Long Acting and Permanent Contraceptive Use in Arada Sub City, Addis Ababa, Ethiopia, 2017
Received: 17-May-2018 / Accepted Date: 29-May-2018 / Published Date: 01-Jun-2018 DOI: 10.4172/2161-0711.1000618
Keywords: Long acting; Permanent; Contraceptive; Arada sub city; Addis ababa; Health extension program
Introduction
Family planning is the voluntary use of natural or modern methods of contraceptives by individuals and couples. Contraceptive can be divided in to two broad categories: hormonal and non-hormonal [1]. There are also two categories of hormonal contraceptive, combined estrogen and progesterone and progesterone only. Long acting reversible contraceptive are the copper intrauterine system, injectable and implants and the non-hormonal contraceptives intrauterine device [1,2].
The methods include: Contraceptive injection, which works for up to 12 weeks and can be repeated. Devices that are fitted inside a woman womb intrauterine device (IUDS) and inter uterine system (IUS) which lasts for between 5 and 10 years and can be replaced. Injections, IUDS, the IUS and implant are called long acting reversible contraceptives because a woman can stop using them if she wants to get pregnant.
Using long acting contraceptive helps women and their families perceive health and also contribute to improve the overall quality of their lives by reduction of morbidity and mortality of mothers and children. Avert unplanned pregnancy and its adverse consequences that are high risk for abortion, prevention of HIV/AIDS and other sexual transmitted disease, improve standard of living and increases house hold income, and promote the conservation and efficient use of natural resources [3]. Key drivers of long acting contraceptive use depends on the following factors, easy availability of method, social/ spousal/partner support, spouse/partner communication/knowledge about economic and health benefits of family planning, correct knowledge of effectiveness and side effects about specific modern family planning methods. Knowledge and use of modern contraceptive improved through the implementation of health extension program [4].
The health extension program was introduced in 2002/2003 during HSDP II in rural parts of Ethiopia which covers a total 84% of the population and urban health extension program also introduced 2009, during HSDP the program is being implemented in urban areas of all states as well as Addis Ababa and Dire Dawa administration to make essential health service available at the grass root level with the aim of creating healthy environment and healthy living [5]. It is a package of promotive, preventive and basic curative service targeting households particularly women and children, and favorable change where seen in the coverage of major health programs particularly immunization, family planning and environmental health [6].
Extension workers identify and train model families that have been involved in other development work, and/or that have acceptance and credibility by the community, as early adopters of desirable health practices to come role model in line with health extension packages. Model families help to diffuse health message leading to the adoption of the desired practices and Perceived by the community. There is different in fertility between urban and rural women. Women from urban areas have TFR of 2.4 while women living rural areas have almost three times as many children with TFR of 6. Oromia region has the highest fertility, at 6.2 children per-woman [7].
Utilization of long acting and permanent contraceptives is very minimal related to socio-cultural and psychological issues, and also little is known about long acting and permanent contraceptives. Therefore, it is important to assess the prevalence and factors that influence long acting contraceptives among model and non- model households during the implementation of urban health extension program in Addis Ababa at Arada sub city [7].
This research gives insight of awareness on long acting and permanent contraceptives utilization and factors affecting the use of long acting and permanent contraceptive methods during the implementation of urban health extension programme. The findings of this study will be a good feedback to the stakeholders like the Addis Ababa City Administration Health Bureau about the effectiveness of the urban health extension programme.
Materials and Methods
Study design, area and period
This study is conducted by Cross-sectional study design in Arada sub city, which is one of the ten sub cities and found at the center of Addis Ababa. The total population of sub-city is approximately 300,000. Among these 34% women are in reproductive age (15-49 year). The sub city had ten woreda, and more than 100 health extension worker. In each woreda there is one health extension worker per 500 houses holds. This study is conducted from November 25 to December 20, 2017.
Source population
The source populations are all Women of reproductive age who live in Arada sub city, Addis Ababa Ethiopia.
Study population
The study populations were women of reproductive age who live and use contraceptives in those selected woreda of Arada sub-city.
Inclusion criteria and exclusion criteria
All women of reproductive age group who use contraceptive and live in those selected woreda at least for six months were included and Woman of reproductive age group who live less than six months in the woreda were excluded.
Ethical consideration
Ethical clearance was obtained from ACIPH and Haromaya University ethical committee. Based on the ethical clearance, AACAHB wrote a support letter to Arada Subcity health office. Informed verbal consent was received for each study subjects and one who is willing to take part in the study has the full right to do so. To ensure confidentiality of respondents, their name was not mentioned on the questionnaires. All interviews were made individually to keep privacy appropriate information was provided on use of long acting contraceptives methods for those women who have used it.
