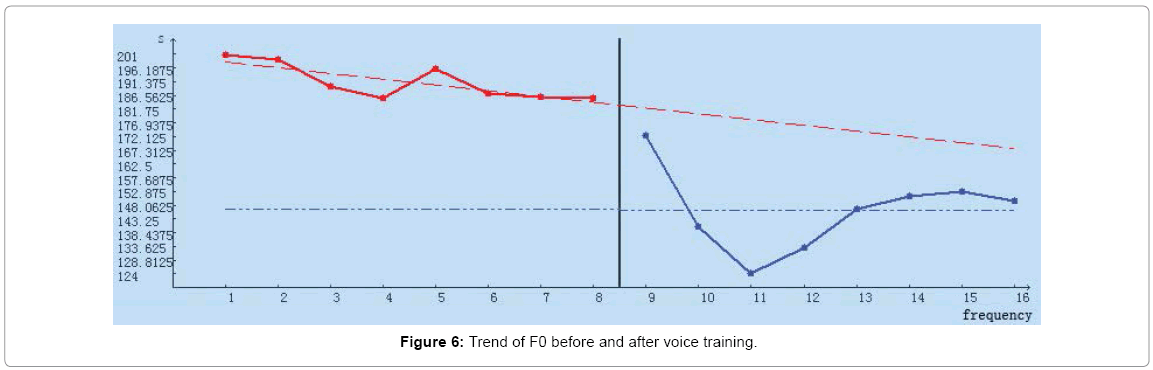
Prior to LQG training 8 voice variables were recorded as baseline and compared to results after 8 training sessions. These data appear in Tables 1-4 and Figures 3-6.
| Measurement | Baseline period | Treatment period |
|---|---|---|
| 1 | -3.28 | -2.68 |
| 2 | -3.96 | -5.14 |
| 3 | -2.09 | -5.62 |
| 4 | -1.83 | -4.26 |
| 5 | -2.44 | -5.54 |
| 6 | -2.75 | -10.99 |
| 7 | 1.18 | -15.17 |
| 8 | -0.53 | -15.83 |
| M±SD | -1.96±1.63 | -8.15±5.12 |
| Br | 0.397 | 0.851 |
| P | 0.006 | |
Table 1: NNE (dB) variables before and after voice training.
| Measurement | Baseline period | Treatment period |
|---|---|---|
| 1 | 1.2 | 0.55 |
| 2 | 1.33 | 0.45 |
| 3 | 1.96 | 0.22 |
| 4 | 1.64 | 0.35 |
| 5 | 1.56 | 0.28 |
| 6 | 1.52 | 0.29 |
| 7 | 1.95 | 0.14 |
| 8 | 1.57 | 0.15 |
| M ± SD | 1.59 ± 0.27 | 0.30 ± 0.14 |
| Br | -0.025 | 0.462 |
| P | <0.001 | |
Table 2: Variables for Jitter (%) before and after voice training.
| Measurement | Baseline period | Treatment period |
|---|---|---|
| 1 | 4.35 | 4.32 |
| 2 | 5.14 | 2.22 |
| 3 | 11.58 | 3.07 |
| 4 | 10.75 | 2.71 |
| 5 | 4.47 | 2.32 |
| 6 | 4.14 | 2.35 |
| 7 | 6.53 | 1.47 |
| 8 | 4.77 | 1.5 |
| M ± SD | 6.47 ± 3 | 2.50 ± 0.92 |
| Br | 0.309 | 0.149 |
| P | 0.003 | |
Table 3: Shimmer (%) variables before and after voice training.
| Measurement | Baseline period | Treatment period |
|---|---|---|
| 1 | 200.76 | 172.26 |
| 2 | 199.17 | 140.47 |
| 3 | 189.77 | 124.23 |
| 4 | 185.63 | 133.07 |
| 5 | 195.70 | 146.61 |
| 6 | 187.14 | 150.96 |
| 7 | 185.95 | 152.63 |
| 8 | 185.74 | 149.60 |
| M ± SD | 191.23 ± 6.35 | 146.23 ± 14.36 |
| Br | 0.399 | 0.309 |
| P | <0.001 | |
Table 4: F0 (Hz) variables before and after voice training.
