Management of Subcutaneous Emphysema in Low Income Setting Eastern of DR Congo: Rare Complication of Inhalation Foreign Body Type Peanut. Case Report
Received: 18-Dec-2018 / Accepted Date: 26-Dec-2018 / Published Date: 02-Jan-2019 DOI: 10.4172/2161-119X.1000358
Abstract
A Foreign Body (FB) in airway tract remains a serious and fatal event if not managed properly in time. We present in this case report a result of management of a gross subcutaneous emphysema following inhalation of peanut at a 6 year old girl who consulted our hospital with symptomatology of pneumonia following inhalation of foreign body type peanut seven days earlier. During her hospitalization, she developed a gross subcutaneous emphysema which was managed using subclavicular subcutaneous incision for aspiration associated on antibiotics, oxygen therapy and chest physiotherapy. The condition resolved within fifteen days. Bronchoscopy remains the good approach to remove and to prevent the complications of inhalator foreign body.
Keywords: Management; subcutaneous emphysema; inhalation; foreign body; DR Congo
Introduction
Inhalation of Foreign Bodies (FBs) in airway tract remains a serious and fatal event if not managed properly in time and might be a key causer of chronic lung injuries [1,2]. It is a leading cause of sudden death in old children [3].
The most common objects that children inhaled are food, seeds, coins, balloons, hard candy and chewing gum. One-third of them are vegetables especially nuts and generally peanuts [4]. The clinic of FBs inhaled can be asymptomatic or present as acute respiratory difficulty, choking and wheeze usually in absence of fever. Subcutaneous emphysema is an unusual complication of airway’s foreign body. In the absence of suspicion of inhalation of foreign body, such complications can lead to misdiagnosis, mismanagement and delay in appropriate care, which expose to a high morbidity and mortality [5].
In this case report, we are reporting the management of a 6 year old girl with gross subcutaneous emphysema of face, neck, chest secondary to an unusual foreign body (peanut) in the airway tract.
Case Report
A 6 year old girl admitted in the pediatric department of the teaching Hospital of Catholic University of Graben with cough, fever and respiratory distress following accidently inhalation of peanut six days before his admission.
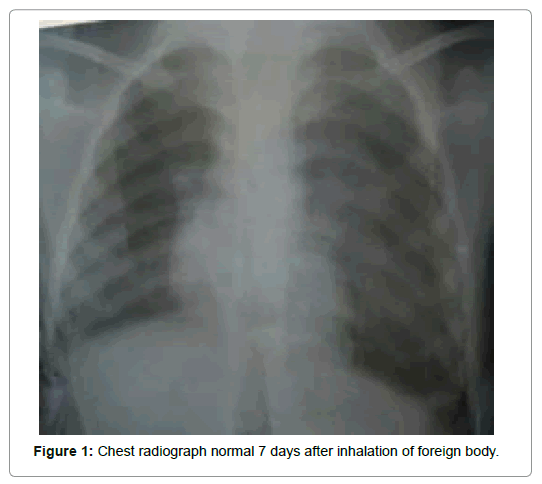
Birth history and past medical history were unremarkable. There was neither family history of asthma, atopy nor any contact with pulmonary tuberculosis. Initial AP (Anteroposterior) chest radiograph (Figure 1) revealed no abnormality. The pulmonary exam revealed crepitations in the left lung and absent breath sounds on the right side indicated a bronchopneumonia on that side. She underwent treatment of bronchopneumonia receiving Ceftriaxone 750mg, Metronidazol 750mg and Dexamethasone 4mg daily; nebulisation on Salbutamol once daily; Metronidazol 750 mg daily and oxygen therapy during one week without success. Despite this management, the child’s condition worsens and developed subcutaneous emphysema of the chest, neck and face (Figure 2). Thus the child was referred to surgery department for management.
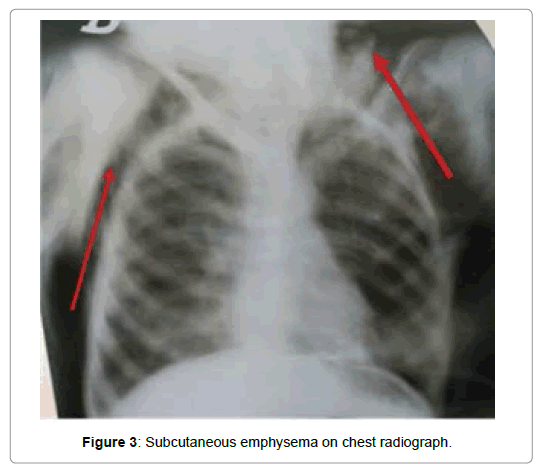
In surgery department, the child was tachypnic and tachycardia. Swelling was clinking, crepitations and crunching on palpation and tender on touch. An AP chest radiograph done, showed a huge subcutaneous emphysema affecting the face, neck and chest (Figure 3). Due to luck of bronchoscopy, the child underwent a subclavicular subcutaneous incisions for aspiration to reduce the emphysema with Tazex (association of Ceftriaxone and Tazobactam) twice 562.5 mg per day, Gentamycin 40 mg once daily and Oxygen therapy associated to the chest physiotherapy for ten days. Two weeks later patient was released from our hospital healthy (Figures 4 and 5).