Sample size determination
In this study two formulas were used to address the research objectives. The first one is by using single population proportion. It was assumed that a study done on the prevalence and factors affecting use of LAPMS contraceptive, in Jinka, SNNPR, Ethiopia showed the prevalence of contraceptive among participants was about 39.5% of this LAMPS contributes for 7.3%, 95% confidence interval, 10% nonresponse rate and 2.5% marginal error.
n=Z2 × P (1−P)/d2
=1.962 × 0.073 (1−0.073)/0.0252
=416+10% non-response rate=458
The second sample size were calculated using Epi info stat calc. with the following assumption CI=95% power or 1-β=80%, Ratio (exposed to un exposed)=1:1, with a prevalence of long acting contraceptives use 7.3% as study done on the prevalence and factors affecting use of long acting contraceptive in Jinka, SNNPR, Ethiopia. The sample size calculated the Epi info Stat Cal was about 432+10% non-response rate=476. From the above two calculations, the largest sample size were taken. Therefore, using the formulas and other assumptions, a total of 476 included in the study.
Sampling procedure
Multi stage sampling technique was used to get the required sample size. The total sample size were allocated proportionally to the size of the selected Woreda of women at reproductive age groups and the total sample size equally divided for model and non-model households, these calculated sample size for each woreda were collected every Nth based on sampling fraction using systematic sampling technique. The proportional allocation of the sample size was made for each Woreda by using the following formula.
Ni=Ni−n/N
Data collection procedure
Structured questionnaires were used to collect the data, which was prepared in English version first then was translated into Amharic language.
The questionnaires include the following section socio-economic, socio cultural, demographic, variables related with long acting contraceptive use. The interview was made by house to house visit by ten female interviewers who have had diploma in nursing and have experience of data collection and two supervisors who have had BSC in nursing were recruited and trained. Data collectors and supervisor were trained for two days on questions include in the questionnaires, on interviewing techniques, purpose of the study, and importance of privacy. The supervisor was responsible to oversee the overall data collection process. The questionnaires were checked for consistencies and completeness.
Dependent and independent variable
Long acting contraceptive use is the dependent variable and sociodemographic characteristics such as: age, occupation, marital status, educational level and religion, parity, misconceptions, partner influence, number of children alive, health worker, access and availability of services are independent variables.
Operational definition
Long acing contraceptives: Contraceptive that can be used for an extended period of time once the women used it like implants for 3-5 years and IUD for 10 years.
Permanent method: Contraceptive method used for life like female sterilization and male vasectomy.
Long acting contraceptive prevalence rate (CPR): Refers to the proportion of women of reproductive age who are using long acting contraceptive method at particular point in time.
Modern contraception: Any medicine, process, apparatus or method that prevents conception.
Model households: Those families who have got 4 months training on the 16 packages of health extension program and who implemented 75% of their training.
Non-model households: Those families who didn’t get the training on 16 packages of health extension program.
Data processing and analysis
Data was entered, coded and cleared using Epi-Info version 3.3.2 Statistical software package, then that data was exported in to SPSS 20 statistical software to analyze. Tables, frequencies, graphs, mean were used to present the data. The association between the dependent and independent variables were determined with ratio with 95% CI. Logistic regression analysis was performed to control the potential confounders. The association and significant between the explanatory and response variables were measured using odds ratio, p-values and 95% CI. The relative contributions of the selected variables to the outcome of interest were assessed using multivariate analysis and logistic regression.
Results
For this study 476 women of reproductive age were selected to participate in the study, out of this 476 (98.7%) women have completed their interviews [6]. (1.3%) women were not willing to participate in the study due to their personal reason. Analysis was made on data gathered from 469 respondents of the study.
Socio-demographic and socio-economic characteristics of the respondents
Out of the 469 study participants, 247 (52.7%) were model family, 222 (47.3%) were non-model family. The mean age of the study participants were 31.2 ± 5.7. The majorities of the respondents of the study in both group had 1-4 family size with mean 4.32 and ± 1.62 SD. The majority of the respondents in both non-model and model family 145 (65.3) and 149 (60.3) were orthodox Christian respectively. Majority of respondents from model family were completed primary education, 136 (61.3%) and (65.2%) for non-model and model family respectively. In both group majority of the respondents were married, 192 (86.5) and 223 (90.3) for model and non-model respectively. Regarding occupational status of the respondents there is no a difference between model and non-model.
The Majority of the respondents 135 (60.8%) and 148 (59.9%) model and non-model respectively had both television and radio, this can provide information about long acting contraceptive and related issues. There was no statically significant difference between model and non-model except family type and religion.
Regarding the average monthly income of the study participants, 232 (49.5%) of the respondents had average monthly income of less than 500 birr. More over 237 (50.5%) of respondent had average monthly income ≥ 500 birr (Table 1).
