Long Acting Injectable versus Oral Antipsychotics in Reducing Hospitalization Outcomes in Schizophrenia: A Mirror-Image Study
Received: 01-Jan-1970 / Accepted Date: 01-Jan-1970 / Published Date: 27-Dec-2017 DOI: 10.4172/1522-4821.1000377
Abstract
Objective: The primary objective of this study was to assess the difference of hospitalization rates when switching patients with schizophrenia from oral antipsychotics to Long Acting Injectable (LAI) antipsychotic medications.
Methods: A single centre mirror image design study of 44 patients was conducted in a community centre hospital. Data surrounding hospitalization was collected 12 months before and 12 months after switching from oral to LAI.
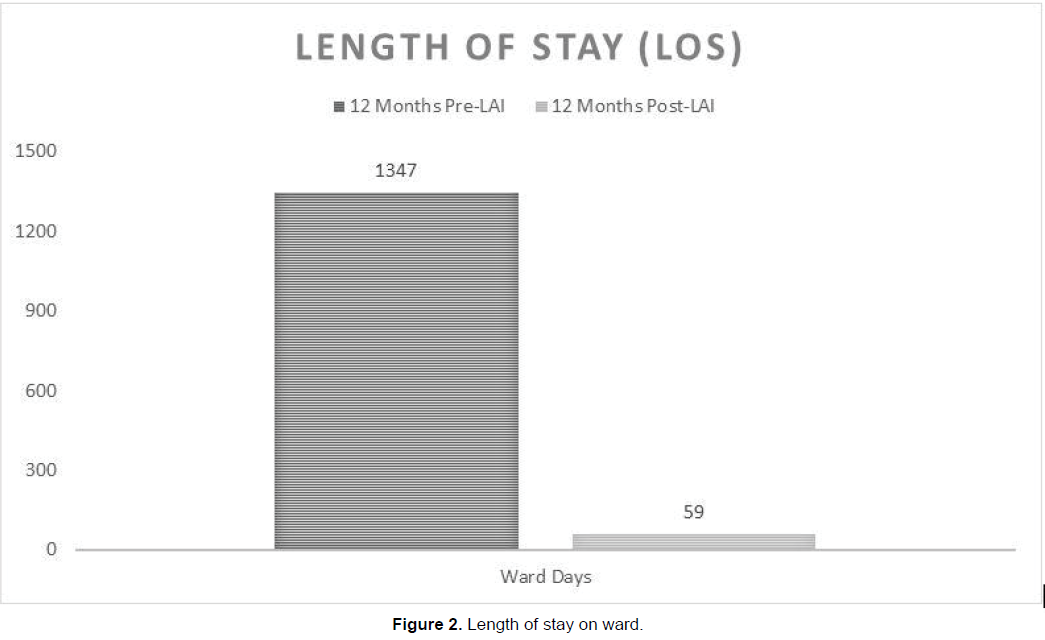
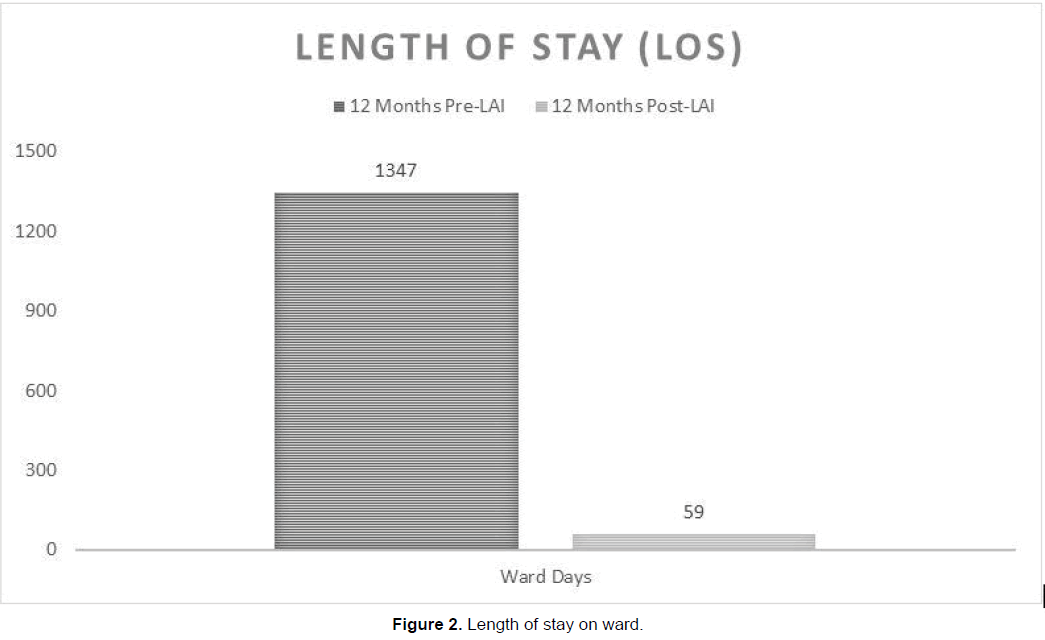
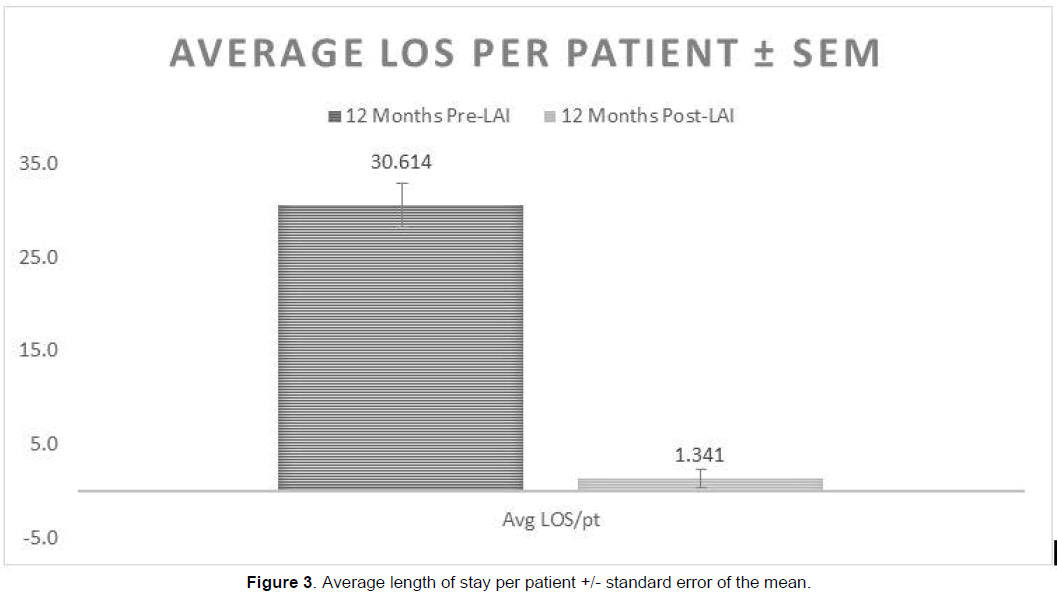
Results: There was a 91% reduction in ward admissions and an 80% reduction in ER visits when switched to LAI (p<0.001). Of the 44 patients, 32 were admitted at least once whilst on oral therapy; after switching to LAI, only 5 patients were admitted. The total number of days spent on the ward on oral therapy was 1347 days, versus 59 days on LAI. After switching to LAI from oral therapy, mean length of stay in hospital per patient decreased by 30 days (p<0.001). Cost benefit analysis showed a net savings of $805,798.80 for 44 patients over the course of one year.
Conclusions: The data from this study suggests that long acting injectable therapy is strongly superior to oral antipsychotics for the treatment of schizophrenia. A significant reduction in hospitalization rates and costs was seen.