Hoarseness
NNE variables significantly changed after treatment and Figure 3 shows that NNE variables were lower after voice therapy. NNE was stable and within the normal range (<-10 dB) after the sixth therapy session. Jitter variables were also lower after therapy and Figure 4 shows these jitter data were stable and within the normal range (<0.5%) after the second therapy session. Shimmer variables changed after therapy and Figure 5 shows that shimmer was lower after voice therapy and was stable and within the normal range (<3%) after the fourth therapy session.
After voice therapy variables of F0 decreased to the lowest values and diplophonia emerged after 3 sessions of enhanced lower pitch training (Figure 6). Therefore, pitch inflection was used in the treatment stage, with LQG training establishing an easy pattern of articulation to increase F0 gradually. F0 was stable and within the normal range (158.00 ± 23.91 Hz [23]) after the fifth session.
Diplophonia therapy
A total of 8 audio fragments were recorded as baselines when diplophonia appeared and these were compared with 8 audio fragments during the treatment period after changing therapeutic techniques to use LQG training and to search for proper tone. The labels of G and diplophonia in 16 audio fragments were assigned by 3 authors, respectively. Scores for analyzed audio fragments appear in Tables 5 and 6.
| Measurement | Baseline period | Treatment period | ||
|---|---|---|---|---|
| 1 | 0 | 1 | 0 | |
| 1 | 6 | 0 | 0 | 6 |
| 2 | 3 | 3 | 1 | 5 |
| 3 | 6 | 0 | 3 | 3 |
| 4 | 5 | 1 | 0 | 6 |
| 5 | 6 | 0 | 0 | 6 |
| 6 | 6 | 0 | 1 | 5 |
| 7 | 3 | 3 | 0 | 6 |
| 8 | 5 | 1 | 6 | 0 |
| M ± SD | 0.81 ± 0.394 | 0.23 ± 0.425 | ||
| P | <0.001 | |||
Labels were 0 (diplophonia absent), and 1 (diplophonia present). Diplophonia in the 8 measurements was recorded. There were statistically significant differences when comparing diplophonia (p<0.001) which improved significantly
Table 5: Scores before and after diplophonia therapy.
| Measurement | Baseline period | Treatment period | ||||||
|---|---|---|---|---|---|---|---|---|
| III | II | I | 0 | III | II | I | 0 | |
| 1 | 6 | 0 | 0 | 0 | 0 | 0 | 3 | 3 |
| 2 | 6 | 0 | 0 | 0 | 0 | 0 | 5 | 1 |
| 3 | 3 | 3 | 0 | 0 | 1 | 5 | 0 | 0 |
| 4 | 0 | 6 | 0 | 0 | 0 | 0 | 3 | 3 |
| 5 | 0 | 5 | 1 | 0 | 0 | 0 | 6 | 0 |
| 6 | 0 | 6 | 0 | 0 | 0 | 2 | 2 | 2 |
| 7 | 5 | 1 | 0 | 0 | 0 | 2 | 3 | 1 |
| 8 | 4 | 2 | 0 | 0 | 1 | 5 | 0 | 0 |
| M ± SD | 2.48 ± 0.545 | 1.15 ± 0.799 | ||||||
| P | <0.001 | |||||||
Labels were 0 (no deviance from normal voice quality), I (mild deviance), II (moderate deviance), and III (severe deviance). The frequency of G in the 8 measurements was recorded. There were statistically significant differences in G (p<0.001). Scores decreased but mild deviance was still present
Table 6: Grade of hoarseness before and after diplophonia therapy.
Discussion and Conclusion
Laryngeal nerve injury after thyroidectomy is a primary cause of UVFP, but timely intervention can improve hoarseness. Chen’s group report that for unilateral vocal fold paralysis after thyroidectomy, injection laryngoplasty, voice training and neurolysis are recommended during the first 12 months but laryngeal reinnervation is suggested after 12 months [20]. The patient who had hoarseness after thyroidectomy a year previously did not accept another surgery and he wanted to learn voice training methods to improve hoarseness. Laryngoscope analysis showed midline paralysis on the right side and edema on the left side, as well as incomplete glottal closure when speaking. These symptoms were closely related to incorrect breathing and overcompensation of the left side after thyroidectomy. The individual was accustomed to chest respiration and a quickening breath with laborious talking. The affected side was fixed and the normal side moved across to the midline violently, locking the throat for speaking and increasing the volume. The pitch was driven by the volume, resulting in the F0 rising to about 191 Hz. Marc’s group suggested that high pitch led to a significantly worse closure compared to closure at normal pitch [24]. The individual who experiences phonotrauma might suffer from chronic edema on the normal side, gradually developing into severe hoarseness [25].