| Characteristics | Non-model (%) | Model (%) | χ2(df) | P-value |
|---|---|---|---|---|
| Family type | 222 (47.3) | 247 (52.7) | 6.36 (1) | 0.012 |
| 7.2 (3 ) | 0.063 | |||
| Age | ||||
| 18-24 | 31 (14) | 19 (7.7) | - | - |
| 25-29 | 71 ( 32) | 69 (27.9) | ||
| 30-34 | 51 ( 23) | 72 (29.1) | ||
| 35-49 | 69 (31) | 87 (35.2) | ||
| Family size | ||||
| 4-Jan | 142 (64) | 135 (54.7) | 0.063 (1) | 0.802 |
| >4 | 80 (36) | 112 (45.3) | ||
| Educational status | ||||
| Illiterate | 51 (23) | 49 (19.8) | 12.667 (2) | 0.569 |
| Primary education | 136 (61.3) | 161 (65.2) | ||
| Secondary/higher education | 35 (15.8) | 37 (15) | ||
| Religion | ||||
| Orthodox | 145 (65.3) | 149 (60.3) | 15.657 (2) | 0.03 |
| Muslim | 58 (26.1) | 76 (30.8) | ||
| Protestant | 19 (8.6) | 22 (8.9) | ||
| Marital status | ||||
| Married | 192 (86.5) | 223 (90.3) | 10.995 (1) | 0.199 |
| Non-married | 30 (13.5) | 24 (9.7) | ||
| Occupational status | ||||
| Housewife | 183 (82.4) | 203 (82.2) | 7.877 (1) | 0.994 |
| Government employee | 39 (17.6) | 44 (17.8) | ||
| Possession of radio/TV | ||||
| Only radio | 26 (11.7) | 33 (13.4) | 1.648 (3) | 0.648 |
| Only television | 52 (23.4) | 54 (21.9) | ||
| Both radio and Television | 135 (60.8) | 148 (59.9) | ||
| Both radio and Television | 135 (60.8) | 148 (59.9) | ||
| Not have both | 9 (4.1 ) | 12 (4.9) | ||
| Monthly income | ||||
| < 500 | 111 (50) | 121 (49) | 000 (1) | 0.989 |
| ≥ 500 | 111 (50) | 126 (51) | ||
Table 1: Sociodemographic and socioeconomic characteristics of women in reproductive Age group at Arada sub city, Addis Ababa, 2017(n=469).
Reproductive history of respondents
Majority the respondents 166 (74.8%) for model and 195 (78.9) had history of one or more pregnancies in their life time. The mean age of the pregnancy was 22.05 with ± 4.63SD and among their pregnancies about 189 (87.5%) non-model and 203 (83.9%) were wanted. Regarding number of live births among those respondents who had pregnancy history, in both model and non-model family majority of the respondents have children 4 and above (Table 2).
| Characteristics | Non-model (%) | Model (%) | χ2df | P-value |
|---|---|---|---|---|
| Previous experience pregnancy | ||||
| Yes | 166 (74.8) | 195 (78.9) | 0.671 (1) | 0.413 |
| No | 56 (25.2) | 52 (21.1) | ||
| Age at first pregnancy | ||||
| <15 | 15 (6.8) | 15 (6.1) | 5.9 | 0 .20 |
| 15-17 | 19 (8.6) | 28 (11.3) | ||
| 18-20 | 65 (29.3) | 65 (26.3) | ||
| 21-23 | 35 (15.8) | 41 (16.6) | ||
| >23 | 88 (39.6) | 98 (39.7) | ||
| Pregnancy wanted | ||||
| Yes | 189 (87.5) | 203 (83.9) | 2.987 (1) | 0.087 |
| No | 27 (12.5) | 39 (16.1) | ||
| Number of living children | ||||
| 0 | 20 (9.9) | 20 (8.8) | 3.943(2) | 0.139 |
| 3-Jan | 87 (42.9) | 68 (30) | ||
| 4 and above | 95 (47.3) | 139 (61.2) | ||
Table 2: Reproductive History of women in reproductive age group at Arada subcity,Addia Ababa, 2017 (n=469).
General knowledge, belief and side effects experienced/heard about long acting contraceptive use of respondents
Out of the total participants of the survey, only 232 (49.5%) had some general knowledge about LAPMs. Among LAPMs the most known method was implants which accounts for 232 (100%), followed by IUCD 175 (67.8%) and the least known methods were tubal ligation accounting for 44 (18.5%) of the responses. The majority of women 211 (90.9%) could mention at least two LAPMs and only 25 (10.8%) knew three or more methods. Regarding the characteristics of women with respect to knowledge of LAPMs, illiterates had less knowledge, 25 (52.1%) as compared to literate 244 (57.95%). Looking at their occupational status 46 (59.74%) who knew LAPMs were government employee followed by 220 (56.99%) house wife (Table 3).
| Knowledge on LAPMs (469) | Frequency | Percent |
|---|---|---|
| Yes | 232 | 49.5 |
| No | 237 | 50.5 |
| LAPMS known(232) | ||
| Implants | 232 | 100 |
| IUCD | 175 | 67.8 |
| Tubal ligation | 43 | 18.5 |
| Known 2 methods | 211 | 90.9 |
| Known 3 methods | 25 | 10.8 |
| Beliefs and side effects of long acting contraceptive(469) | ||
| Yes | 232 | 49.5 |
| No | 237 | 50.5 |
Table 3: General knowledge, beliefs and experienced/heard side effects about long acting contraceptive use of respondents.