Discussion
The anatomical predisposition of airway and less mature protective mechanism of children is a leading cause of high rate of complications of foreign body and the commonest age affected by those complications is a child younger than 6 years [3]. In our case report our girl describe was a 6 year old. Our patient developed a serious and dangerous pneumonia due to inhalation of vegetable foreign body type peanut. According to the literature, it is reported that One-third of foreign bodies are vegetables especially nuts and generally peanuts [4].
The clinic and the complications depend on the location of foreign body in the airway tract. It is indicated that organic substances induce more severe mucous inflammation. On the other hand, patients who aspirate small inorganic bodies tend to be asymptomatic in the long term, unless full obstruction of a terminal airway is caused [6].
Little reports in literature are known about lower airway foreign body presenting as subcutaneous surgical emphysema. Mehta and Sarin cited in their survey two authors who had reported cases children with pneumo-mediastinum and subcutaneous emphysema following foreign body aspiration [7].
Complication such as Subcutaneous emphysema is induced because of peculiar arrangement of facial planes in the neck, chest and an excessive pressure gradient at the alveolar level, facilitating extra alveolar migration of air in the subcutaneous tissue [8]. Our case, presented the foreign body located clinically in the right lung and inducing the fermentation of alveoli in the lower way of lung inducing rupture of alveoli and escaping of air along the large pulmonary vessels to the mediastinum. From there the emphysema extended to the chest, neck and scalp through the subcutaneous tissue.
We undertook a subclavicular subcutaneous incision for aspiration associated on antibiotics, oxygen and chest physiotherapy which help us to better improve the health of our patient within one week and health.
A variety of technics to manage subcutaneous emphysema have been described in case reports. O’Reilly et al. reported in their case report some technics of management of subcutaneous emphysema by using bilateral 3 cm infraclavicular incisions down to pectoralis fascia, using a trochar-type chest tube as a subcutaneous drain and using of a modified micro catheter [9].
Conclusion
Foreign body is a serious problem in low income setting due to the lack of equipment in management. The using of subclavicular subcutaneous incision for aspiration associated on antibiotics, oxygen and chest physiotherapy remains a solution to manage the subcutaneous emphysema to improve the health of children with this complications following inhalation of foreign body in low income setting. Bronchoscopy remains the good approach to remove and to prevent the complications of inhalator foreign body.
Declaration of Patient Consent
Authors certify obtained all appropriate consent from her parents. In the form the parents have given their consent for the images and other clinical information to be reported in this case report.
Financial Support and Sponsorship
None existed.
Conflicts of Interest
None existed.
Acknowledgement
The authors are thankful the entire medical staff of Teaching Hospital of Catholic University of Graben for their collaboration during the management of this patient.
References
- Dar MH, Patigaroo SA, Hussain T (2016) Foreign body inhalation in children: clinical presentations and x-ray chest fidings. Int J Med Sci Public Health 5: 2274-2278.
- Nagaraj N, Sehra RN, Berwal P, Choudhary S, Deepchand L, et al. (2017) Clinical study of foreign bodies in air passages. Indian J Child Health 4: 151-154.
- Malipatil SR, George CK, Thekkethil JS, Thottappa LH, Karadi RN, et al. (2016) Foreign bodies of tracheo-bronchial tree: A retrospective study. Int J Contemporary Med Res 3: 3202-3204.
- Aihole JS, Babu NM, Deepak J, Jadhav V (2016) Airway foreign bodies: Our six years’ experience with 301 cases. Int J Contemp Pediatr 3: 64-69.
- Tauseef U, Agha F, Ehsan S, Bukhari SI, Tauseef A, et al. (2017) Subcutaneous emphysema: A rare presentation of bronchial foreign body overlooked by paediatricians. Int J Res 4: 1096-1099.
- Gregori D, Salerni L, Scarinzi C, Morra B, Berchialla P, et al. (2008) Foreign bodies in the upper airways causing complications and requiring hospitalization in children aged 0-14 years: Results from the ESFBI study. Eur Arch Otorhinolaryngol 265: 971-978.
- Mehta AK, Sarin D (2007) Subcutaneous emphysema: An unusual presentation of foreign body bronchus. Med J Armed Forces India 63: 71-72.
- Ratageri VH, Shepur TA, Pol RR (2006) Foreign body--what is unusual? Indian J Pediatr 73: 452-453.
- O’Reilly P, Chen HK, Wiseman R (2013) Management of extensive subcutaneous emphysema with a subcutaneous drain. Respirol Case Rep 1: 28-30.
Citation: Sikakulya FK, Sivulyamwenge AK, Mbahweka FK, Masumbuko CK (2019) Management of Subcutaneous Emphysema in Low Income Setting Eastern of DR Congo: Rare Complication of Inhalation Foreign Body Type Peanut. Case Report. Otolaryngol (Sunnyvale) 9: 358. DOI: 10.4172/2161-119X.1000358
Copyright: © 2019 Sikakulya FK, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Select your language of interest to view the total content in your interested language
Share This Article
Recommended Journals
Open Access Journals
Article Tools
Article Usage
- Total views: 4229
- [From(publication date): 0-2019 - Dec 08, 2025]
- Breakdown by view type
- HTML page views: 3331
- PDF downloads: 898