Based on the clinical diagnosis, during voice training, the program was first prescribed to regulate breath, avoid phonotrauma and resolve the phenomenon of breathiness caused by a glottal flow leakage. The individual presented with a fast and shallow breathing pattern, so the LQG respiratory exercises were used to establish abdominal respiration. Ping’s group suggested that physiological abdominal respiration is a natural, economical and effective way of respiration and it is used to provide adequate breathing support for pronunciation [26].
When the individual was asked to pronounce ‘h?’ sound and ‘h?’ sounds, an exaggerated yawn was recommended to open the pharyngeal cavity so that the vocal tract could be fully open and pharyngeal muscles could be relaxed and then the pronunciation time was extended when sighing to experience the feeling of relaxation, which was learned from yawn-sigh [3,4]. When the individual was asked to pronounce ‘x?’ sound, ‘s?’ sound, ‘chu?’ sound and ‘x?’ sound, similar to SOVT [5], the vocal tract was narrowed and the sound was supposed to be produced near the lips or tongue, coming into the pronunciation model of tip of the tongue-alveolus dentis and half of the exhaled air obstruction, to promote airflow running through the glottis uniformly for a long period of time, which might cause vibration of the VFs mucosa. As is mentioned, health qigong is a low-intensity physical activity, with limited metabolic equivalents [27]. LQG can help patients to extend the time of speaking and to experience the most relaxing and natural state of pronunciation without burden to the VFs.
LQG training changed bad habits of phonotrauma and locking the throat to speak by easing pronunciation. Under certain circumstances, intrinsic laryngeal muscles relaxed and muscular tension was reduced to relieve fatigue caused by high pitch talking. To improve pitch abnormalities, pitch inflection (lower pitch) could reduce F0 consciously, which can reduce edema on the normal side caused by over compensatory pronunciation, as well as promote complete closure between the VFs. Through this period of voice training, jitter, shimmer and NNE were significantly reduced and maintained within the normal range. However, during that time, the F0 were decreased to the lowest value of 124.23 Hz and diplophonia emerged after enhanced lower pitch training. Diplophonia was defined as the simultaneous presence of 2 pitches, or the impression of distinct diplophonic beating [28]. Cyclic waveform patterns arose from the beating of 2 signals with different fundamental frequencies. Ki’s group believes that there is a close relationship between the occurrence of diplophonia and the glottal conditions in tension imbalance [29]. Under normal circumstances, there is little difference in muscle tension on both sides of the VFs, the imbalance of movement will not occur. When the tension difference exceeds 20%, however, the balance of movement is broken and diplophonia appears. Qian’s group suggested that VF vibration is accompanied by energy transfer [30]. The energy flows into the VFs in the early opening and late closing phases and flows out of the VFs in the middle of the cycles and the majority of the energy is consumed by the lateral motion of VFs. The study also showed that the normal side was able to produce greater lateral motion and transfer more energy, compared with the affected side. The patient initially presented with a high pitch but no diplophonia, which could be regarded as subtle muscular tension differences between both VFs, stable below 20% and only one F0 signal. Pitch inflection (lower pitch) changed the vibration of the VF itself. The normal side produced greater lateral motion, passed more energy and gave better relaxation. At the same time, muscular tension decreased significantly, accompanied by a substantial decline in pitch. The affected side may produce limited lateral motion and pass less energy, so that muscular tension was relatively difficult to significantly change. There was a small decline in pitch and the muscular tension difference between both VFs was beyond 20%, so that the balance was broken and 2 different F0 signals appeared. We inferred from this phenomenon that diplophonia was closely related to the sharp pitch inflection and speaking with lower pitch made muscular tension of the affected side change significantly less than the normal side and diplophonia emerged. Therefore, in the following treatment period, therapeutic techniques were changed, including searching for proper tone to increase muscular tension of the normal side and narrowing the gap with the high tension of the affected side (the lateral motion of the affected side was limited and the tension was slightly increased), to reach similar vibration frequency between both of the VFs and to ensure that pitch was always maintained within the normal range [23]. Establishing a new pitch may influence the stability of articulation, so that the regulation of pitch can be worked with LQG training to ease pronunciation and to eliminate diplophonia.