Among women who had general knowledge about LAPMs, 232 (49.5%) encountered side effects and misconception and 194 (83.6%) this women said that use of implants would affect their health negatively. They said implants could cause 60 (31%) pain to the arm, Some women 39 (20%) encountered that implants could move around freely in the body once inserted and could be lost at the day of removal 22 (11%) bleeding, 14 (7%) uterine cancer, 14 (7%) infertility, 11 (5%) difficult to work. And the rest 34 (17.5%) said infection, decrease sexual desire; enlarge breast, head ache, hunger, weight gain, weight loss, and hypertension.
Regarding IUD, from 232 (100%) who heard/experienced side effect, about 111 (47.8%) said IUD could cause 53 (47.7%) infection, 13 (11.7%), excessive vaginal bleeding, 13 (11.7%) pain, 10 (6.3%) goes to the brain, 8 (7%) discomfort during sexual intercourse, and others said IUD could cause uterine cancer and also bad smell of the vagina. Among women who heard myths and misconception, IUD and implants could cause permanent infertility 19 (13.2%) and 14 (12.6%) respectively.
Contraceptive utilization in Arada sub-city respondents
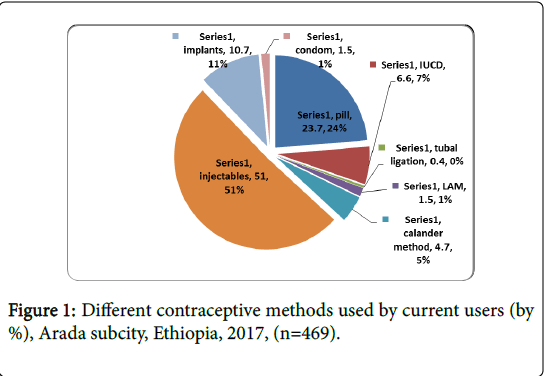
The data were collected from 469 (100%) respondents’ who were used different types of contraceptive in order to determine the prevalence of long acting and permanent methods of contraception. The majorities of the women 239 (51.0%) were used injectable contraceptives. The participants who have used 111 (23.7%) was pill, 31 (6.6%) IUCD, 50 (10.7%) Implants, both implants and IUD are long acting and they were 81 (17.3%) and 7 (1.5%) condom and permanent method was 2 (0.4%), some respondents were used natural methods like calendar and lactation amenorrhea with 22 (4.7%) and 7 (1.5%) respectively. Regarding respondents use of modern contraceptives the majority of respondents 265 (56.5) use for spacing, 132 (43.5) for limiting. Decision making about family planning use, majority of the respondents 412 (87.8%) had preferred joint decision for family planning usage. About accessibility of modern contraception is concerned, the dominant number 393 (83.8%) of the respondents reported that they had access to modern contraceptive and the dominant provider about 83.8% were public institution. Study participants have mentioned side effect contraceptive 138 (29.4%), husband dominance 106 (22.6%), religion 83 (17.7%) and 16 (3.4 %) lack of method mix as major weakness of service provision. Regarding long acting contraceptive 120 (25.6%) of the respondents have ever used long acting contraceptive, and the very reason for their interruption among those defaulters were 18 (3.8%) husband influence, 16 (3.4%) religion, 10 (2.1%) sex preference, and 40 (8.5%) health reason (Figure 1).
Utilization of modern contraceptive among model and nonmodel
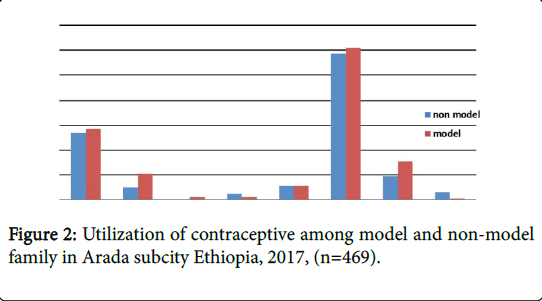
Pertaining to contraceptive practice, about 222 (47.3%) were nonmodel family, 247 (52.7%) were model family. When we compare both families utilization of long acting contraceptive implants and IUD were better practiced among model families as compared to non-model families which is statically significant as indicated by P value less than 0.05. Among those respondents the majority of the respondents have used injectable contraceptive. 122 (51%), and 117 (48.9%), injectable 57 (51.4%), and, 54 (46.6%) pill, 31 (62%) and, 19 (38%) implants, 21 (67.7%) and 10 (32.3%), IUCD, respectively model and non-model families. From 247 model families 222 were satisfied with information related to contraceptive given by health extension professional. About 382 (82.5%) of the respondents were interested to have contraceptive which will be provided by health extension professional at their home especially injectables and pill 201 (49.2%), and Pill 154 (32.8%) respectively, and the rest of the respondents 87 (17.5) were not interested to get any modern contraceptive at their home due to lack of confidence on the skill of health extension professional.
Figure 2 shows utilization of long acting and permanent (LAPM) contraceptive methods among model and non-model families, during the survey, the data were collected from 470 (100%) respondents’ who were used different types of contraceptives, in order to determine the prevalence of long acting and permanent methods of contraception from those respondents who were already taking different methods of contraceptives.