Keywords: Long acting injectable, Schizophrenia, Hospitalization, Antipsychotics
Introduction
Schizophrenia is a serious mental illness, characterized by delusions, hallucinations, disorganized speech and behavior, and other symptoms that can cause major dysfunction. It affects approximately 1% of the Canadian population with an onset in early adulthood (Public Health Agency of Canada, 2017). It has a profound and chronic effect on an individual’s ability to function in all aspects of life-social, education, career, family, self-care, and relationships. The burden of the illness includes discrimination from others and self-stigma, including loss of hope, low self-esteem and poor quality of life (Brohan, Elgie, Sartorius, & Thornicroft, 2010). The disease also incurs significant financial cost both directly and indirectly on the health care system. The total direct cost of schizophrenia has been estimated at $2.35 billion per year, 0.3% of GDP while the indirect costs are estimated at upwards of $2 billion yearly (Goeree et al., 2005). Schizophrenia has been estimated to account for 1-3% of total healthcare expenditure (Phanthunane, Vos, Whiteford, & Bertram, 2011). Overall, 79% of the direct costs of schizophrenia result from hospitalization or other residential care (Chue, 2007).
Effective early treatment can prevent debilitating symptoms and allow patients to lead productive lives. For acute and chronic phases of schizophrenia, antipsychotic therapy is the pillar of disease and symptom management. However, lack of compliance and poor medication adherence is a major issue. Non-adherence can jeopardize disease management and lead to poor outcomes such as relapses, greater use of emergency resources, suicide attempts and greater rates of substance abuse, hospital admissions, and a decrease in quality of life. These outcomes are associated with high medical and non-medical costs, as well as productivity loss. Rehospitalization is frequently the most expensive healthcare cost component for schizophrenic patients (Lafeuille, 2013).
Long Acting Injectable (LAI) formulations of antipsychotic medications were developed to improve non-adherence and reduce relapse incidence among patients with schizophrenia. LAI treatment requires patients to visit clinics to receive treatment every 2 to 4 weeks, eliminating the need for daily oral antipsychotic administration. They provide the advantage of immediate awareness of non-adherence. If a patient misses a scheduled appointment the physicians, nurses, caregivers and family become aware. The blood levels do not decline as rapidly as oral antipsychotics giving the healthcare team a chance to intervene before an exacerbation of symptoms occurs (Kane, Kishimoto, & Correll, 2013). Comparatively in oral therapy, non-adherence is difficult to detect and it may take a severe relapse before any medical intervention occurs.
The rate of LAI use from published outpatient studies is as low at 6.3% in Canada, compared with 15% to 80% worldwide (Manchanda, 2013). In a qualitative study by Iyer et al., (2003) physicians reported the use of LAIs was a last resort for their patients. Other reasons for non-use included lack of knowledge or experience surrounding LAIs, as well as concerns about the initial costs of the medication. Although LAIs, especially the more recently-developed second-generation LAIs can be costlier than oral antipsychotics, if relapses are prevented then the long term benefits and financial burden on the health care system out-weigh the immediate cost of the new medications.
In a previous study, Koczerginski and Arshoff (2011) showed that when 25 schizophrenia patients switched from oral antipsychotic therapy to risperidone LAI (RLAI), their annual hospitalization rates decreased significantly between the 12 months before and after the switch. This decrease in hospitalization rates was also associated with an annual hospital savings of $569, 450 for the 25 patients. Since then, newer second generation LAIs such as paliperidone palmitate have become available in Canada in addition to RLAI. Although these newer formulations are more costly upon initiation compared to oral therapies, we became interested in examining whether utilization of these second generation LAIs would result in a similar cost savings in a rural community hospital setting. In our study at the Peterborough Regional Health Centre (PRHC), we hypothesized that clinically indicated initiation of LAI in outpatients with schizophrenia would reduce the total number of ER visits, ward admissions, and total length of stay in the hospital, compared to patients receiving oral antipsychotics. A reduction in the aforementioned outcomes would make the costs of investing in LAI therapy for more patients an advisable clinical decision; both for the patient’s increase in quality of life, and for the resources and direct hospital costs that are saved.