Considering that 0.6 s of the stable segment /æ/ intercepted by the acoustic test cannot represent the entire 3 s audio fragment, we tested voice stability with subjective and objective evaluation methods to better reflect diplophonia in the audio fragments, including perceptual assessment (including diplophonia and G). The results show that LQG training can consolidate the correct way of pronunciation, with the regulation of pitch, to significantly reduce remissions in diplophonia after treatment. To a certain extent, less diplophonia can alleviate hoarseness and improve the overall voice quality. However, Table 6 shows that although there is a significant difference in G before and after treatment, mild deviance still existed after voice training. Therefore, voice therapy is not limited to stable statistics in audio fragments, but can be used to avoid hoarseness and diplophonia in daily life. The severity of psychological and social stress in an individual when speaking decreases after LQG training. During the 6 month LQG training, no exercise-related issues occurred and LQG appeared to be safe. Furthermore, selecting LQG as a health promotion program is advantageous because it can be practiced without the limitation of place and time and it requires no special equipment.
Limitations and Outlook
Laryngeal nerve injury after thyroidectomy may cause UVFP and LQG training may help those people to better articulate and compensate for lost function. However, the etiology of UVFP is complicated and UVFP types are fluid. For instance, paramedian paralysis of UVFP often presents as the affected side deviating from the midline and fixing in that position. To make the vocal glottis close completely, the normal side should move across the midline, eventually closing to the affected side, so the effectiveness of voice training should be verified. The best time for voice training is within one year and in contrast, the individual in this case obtained rehabilitation after the best period of time, while benefited from it. For patients with various courses of diseases, differences in rehabilitation efficacy should be confirmed. Thus, we suggest that LQG training may help reverse diplophonia caused by tension imbalances between the VFs and remove hoarseness caused by UVFP.
Acknowledgement
The authors thank Zheng H and Zhou S from the Department of Otolaryngology, Changhai Hospital of the Second Military Medical University.
Funding
Funded by Key Specialty Construction Project of Pudong Health and Family Planning Commission of Shanghai (Grant No. PWZz2013?01)
References
- Xiao CM, Zhuang YC (2015) Efficacy of Liuzijue Qigong in individuals with chronic obstructive pulmonary disease in remission. J Am Geriatr Soc 63: 1420-1425.
- Yan XF (2016) Effect of Liuzijue and Baduanjin on exercise tolerance in patients with chronic heart failure. Chin Meds Mod Distance Educ 16:126-128.
- D'Alatri L, Galla S, Rigante M, Antonelli O, Buldrini S, et al. (2008) Role of early voice therapy in patients affected by unilateral vocal fold paralysis. J Laryngol Otol 122: 936-941.
- Schindler A, Bottero A, Capaccio P, Ginocchio D, Adorni F, et al. (2008) Vocal improvement after voice therapy in unilateral vocal fold paralysis. J Voice 22: 113-118.
- Titze IR (2006) Voice training and therapy with a semi-occluded vocal tract: Rationale and specific underpinnings. J Speech Lang Hear Res 49: 448-459.
- Aliaa K (2003) Effects of the ‘Smith Accent Technique’ of voice therapy on the laryngeal functions and voice quality of patients with unilateral vocal fold paralysis. International Congress Series 1240: 1235-1241.
- Xu DY, Li KY (2016) Cause and treatment of unilateral vocal Fold paralysis. J Clin Otorhinolaryngol Head Neck Surg 30: 423-426.
- Meek P, Carding PN, Howard DH, Lennard TW (2008) Voice change following thyroid and parathyroid surgery. J Voice 22: 765-772.
- Mattioli F, Bergamini G, Alicandri-Ciufelli M, Molteni G, Luppi MP, et al. (2011) The role of early voice therapy in the incidence of motility recovery in unilateral vocal fold paralysis. Logoped Phoniatr Vocol 36: 40-47.
- Shi JB, Zheng HL, Chen SC (2010) Modified arytenoid adduction for unilateral vocal fold paralysis. J Audiol Speech Pathol 18: 29-32.
- Friedman AD, Burns JA, Heaton JT, Zeitels SM (2010) Early versus late injection medialization for unilateral vocal fold paralysis. Laryngoscope 120: 2042-2046.