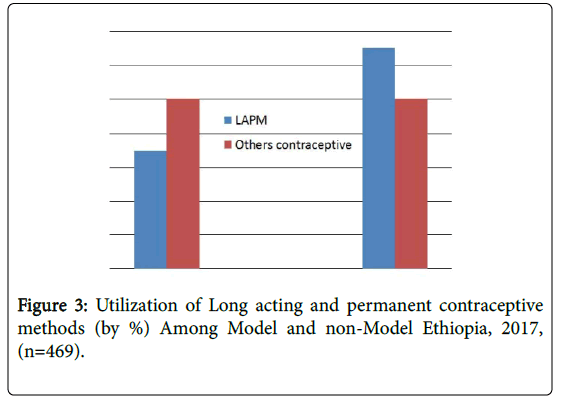
Utilization of LAPM among model and non-model families
The participants who have used long acting and permanent methods among non-model family were 29 (34.9%) ,whereas among model were 54 (65.1%), even though long acting and permanent methods used differently among model and non-model family other contraceptives methods utilized equally in both groups (Figure 3).
Socio-demographic factors associated with long acting contraceptive use
According to the bivariate analysis result of this study, being model family more likely to use long acting contraceptive methods compared to those women from non-mode family. The COR (1.9 (1.1, 3.1) showed that the women from model family were more likely to use long acting contraceptive methods than non-mode family. According this study, the COR of age group between 30-34 and 35-49 had significant difference on long acting contraceptive utilization as compared to age group 18-24 indicated by(COR (95%CI); 2.3 (1.1.17, 4.5); 2.0 (1.1, 4.0) respectively. Moreover, bivariate analysis of this study showed that family size had no significant relation with long acting contraceptive use as stated in Table 4. Bivariate analysis of this study indicates marital status had effect/association with long contraceptive utilization as indicated by (COR (95%CI); 6.3 (1.5, 26.4) as compared to non-married women.
| Variable | Long acting contraceptive | COR (95 %CI) | |
|---|---|---|---|
| Yes | No | ||
| Family type | |||
| Non-model* | 29 (13.1) | 193 (86.9) | 1 |
| Model | 54 (21.9) | 193 (78.1) | 1.9 (1.1,3.1)** |
| Age | |||
| 18-24* | 8 (10) | 42 (84) | 1 |
| 25-29 | 26 (18.6) | 114 (81.4) | 1.6 (0.8,3.1) |
| 30-34 | 18 (14.6) | 105 (85.4) | 2.3 (1.2,4.5)** |
| 35-49 | 31 (19.9) | 125 (80.1) | 2.057(1.1,4.0)** |
| Family size | |||
| 1-4* | 48 (17.3) | 229 (82.7) | 1 |
| >4 | 35 (18.2) | 157 (81.8) | 0.940(0.6,1.5) |
| Religion | |||
| Orthodox | 39 (13.3) | 255 (86.7) | 1.101 (0.4 3.0) |
| Muslim | 39 (29.1) | 95 (70.9) | 3.0 (1.1,8.1)* |
| Protestant* | 5 (12.2) | 36 (87.8) | 1 |
| Marital status | |||
| Married | 81 (19.5) | 334 (80.5) | 6.3 (1.5,26.4**) |
| Not married* | 6 (11.2) | 48 (88.8) | 1 |
Table 4: Socio-demographic factors associated with long acting contraceptive use in Arada subcity, Ethiopia, 2017 (n=469).
Socio-economic factors associated with long acting contraceptive use
Based on the result of this study, the crude OR showed that the respondents who were primary education indicated by (COR (95% CI; 3.6 (1.6, 8.3) are more likely to use long acting contraceptive as compared to women who were illiterate. Concerning the type of occupation being government employee had significant relation with long acting contraceptive utilization indicated by (COR (95%CI; 2.3 (1.3, 3.9).
Moreover, bivariate analysis of this study showed that the following variables Income, economical status, and possession radio/TV had no significant relation with long acting contraceptive use as stated in Table 5.
| Educational status | |||
| Illiterate* | 7 (7) | 93 (93) | 1 |
| Primary education | 64 (21.5) | 233 (78.5) | 3.649 (1.6,8.2)** |
| Secondary/higher education | 12 (16.7) | 60 (83.3) | 2.657 (1.0,7.1) |
| Occupational status | |||
| Housewife * | 59 (15.3) | 327 (84.7) | 1 |
| Government employee | 24 (28.9) | 59 (71.1) | 2.3 ( 1.3,3.9)** |
| Possession of radio/TV | |||
| Only radio | 8 (13.6) | 51 (86.4) | 0.1 (0.1,1.8) |
| Only television | 17 (16) | 89 (84) | 0.6 (0.2,1.9) |
| Both radio and Television | 53 (18.7) | 230 (81.3) | 0.7 (0.3,2.1) |
| Not have both* | 5 (23.8) | 16 (76.2) | 1 |
| Monthly income | |||
| < 500 | 41 (17.7) | 191 (82.3) | 1.0 ( 0.6,1.6) |
| ≥ 500* | 42 (17.7) | 195 (82.3) | 1 |
| Husband and wife education | |||
| Yes | 7 (36.6) | 12 (63.4) | 1.8 (1.1,3.0)* |
| NO | 16 (16.9) | 347 (83) | 1 |
Table 5: Socio-economic factors associated with long acting contraceptive use in Arada subcity, Ethiopia, 2017 (n=469).