Methods
This was a retrospective mirror-image design study looking at hospitalization rates one year before and one year after initiation of LAI antipsychotics: Risperidone LAI (RLAI) and Paliperidone Palmitate Once-Monthly (PP1M) Because this was a mirror-image design, the 44 outpatients served as their own controls. Treatment decision to start LAI was made collectively by both psychiatrist and patient. Patients diagnosed with schizophrenia who initiated the use of LAI were identified at the PRHC between 2005 to 2016. The date at which LAI was initiated was defined as the index event. Each patient served as their own control for the comparison of outcomes between the baseline and follow-up time periods. The patient’s charts were examined one year before and one year after the index event.
Inclusion criteria in the study population required that patients be greater than 18 years of age at the beginning of the study, that patients have a diagnosis of schizophrenic spectrum disorder as defined by the DSM-IV and at least 12 months of continuous chart data during the baseline period, and at least 12 months of continuous chart data after initiation of LAI. The two LAIs examined in the study were PP1M and RLAI. Of the 44 patients, 22 were switched to RLAI and 22 were switched to PP1M. Patients who were switched from a first generation long acting injectable to secondgeneration LAIs were not included. Only patients who had never taken injectable therapy before were examined. Baseline patient demographics include age and gender. Patients were a minimum 18 years, maximum 63 years (Mean 34, Standard Deviation 11.3). There were 10 females and 34 males.
Following initiation of LAI therapy, patients were followed by the team nurse every 2-3 weeks, if on RLAI and every 4 weeks if on PP1M. The team nurse conducted a general health assessment and mental status examination. Testing was done for metabolic side effects and extra pyramidal symptoms. These side effects were not analyzed in this study. The psychiatrist was seen as needed. Ethical approval for this study was granted by Peterborough Regional Health Centre ethics committee.
Descriptive statistics were used to determine significant differences between Pre-LAI and Post-LAI outcomes including total ER visits, ward admissions, and length of stay. The significance of the differences among the Post-LAI and Pre-LAI cohorts was determined by a paired samples t test. A two sided alpha error of 0.05 was used to declare statistical significant. No adjustments were made for multiplicity. All statistical analyses were conducted using IBM SPSS Statistics. A cost analysis was also conducted to examine whether changes in hospitalizations pre and post switch to LAI would result in an overall annual cost saving to the hospital.
Results
Following initiation of LAI therapy, there was an 80% (p<0.001) decrease in ER visits and a 91% (p<0.001) reduction in ward admissions over the course of one year. Before the initiation of LAI 32 (73%) patients had at least one admission to the ward while on oral therapy (Figure 1). After switching to LAI, only 5 (11%) patients were admitted.
The total length of stay on wards was significantly reduced after switching to LAI. Whilst on oral therapy the length of stay on the ward was 22.8 times higher (p<0.001) than the total length of stay on LAI therapy (Figure 2). Patients on oral therapy spent a total of 1347 days on the ward. After switching to LAI the total number of ward days across one year was reduced to 59 days. On average, each patient on oral therapy spent 31 days in the ward. After substituting to LAI therapy, each patient stayed an average 1 day on the ward (Figure 3).
Cost Analysis
The cost of 50 mg of RLAI according to the Ontario Drug Benefit Formulary/Comparative Drug Index is $326.34 per unit. This LAI is required twice a month, therefore the annual cost per patient is $7,832.16. The cost of 100 mg of PP1M is $476.87 per unit, required monthly, resulting in an annual cost of $5,722.44. Comparatively, the average cost of oral antipsychotic medication is approximately $900 annually. Interviews were conducted with hospital administrative staff at PRHC to determine the cost of ward admission and ER visits; approximately $800.00/day.
LAIs are often not used due to their high cost in comparison to oral medications. However, given their enhancement of compliance and subsequent decreases in hospital admission rates several studied have showed that in the long term LAIs cause significant savings. The cost differences before and after initiation of LAI were estimated using the above numbers. Because compliance on oral antipsychotic medications was uncertain, their cost was eliminated and assigned a value of 0.