- Lee SW, Kim JW, Chung CH, Mok JO, Shim SS, et al. (2010) Utility of injection laryngoplasty in the management of post-thyroidectomy vocal Fold paralysis. Thyroid 20: 513-517.
- Li M, Zheng HL. (2012) Exploration and reinnervation of recurrent laryngeal nerve injury in thyroid surgery. Chin J Practical Surg 32: 364-367.
- Reiter R, Brosch S (2012) Laryngoplasty with hyaluronic acid in patients with unilateral vocal fold paralysis. J Voice 26: 785-791.
- Li M, Wang W, Chen S (2012) Laryngeal reinnervation using ansa cervicalis for iatrogenic unilateral vocal fold paralysis. Chin J Gen Surg 27: 267-273.
- Fang TJ, Lee LA, Wang CJ, Li HY, Chiang HC (2009) Intracordal fat assessment by 3-dimensional imaging after autologous fat injection in patients with thyroidectomy-induced unilateral vocal Fold paralysis. Surg 146: 82-87.
- Wang CC, Chang MH, Wang CP, Liu SA, Liang KL, et al. (2012) Laryngeal electromyography-guided hyaluronic acid vocal fold injection for unilateral vocal fold paralysis-preliminary results. J Voice 26: 506-514.
- Dionigi G, Rovera F, Rausei S, Castelnuovo P, Dionigi R, et al. (2010) Postoperative laryngoscopy in thyroid surgery: Proper timing to detect recurrent laryngeal nerve injury. Langenbeck’s Arch Surg 395: 327-331.
- Siu J, Tam S, Fung K (2016) A comparison of outcomes in interventions for unilateral vocal fold paralysis: A systematic review. Laryngoscope 126: 1616-1624.
- Chen XH, Wan P, Yu YB, Li M, Xu Y, et al. (2014) Types and timing of therapy for vocal fold paresis/paralysis after thyroidectomy: A systematic review and meta-analysis. J Voice 6: 799-808.
- Zheng XT, Sun HH, Tu RS (2012) Rehabilltation of ‘Six Healing Sounds’ on anxiety disorders of the old and middle-aged person. International J TCM 4: 299-302.
- Sun SJ, Zheng XT, Tu RS (2012) Effect of ‘Six Healing Sounds’ on quality of life of the old and middle-aged person. Int J TCM 5: 405-406.
- Sun SJ, Wei LY (2017) Nursing care for patients with mutational falsetto receiving thyroplasty. J Nsg Sci 8: 50-51.
- De Bodt MS, Clement G, Wuyts FL, Borghs C, Van Lierde KM (2012) The impact of phonation mode and vocal technique on vocal fold closure in young females with normal voice quality. J Voice 26: 818.
- Tang J, Wan P, Chen X (2016) The review on voice disorders and rehabilitation in teachers of primary and secondary school. Lin Chung Er Bi Yan Hou Tou Jing Wai Ke Za Zhi 30: 84-88.
- Wan P (2012) Speech Therapy. In: Wan P, Huang ZM, Yu P (eds.) Evaluation and rehabilitation of speech disorder. Beijing: People's Medical Publishing House, pp: 61-66.
- Yan J, Jun Z (2013) Analysis of the TCM theory of traditional Chinese health exercise. J Sport Health Sci 4: 204-208.
- Aichinger P, Hagmüller M, Roesner I, Bigenzahn W, Schneider-Stickler B, et al. (2016) Diplophonia disturbs jitter and shimmer measurement. Folia Phoniatr Logop 1: 22-28.
- Hong KH, Kim HK (1999) Diplophonia in unilateral vocal fold paralysis and intracordal cyst. Otolaryngol Head Neck Surg 121: 815-819.
- Xue Q, Mittal R, Zheng X, Bielamowicz S (2014) Computational study of effects of tension imbalance on phonation in a three-dimensional tubular larynx model. J Voice 28: 411-419.
Citation: Tang J, Huang W, Yu M, Wan P, Jin X, et al. (2017) Liuzijue Qigong, a New Method of Voice Training after Thyroidectomy Due to Unilateral Vocal Fold Paralysis: A Case Study. Otolaryngol (Sunnyvale) 7:328. DOI: 10.4172/2161-119X.1000328
Copyright: © 2017 Tang J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 7672
- [From(publication date): 0-2017 - Dec 15, 2025]
- Breakdown by view type
- HTML page views: 6065
- PDF downloads: 1607