Wife and husband education is one of the independent variable examined by logistic regression had association/effect on the use of long acting contraceptive as compared to not to have husbands and wife education indicated (COR (95% CI; 2.9 (1.2, 7.5).
Reproductive health factors associated with long acting contraceptive use
Bivariate analysis of this study indicates age at first marriage between 15-17 years had effect/association with long contraceptive utilization as indicated by (COR (95% CI); 2.3 (1.1, 4.8) as compared to age at first marriage greater than 23. Moreover, bivariate analysis of this study showed that the following variables number of children alive, pregnancy wanted or not wanted had no significant relation with long acting contraceptive use in the study area (Table 6).
| Age at first pregnancy | |||
| <15 | 6 (20) | 24 (80) | 1.4 (0.5,3.6) |
| 15-17 | 14 (29.8) | 33 (70.2) | 2.3 (1.1,4.8)** |
| 18-20 | 24 (18.5) | 106 (81.5) | 1.2 (0.7,2.2) |
| 21-23 | 10 (13.2) | 66 (86.8) | 0.8 (0.3,1.7) |
| >23* | 29 (15.6) | 157 (84.4) | 1 |
| Pregnancy wanted | |||
| Yes | 65 (16.6) | 327 (83.4) | 1 |
| No | 17 (25.8) | 49 (74.2) | 1.7 (0.9, 3.2) |
| Number of alive children | |||
| 0* | 6 (15) | 34 (85) | 1 |
| 3-Jan | 20 (12.9) | 135 (87.1) | 0.8 (0.3,2.3) |
| 4 and above | 48 (20.4) | 187 (79.6) | 1.5 (0.577,3.7) |
Table 6: Reproductive Health factors associated with long acting contraceptive use in Arada sub city, Ethiopia, 2017 (n=469).
Promotional factors associated with long acting contraceptive use
Regarding the bivariate analysis of this study availability of contraceptive methods, information provided by health extension professional at house hold, and health worker counseling about long acting contraceptive were some of the independent variable examined by logistic regression.
Availability of contraceptive methods, health extension professional information given to at house hold level, and health worker counseling had association/effect indicated by ((COR (95% CI); 1.8 (1.1, 3.01), 0.8 (1.1, 2.8), 1.8 (1.1, 2.9)), respectively on the use of long acting contraceptive as compared to methods not available, and not to have information by health extension professional at house hold level and not to have health worker counseling (Table 7).
| Health extension professional information at the respondents home | |||
| Given | 48 (22.1) | 169 (77.9) | 1.8 (1.1,2.8) |
| Not Given | 35 (13.9) | 217 (86.1) | 1 |
| Health worker counseling | |||
| Yes | 54 (21.4) | 198 (78.6) | 1.8 (1.1,2.9)** |
| No | 29 (13.4) | 188 (86.6) | 1 |
| Availability of long acting methods | |||
| Available | 25 (25) | 75 (75) | 1.8 (1.05,3.04)** |
| Not available* | 58 (15.7) | 311 (84.3) | 1 |
Table 7: Promotional factors associated with long acting contraceptive use in Arada sub city, Ethiopia, 2017 (n=469).
Determinants factors with long acting contraceptive use
According to the bivariate analysis result of this study, being model family more likely to use long acting contraceptive methods compared to those women from non-mode family. The crude OR 1.862 (1.137, 3.050) showed that the women from model family were more likely to use long acting contraceptive methods than non-mode family. This association also indicated in the multivariate analysis of this study indicated by (AOR, (95% CI; 1.7 (1.0, 2.9). Regarding the marital status, bivariate analysis of this study indicates marital status had effect/association with long contraceptive utilization as indicated by (COR (95%CI); 6.3 (1.5, 26.4). After controlling the influence of other independent variable constant, marital status had also effect on the utilization of long acing contraceptive.
Based on the result of this study, the crude OR 3.65 (1.6,8.3) showed that the respondents who were education are more likely to use long acting contraceptive where as women who were higher education were less likely to use long acting contraceptive as compared to those who were no educated. Though by controlling the effect of other independent variable analyzed by logistic regression only primary education (AOR, (95% CI, 4.4 (1.9,10.4) had significant association/ effect with long acting contraceptive utilization. Concerning the type of occupation being government employee had significant relation with long acting contraceptive utilization in respect to bivariate analysis of this study, and also the multivariate analysis of this studies indicating (AOR, (95% CI, 3.1 (1.6,5.9)) had association between long acting contraceptive and being governmental employee. According to the multivariate analysis of this study health worker counseling and information given by health extension professional at home of the respondents had association or effect with long acting and permanent methods of contraceptives use which is indicated by (AOR, (95% CI, 1.9 (1.2,3.2) and 1.93 (1.2,3.2) respectively (Table 8).