The cost in total for all 44 patients before initiation of LAI (hospital cost only) was calculated at $1,169,600.00 due to 1347 days of admission in the ward and 115 ER visits in total. The cost of the LAI for one year for all 44 patients was $298,201.20 and the total cost of ward and ER admissions was $65,600 (59 days in ward and 23 ER visits), totaling to $363,801.20. Thus, the net savings before LAI and after LAI initiation is approximately $805,798.80. This equates to savings of $18,313.60 per patient per year. This cost excludes the cost of oral antipsychotic medications, which would result in a higher number for the net savings.
Discussion
The primary purpose of this study was to assess the difference in number of hospital admissions and ER visits, and length of stay, and subsequent cost differences, in patients with Schizophrenia Spectrum Disorder (DSM 4) when comparing LAI medication versus oral antipsychotics. This is the first Canadian study to our knowledge looking at the impact of LAI use on hospitalization rates in patients with schizophrenia in a rural community centre.
Switching to LAI demonstrated a 91% reduction in yearly ward admission rates. This data is consistent with a large metaanalysis (N=5940) of 25 mirror-image studies which showed a significant difference in preventing and reducing hospitalizations when patients were switched to LAI (Kishimoto, Nitta, Borenstein, Kane, & Correll, 2013). These findings are also consistent with the
conclusions made by Koczerginski, & Arshoff (2011). Although they examined a smaller cohort of patients, they too found a significant reduction in hospitalization rates. The rate of emergency department visits was 6 times lower when patients were switched to LAI. Compared to oral therapy, the average length of stay on the ward per patient was 32 days lower during LAI treatment. They found that there was a saving of approximately $23,000/patient per year.
Our cost analysis estimated a saving of over $18,000/patient per year. Other cost benefit analysis studies have estimated to translate into overall cost savings of $4142-$7465 US for the first year of treatment of switching to RLAI (Chue, 2007). This data is only representative of direct costs to the health care system, the indirect savings of preventing relapses on a societal, individual, and caregiver level are invaluable. The benefits seem to greatly outweigh the initial cost of the injectable medications (4).
In current clinical practice, patients with schizophrenia are commonly started on oral antipsychotic medications and are only switched to an LAI agent after chronic non-adherence occurs and leads to poor outcomes. The results of this study suggest that LAI can significantly decrease the time spent in hospital and financial burden by patients diagnosed with schizophrenia who are noncompliant to oral medication and thus consideration should be given to earlier initiation of long acting injectable for preventing relapses early in the illness course.
Limitations
The first limitation of this study is the design of the study. This study is a retrospective mirror image design. There was no preceding randomization process, blinding, or parallel control group assignment (Each patient served as their own control). The spontaneous course of illness or other factors such as changes in hospital policy was not accounted for. The small sample size of this study is also noted as a limitation. However, with such significant results in all outcomes, transfer of this study design to a greater sample size is expected to largely support the evidence of this research.
Ideally, a Randomized Controlled Trial (RCT) would be the gold standard. Meta-analysis of previous RCTs examining LAI vs OAP do not show significant results (Kishimoto et al., 2012). However, the patient population selected for these trials (clinically stable and motivated for treatment) may not be representative of the patient group for whom clinicians would choose LAIs. The design of the study may also not be reflective of real world settings and may enhance adherence. Mirror image design studies may be more representative of naturalistic clinical practice and “Real World” patient population.
Patients in the study were started on LAI for different clinical indications including patient or clinical preference, lack of compliance, placement on CTO, and disease severity. These indications were not analyzed or documented in data collection, or used for stratification of results. Furthermore, during the course of this study, improvements on quality of life was not directly studied. However, the decrease in hospitalization does suggest a decrease in severe symptoms and therefore an improvement in quality of life for the patient.
The data was only collected from one hospital thus results are subjects to missing data if patients had visits at other health care facilities; however due to the rural setting of our hospital, our patients are less likely to move between hospitals as they are more likely to do in larger cities and urban centres.
Conclusion
Based on the data presented in this study, LAI antipsychotic medications are a beneficial alternative to oral antipyschotics. This study demonstrates the strong superiority of LAIs in reducing hospitalization rates and financial burden of poorly controlled schizophrenia. Clinically, our results suggest that prompt detection of patients who need support with medications and earlier initiation of LAI could prevent relapses and reduce both indirect and direct costs associated with schizophrenia. Future studies may focus on subjects of all disease severity to determine if starting LAI early in the disease process and proactively can also be beneficial. Furthermore, it may be useful to determine what type and what dose of LAIs are most effective in clinical practice.
References
- Brohan, E., Elgie, R., Sartorius, N., & Thornicroft, G. (2010). Self-stigma, empowerment and perceived discrimination among people with schizophrenia in 14 European countries: The GAMIAN-Europe study. chizophr Res, 122(1-3), 232-238. Chue, P. (2007). Long-acting risperidone injection: Efficacy, safety, and cost-effectiveness of the first long-acting atypical antipsychotic. Neuropsychiatr Dis Treat, 3(1), 13-39. Goeree, R., Farahati, F., Burke, N., Blackhouse, G., O’Reilly, D., Pyne, J., et al., (2005). The economic burden of schizophrenia in Canada in 2004. Curr Med Res Opin, 21(12), 2017-2028. Iyer, S., Banks, N., Roy, M., Tibbo, P., Williams, R., Manchanda, R., et al., (2013). A qualitative study of experiences with and perceptions regarding long-acting injectable antipsychotics: Part II-physician perspectives. Can J Psychiatry, 58(5), 23-29. Kane, J., Kishimoto, T., & Correll, C. (2013). Assessing the comparative effectiveness of long-acting injectable vs. oral antipsychotic medications in the prevention of relapse provides a case study in comparative effectiveness research in psychiatry. J Clin Epidemiol, 66(8), S37-S41. Kishimoto, T., Robenzadeh, A., Leucht, C., Leucht, S., Watanabe, K., Mimura, M., et al., (2012). Long-acting injectable vs oral antipsychotics for relapse prevention in schizophrenia: A meta-analysis of randomized trials. Schizophr Bull, 40(1), 192-213. Kishimoto, T., Nitta, M., Borenstein, M., Kane, J., & Correll, C. (2013). Long-acting injectable versus oral antipsychotics in schizophrenia. J Clin Psychiatry, 74(10), 957-965. Koczerginski, D., & Arshoff, L. (2011). Hospital resource use by patients with schizophrenia: Reduction after conversion from oral treatment to risperidone long-acting injection. Healthcare Quarterly, 14(1), 82-87. Lafeuille, M., Gravel, J., Lefebvre, P., Fastenau, J., Muser, E., Doshi, D., et al., (2013). Patterns of relapse and associated cost burden in schizophrenia patients receiving atypical antipsychotics. Value in Health, 16(3), 60. Manchanda, R., Chue, P., Malla, A., Tibbo, P., Roy, M., & Williams, R. (2013). long-acting injectable antipsychotics: Evidence of effectiveness and use. Can J Psychiatry, 58(5), 5-13. Phanthunane, P., Vos, T., Whiteford, H., & Bertram, M. (2011). Cost-effectiveness of pharmacological and psychosocial interventions for schizophrenia. Cost Eff Resour Alloc, 9(1), 6. Public Health Agency of Canada (2017). A Report on Mental Illnesses in Canada - Public Health Agency of Canada. [online] Available at: http://www.phac- aspc.gc.ca/publicat/miic-mmac/ chap_3-eng.php [Accessed 29 Jul. 2017]
Select your language of interest to view the total content in your interested language
Share This Article
Open Access Journals
Article Tools
Article Usage
- Total views: 6997
- [From(publication date): 0-2017 - Dec 10, 2025]
- Breakdown by view type
- HTML page views: 5936
- PDF downloads: 1061