| Characteristics | Prevalence (100%) | COR(95%CI) | AOR(95%CI) |
| Family type | |||
| Non-model* | 47.3 | 1 | 1 |
| Model | 52.7 | 1.9 (1.1,3.1)** | 1.7 (1.1,2.9)** |
| Age | |||
| 18-24 | 10.7 | 1 | 1 |
| 25-29 | 29.9 | 1.6 (0.8, 3.1) | 1.0 (0.4, 2.6) |
| 30-34 | 26.2 | 2.3 (1.2,4.5)** | 0.8 (0.3,2.2) |
| 35-49 | 33.3 | 2.057 (1.071,3.951)** | 1.3 (0.5, 3.4) |
| Educational status | |||
| Illiterate* | 21.3 | 1 | 1 |
| Primary education | 63.3 | 3.7 (1.6,8.3)* | 4.4 (1.9,10.4)** |
| Secondary/Higher | 15.4 | 2.7 (1.0,7.1) | 2.3 (0.8,6.9) |
| Marital status | |||
| Married | 88.5 | 6.3 (1.5,26.4)** | 4.7 (1.1,20.3)** |
| Not married* | 11.5 | 1 | 1 |
| Occupational status | |||
| Housewife * | 82.3 | 1 | 1 |
| Government employee | 7.7 | 2.3 ( 1.3,3.9)** | 3.1 (1.6,5.9)** |
| Health extension professional information at the respondents Home | |||
| Given | 46.3 | 1.8 (1.1,2.8)** | 1.9 (1.2,3.2)** |
| Not Given | 53.7 | 1 | |
| Health worker counseling | |||
| Yes | 53.7 | 1.8 (1.1,2.9)** | 1.9 (1.2,3.2)** |
| No | 46.3 | 1 | |
Table 8: Determinants of Long Acting and permanent Contraceptive use, Arada sub city, Ethiopia, 2017 (n=469).
Discussion
The majority of women 90.9% could mention at least two LAPMs and only 10.8% knew three or more methods. This result is relatively similar compared to some other studies conducted in Ethiopia. Percentage of awareness at least one long term methods is 52% [8] and also this study relatively different from the study conducted in Tigray showed 64% of married women heard about LAPMs [9]. This might be due to the difference in resident of the study participants, availability of methods in Addis in both governmental and nongovernmental institution and continuous advertisement of these contraceptives through media (TV and radio). Regarding utilization about different types of modern contraceptive methods, prominent used methods during the study were injectable in both model and non-model families. This finding has similarity in Bangladesh and Thailand the monthly injectable have been widely used in the family planning program [9]. An early evaluation of the Bangladesh family planning program stated that people liked injections better than pills, and that convenience, effectiveness, and suitability for lactating mothers were factors contributing to their popularity. In Thailand women preferred injectable because of the freedom from fear of forgetting pills, the ease, convenience, high effectiveness, and secret use possible [10]. Oral contraceptive were (23.7%), this result relatively similar with study conducted in Great Britain, the oral contraceptives’ pill was 25% of women 16-49 year were practice it [11]. In this study the prevalence of IUCD and implants were 6.6% and 10.7% respectively and permanent method was 0.4%. Long acting contraceptive like others modern contraceptive mentioned above such as injectable , pills better practiced among model families than non-model this is due to better understandings of long acting contraceptive among model families due to the information provided by health extension professional at the respondents home. In general prevalence of long acting and permanent contraceptive in the study area was 17.7%. From this 65.1% model and 34.9% non-model and the contribution of implants is 62%. This is high as compared to the study conducted in Mekele (12.3%), Jinka (7%), Butajira (5%). This might be due to difference in the study areas, access to service and information and used different levels of coverage in terms of the study population. This result also showed an implant is the predominately used method by respondents. Similar to this study other study conducted in Ethiopia showed implants is the most widely used method from LAPM contributing to almost (50%) of users in Jinka and (87%) in Mekele town [12]. Regarding female sterilization, this study showed only 0.4% of the respondents used this method. This finding similar to the study conducted in Ethiopia. It is high when compared to the research conducted in Mekele. There were no users of female sterilization in Mekelle town. However, this finding is not consistent with other studies which showed higher rates of sterilization in Jinka (36%), Butajira (10%), Caribbean (4%) and Uzbekistan (5%). About (53.7%) health worker was the prominent source of information in the study area. However this study showed some difference in the study conducted at mecha woreda (66%) health worker was the prominent source of information but in both studies health workers are the main sources of information. In this study 46.3% of respondents had information about modern contraception from health extension worker. According to EDHS 2011 contraceptive use increased with educational attainment and another study done in Guatemala, showed that more women with high school or higher education (5.2%) use IUDS than women with elementary education (1.4%) or without formal schooling (0.4%) [13]. Among women who had general knowledge about LAPMs, 49.5% had different beliefs and/or experienced/heard side effects of contraceptive, Use of implants and IUD about (83.6%) and (47.8%) respectively ,would affect their health negatively. This finding is consistent and comparable with other studies in different place only 1.5% of the married women used IUCD, which is lower as compared with a study done in Nigeria (7%) and Indonesia (52%) [14], Which might be due to the fact that large number of the women had misconception about IUCD and its side effects such as interference with sexual intercourse, cancer, delays pregnancy, restriction from working normal activity and invasion of privacy during its insertion and removal, fear of side effects, cause cancer and husband’s vaginal dryness (loss of sexual fluids) and loss of interest in sex [15,16]. In this studies large proportion of women were use contraceptives for child spacing (56.5%) than permanent limitation for number of children (43.5%). This finding is somewhat different in result with the study conducted Tigray for spacing (65%) and (17%) for limiting [17]. And some other study conducted in Nigeria the result reverse where, 30% of women contraception for child spacing versus 70% uses it for permanent limitation for number of children [18]. The major source to obtain contraceptives was a public health facility (83.8%). This finding consistent with the study conducted in Tigray (83%). Majority of the respondent (87.8%) preferred joint decision for family planning usage. This finding is consistent and comparable with other studies conducted in different parts of Ethiopia that considered the importance of involvement and joint decision of husbands for family planning usage.
Conclusion and Recommendation
This research finding indicates that, health extension professionals are the major sources of information about modern contraceptive particularly long acting methods. Factors such as being mode family, age, educational status, marital status, occupational status, age at first marriage, information given by health extension professional, health worker counseling, husband and wife education, and availability of method were associated with long acting and permanent contraceptive utilization. After adjusting the confounding factors using multivariate analysis, being model family, educational status, marital status, occupational status, health extension professional information and, health worker counseling were determinants of long acting and permanent methods in the study area. Based on the finding of this research the following recommendations are forwarded. Governmental interventions like health extension program need to be reoriented and strengthened to help people to understand the benefits, differentiate facts from myths and misconception, about long acting and permanent methods. Health extension professional should be encouraged to work on utilization of different contraceptive methods and to correct misconception about contraceptive use.
Acknowledgment
First of all I would like to thank my advisor Dr. Negussie Deyessa who’s all round support, encouragements and comments in a range of aspects of this thesis work starting from proposal development to the write up of this outcome. Moreover, I would like to express my deep appreciation to Arada Subcity health office staff for their invaluable support during data collection. Also I would like to express my thanks to ACIPH and Haramaya University for giving me the chance to conduct this thesis.
References
- Ambaw D, Mengistu A, Wilder J (2015) Service delivery-based training for long-acting family planning methods: Pathfinder international in Ethiopia. Watertown: Pathfinder International.
- Aragaw H (2014) Health extension program of Ethiopia: Summary of concepts, progress, achievements and challenges, WHO Ethiopia country office.
- Caldwell J, Orubuloye IO, Caldwell P (2015) Fertility decline in Africa: A new type of transition? population and development review 18: 211-242.
- Central Statistical Authority (2001) Ethiopian demographic health survey 2000.
- Fentahun M (2016) Comparative study of the characteristics of family planning service user and non-users in Northwest Ethiopia. Afr J Reprod Health 10: 62-70.
- Mekonnen G, Enquselassie F, Tesfaye G, Semahegn A (2014) Prevalence and factors affecting use of long acting and permanent contraceptive methods in Jinka town, Southern Ethiopia: A cross sectional study. Pan Afr Med J 18: 98.
- Minister of Health (2014) Accelerated expansion of primary healthcare coverage in Ethiopia, 2005-2009. Addis Ababa.
- Guttmacher institute (2016) World population day six reasons to support family.
- Trusell J, Vaughan B (2014) Contraceptive failure, methods-related discontinuation and resumption use: Results from the 2010 national survey of family growth. Fam Plann Perspect 3: 64-72.
- Mussie A, Tefera B, Tizta T (2012) Factors associated with utilization of long acting and permanent contraceptive methods among married women of reproductive age in Mekelle town, Tigray region, north Ethiopia. BMC Pregnancy and Childbirth 12: 6.
- Â Pathfinder international Ethiopia (2013) Family planning service in Ethiopian.
- Chigbu B, Onwere S, Aluka C, Kamanu C, Okoro O, et al. (2014) Contraceptive choices of women in rural Southeastern Nigeria. Niger J Clin Pract 13: 195-199.
- U.S. Agency for International Development (USAID) (2013) Long-acting and permanent methods: Addressing unmet need for family planning in Africa. Issue Brief. Washington, DC: USAID.
- USAID (2014) Contraceptive trends in developing countries: Comparative reports.
- USAID Health Policy Initiative (2013) The contribution of family planning, achieving MDGs in Ethiopia, Ethiopia.
- WHO Special Program of Research (1988) Development and research training in human reproduction, task force on long-acting systemic agents for fertility regulation. Contraception 37: 1-20.
- USAID (2013) Ethiopia health extension program: Pathfinder internationals support 2003-2007.
Citation: Teshome GS, Woldeyohanis FW, Deyessa N (2018) Long Acting and Permanent Contraceptive Use in Arada Sub City, Addis Ababa, Ethiopia, 2017. J Community Med Health Educ 8: 618. DOI: 10.4172/2161-0711.1000618
Copyright: © 2018 Teshome GS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 89598
- [From(publication date): 0-2018 - Dec 20, 2025]
- Breakdown by view type
- HTML page views: 88548
- PDF downloads: 1050